Ultimate Guide to Post-Incident Recovery Metrics
Post Summary
When healthcare systems go down - like EHRs, clinical apps, or medical devices - it’s more than an IT issue. Every minute impacts patient safety and care delivery. That’s why post-incident recovery metrics are key. These metrics measure how quickly and effectively healthcare organizations recover after disruptions like cyberattacks or outages. They also help ensure compliance with laws like HIPAA by tracking recovery timelines and outcomes.
Key Takeaways:
- Time-Based Metrics: Measure recovery speed (e.g., Mean Time to Recovery - MTTR).
- Impact-Based Metrics: Assess patient safety, operational disruptions, and financial losses.
- Quality Metrics: Track the success of corrective actions and prevent repeat incidents.
Using tools like Censinet RiskOps™, healthcare organizations can centralize data, monitor vendor performance, and improve recovery processes. By combining automated tracking with actionable insights, these metrics can reduce risks, meet compliance standards, and protect patient safety.
Main Categories of Post-Incident Recovery Metrics
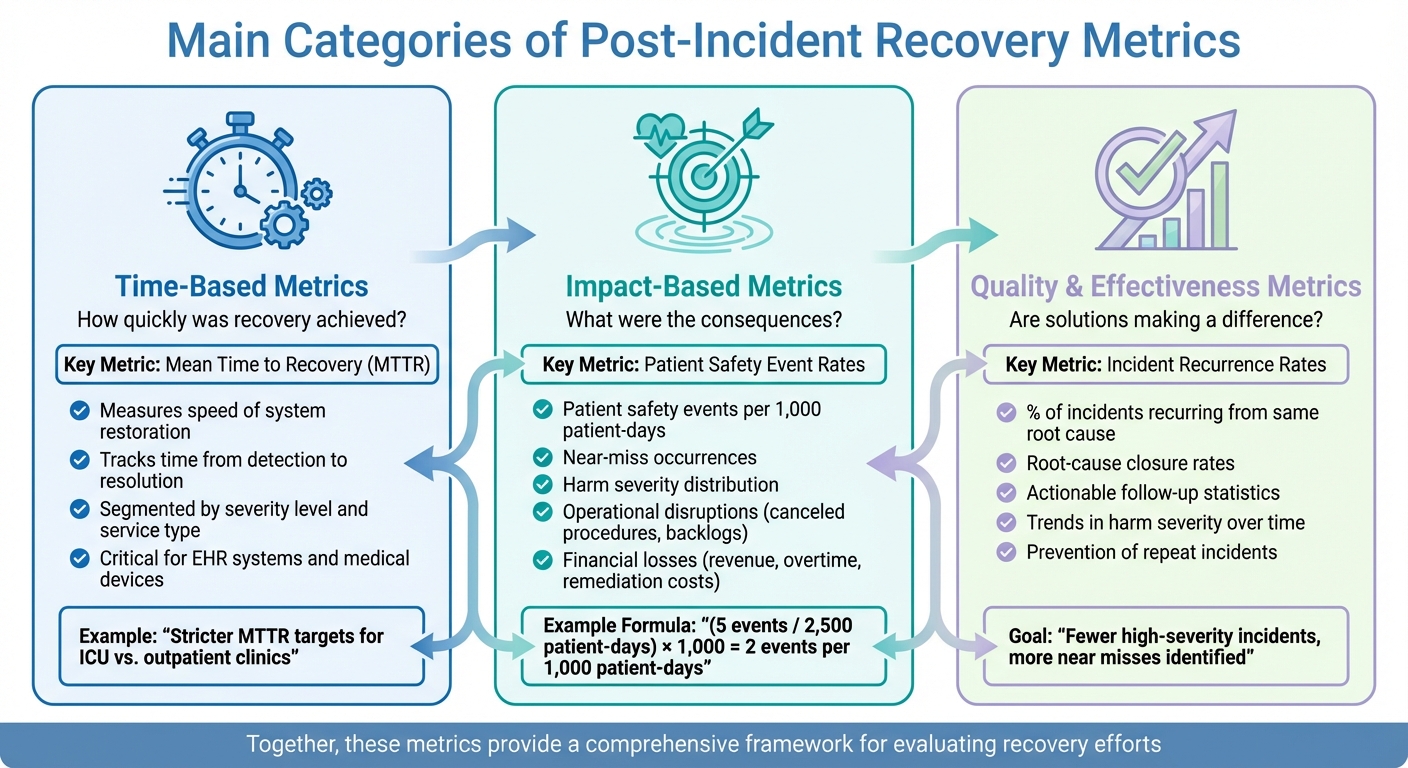
Three Categories of Post-Incident Recovery Metrics in Healthcare
Post-incident recovery metrics can be grouped into three main categories, each offering a unique perspective on how effectively a healthcare organization bounces back from incidents. These categories address key questions: How quickly was recovery achieved? What were the consequences? And are the implemented solutions making a difference? Together, they provide a comprehensive framework for evaluating recovery efforts.
Time-Based Metrics
Time-based metrics focus on how swiftly your organization can restore essential systems and services after an incident. A prime example is Mean Time to Recovery (MTTR), which measures the average time it takes to detect and resolve an issue. Similarly, healthcare providers monitor the time to resolve patient safety incidents, tracking the duration from when an event is reported to when the case is officially closed [2].
Speed is critical in healthcare. Every minute an electronic health record (EHR) system is offline or a medical device network is down disrupts clinical workflows and potentially impacts patient care. Metrics like incident recurrence rates and resolution times serve as indicators of how mature and efficient recovery processes are [7][12]. To prioritize efforts, organizations often segment these metrics by severity level or service type. For instance, stricter MTTR targets might be applied to ICU systems compared to outpatient clinics, ensuring delays are minimized where patient safety is most at risk [2][9].
Impact-Based Metrics
Impact-based metrics evaluate the fallout from incidents, focusing on patient safety, operations, and financial outcomes. Clinical impact measurements include patient safety event rates, such as the number of safety events per 1,000 patient-days, near-miss occurrences, and the distribution of harm severity (ranging from no harm to fatal outcomes) [2][9]. For example, if there are 5 safety events over 2,500 patient-days, the rate would be calculated as (5 / 2,500) × 1,000 = 2 events per 1,000 patient-days [9].
Operational impact metrics capture data like canceled procedures, diverted services, and backlogs following system restoration. Financial metrics, on the other hand, track losses such as revenue shortfalls during downtime, overtime expenses, and costs associated with remediation.
By comparing these metrics across departments and timeframes, organizations can pinpoint where recovery challenges most significantly affect patient care. Notably, metrics like incident counts and patient safety events consistently rank among the top indicators used by U.S. hospitals to monitor quality and risk [8][9][10]. These insights lay the groundwork for assessing whether recovery efforts lead to long-term improvements.
Quality and Effectiveness Metrics
Quality and effectiveness metrics measure the success of recovery actions over time and their ability to prevent repeat incidents. Key indicators include incident recurrence rates (the percentage of incidents that reoccur due to the same root cause within a set timeframe), root-cause closure rates, and actionable follow-up statistics that confirm corrective measures were not just documented but implemented [2][7][12].
Organizations also monitor trends in harm severity, aiming for fewer high-severity incidents and more near misses identified after interventions [2]. These metrics are essential for ensuring that recovery efforts lead to meaningful, lasting improvements rather than temporary fixes.
Given the complexity of healthcare, purpose-built tools like Censinet RiskOps™ enable organizations to track these metrics across their enterprise and vendor networks. This approach supports a stronger, more resilient recovery process, enhancing preparedness and reducing risk over the long term.
Core Post-Incident Recovery Metrics for Healthcare
When it comes to evaluating recovery performance in healthcare, specific metrics provide a clear picture of how well systems bounce back after disruptions. These measurements help identify gaps and guide improvements to ensure patient safety and operational stability.
Mean Time to Recovery (MTTR)
Mean Time to Recovery (MTTR) tracks the average time it takes to fully restore a system after an incident is detected. In healthcare, this metric focuses on achieving full operational recovery, not just containment [11].
Why does MTTR matter? Longer recovery times can disrupt clinical workflows, delay diagnoses, postpone procedures, and even lead to medication errors. Staff may also need to resort to inefficient manual processes. To address this, MTTR should be broken down by system criticality - such as life safety, critical clinical systems, and supporting systems - so efforts can be concentrated where downtime poses the greatest risks [2][9].
Incident dashboards that display MTTR trends by severity and service line (e.g., ICU, ED, OR) can help leadership pinpoint where recovery delays are creating significant risks to patient safety. By categorizing MTTR by system criticality and incident type (like ransomware attacks, network outages, or application failures), organizations gain sharper insights into their vulnerabilities [11][5].
Recovery Time Objective Adherence
Recovery Time Objective (RTO) sets the maximum acceptable downtime for a system before it causes clinical, operational, or financial harm. Recovery Time Actual (RTA) measures how long it actually took to recover the system during an incident or drill. RTO adherence evaluates whether the actual recovery time (RTA) meets the predefined RTO [3].
For instance, if an electronic health record (EHR) system has a 60-minute RTO but takes 2.5 hours to recover, the RTO wasn’t met, and the incident is flagged as a failure. Tracking the percentage of incidents where RTA ≤ RTO provides a clear view of whether recovery capabilities are meeting expectations [3].
RTOs should be defined through a business impact analysis (BIA) that considers clinical risks, regulatory requirements, and operational needs. For example, a medication dispensing system in the emergency department might have an RTO of 15–30 minutes, while a nonclinical HR portal could have a 24-hour RTO.
To effectively monitor RTO adherence, healthcare organizations should:
- Record RTA for every outage and compare it to the defined RTO [3].
- Track the percentage of incidents meeting RTO for critical systems.
- Analyze average and worst-case RTAs to uncover persistent gaps.
- Correlate RTO failures with patient safety incidents, canceled procedures, or financial losses [2][9].
- Use post-incident reviews to identify changes in processes, staffing, or technology that could improve recovery times [13].
Visualizing RTO adherence on executive dashboards - such as monthly adherence rates for systems like EHR, imaging, lab, and pharmacy - helps leadership assess resilience and allocate resources for infrastructure improvements and redundancy [3][4].
Third-Party SLA Recovery Performance
Healthcare organizations often rely on external vendors for critical services like EHR hosting, telehealth, supply chain management, and specialized clinical applications. Third-Party SLA Recovery Performance measures how well these vendors meet their contractual obligations for uptime, incident response, and recovery after disruptions. Since vendor performance directly impacts clinical care and compliance, this metric is essential [4][6].
When vendors fail to meet SLA commitments, it can lead to extended downtime, delayed care, and even data integrity issues. As Matt Christensen, Sr. Director GRC at Intermountain Health, explains:
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare" [1].
To manage vendor recovery performance, organizations should embed these metrics across the vendor lifecycle:
- Procurement: Assess vendor capabilities during the selection process [3][4][6].
- Contracting: Set clear, measurable SLAs for uptime, response, and recovery times. Include penalties or remediation requirements for repeated failures [3].
- Ongoing Governance: Regularly review SLA performance at IT governance and risk committees. Tools like Censinet RiskOps™ can link vendor recovery performance to broader risk data, helping organizations identify how vendor limitations contribute to missed RTOs and benchmark performance against industry standards.
Building a Recovery Metrics Framework for Healthcare
To strengthen healthcare operations, recovery metrics should be integrated with existing tools like your Business Impact Analysis (BIA), Enterprise Risk Management (ERM), incident reporting, and patient safety programs [2][8][9][5]. These metrics - spanning information sharing, governance, and resource coordination - can be embedded into daily dashboards, making them a part of routine operations [5]. Below, we’ll explore how to align metrics with risk, set actionable targets, and weave them into governance processes.
Aligning Metrics with Criticality and Risk
Start by using your BIA to categorize clinical systems, Electronic Health Record (EHR) modules, medical devices, and vendors based on their impact on patient safety, regulatory requirements, and financial risk [5]. For Tier 1 services like order entry or medication administration, aim for rapid Recovery Time Objectives (RTOs) measured in minutes, paired with strict Mean Time to Recovery (MTTR) targets [11][5]. For Tier 2 systems - such as radiology or labs - track MTTR, service completion rates, and backlog clearance. Meanwhile, Tier 3 systems, like HR and finance, require simpler metrics, such as basic MTTR and incident frequency.
To improve decision-making, map out each system’s clinical owner, BIA tier, RTO, MTTR, vendor, and dependencies in a way that aligns with your BIA’s risk framework [17]. For vendors, ensure that their recovery performance is evaluated during governance reviews. This helps identify and address vendor-related issues that could lead to missed RTOs [3].
Setting Targets and Benchmarks
Effective targets combine regulatory requirements, clinical tolerance for downtime, historical data, and external benchmarks [15][3]. By analyzing 12–24 months of incident data, you can establish baseline MTTR and set measurable goals, such as reducing Tier 1 MTTR by 20–30% within a year [14][16][3]. For high-risk systems, consider tiered RTO targets - for example, achieving minimal safe functionality within one hour and full functionality within four hours.
Normalized metrics, like incidents per 1,000 patient-days, allow you to compare performance across departments and time periods [9][2]. Tools like Censinet RiskOps™ aggregate data on risk, incidents, and vendor performance across healthcare organizations. This enables benchmarking of MTTR, RTO adherence, and vendor SLA performance against anonymized peers with similar technology stacks. As Brian Sterud, CIO at Faith Regional Health, notes:
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters" [1].
Review and adjust these targets annually or after major incidents to keep them aligned with changes in clinical risks and technology systems [3]. Feeding these benchmarks into governance processes ensures continuous improvement.
Integrating Metrics into Governance Processes
Embed recovery metrics - such as MTTR, incident severity, RTO adherence, and vendor recovery performance - into risk dashboards and executive reports. These reports, shared quarterly, should provide a clear view of resilience, including trends in outages, percentages of incidents affecting patient care, progress on RTO and SLA targets, and major remediation efforts [3][7].
Recovery metrics should also be tied to clinical outcomes and patient safety. For example, track delays in medication or diagnostics, or diversion events during downtime, and discuss these in quality and patient safety committees [17]. Use key indicators like the percentage of incidents with corrective actions and the completion rate of those actions to measure quality [2]. Trend analysis can help identify recurring issues and capacity challenges, making these metrics essential for post-incident reviews and morbidity and mortality conferences [2][5].
Censinet RiskOps™ offers dashboards and heat maps to rank vendors and internal services by recovery risk. This fosters collaboration, allowing healthcare organizations and vendors to jointly review recovery metrics, track corrective actions, and provide documentation for auditors and insurers. By shifting from static goals to dynamic, evidence-driven objectives, organizations can align their recovery planning with the broader healthcare landscape.
sbb-itb-535baee
Implementing Recovery Metrics in Healthcare Organizations
To make recovery metrics a practical tool, you need clear ownership, consistent definitions, and smooth integration with your existing systems like incident management platforms, EHRs, and risk management tools [2][11][7]. The ultimate aim is to automate data collection, use it to drive meaningful improvements after incidents, and build resilience without relying on manual reporting. This integration lays the groundwork for the automation and analysis steps discussed below.
Automating Data Collection and Reporting
Manual reporting often leads to delays and inconsistencies. Instead, connect your incident reporting tools, SIEM systems, ITSM platforms, and EHR safety modules to automatically capture key timestamps such as detection, acknowledgment, containment, and full recovery [2][11][12][7]. This automated process ensures metrics like MTTR (Mean Time to Recovery), MTTC (Mean Time to Contain), and RTO (Recovery Time Objective) adherence are fed directly into dashboards, eliminating the need for staff to manually input data.
For example, Censinet RiskOps™ streamlines this process by linking healthcare organizations to a broad network and automatically collecting recovery data. Terry Grogan, CISO at Tower Health, noted the impact of this system:
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required" [1].
Similarly, James Case, VP & CISO of Baptist Health, highlighted the benefits of automation:
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with" [1].
Role-based dashboards are essential for providing real-time insights. Clinical leaders can monitor MTTR for critical systems and assess patient safety impacts, while IT teams track incident frequency, severity, and containment times [11][7]. Executives need quarterly summaries that highlight trends in RTO adherence, vendor SLA performance, and progress on corrective actions [3][7]. Automated reporting ensures everyone has access to accurate, up-to-date information without delays.
Using Metrics in Post-Incident Reviews
With automated reporting in place, post-incident reviews turn metrics into actionable insights. These sessions rely on data such as MTTR, time to resolution, and RTO adherence to pinpoint issues like delayed vendor responses, unclear escalation procedures, or flaws in backup systems [2][11][7]. Tracking the completion of corrective actions also serves as a quality measure unique to these reviews [2].
In patient safety incidents, quick resolution is essential for maintaining clinical trust [2]. Sharing feedback with frontline teams - such as how their reporting contributed to faster recoveries or process improvements - encourages a culture of active participation. This approach rewards quick reporting and engagement in root cause analyses, ultimately enhancing both detection and recovery.
Censinet RiskOps™ supports this process by serving as a centralized hub for risk-related policies, incidents, and tasks. Its AI-powered features automatically route findings and corrective actions to the right stakeholders, ensuring accountability and continuous oversight. This "air traffic control" approach keeps everything on track and ensures no detail is overlooked [1].
Improving Resilience Through Metric Analysis
Analyzing recovery metrics over a 12–24 month period can uncover patterns that guide updates to incident response plans, vendor agreements, and risk management strategies [14][3]. For instance, if Tier 1 MTTR consistently misses targets, it’s worth investigating whether the problem lies in technology (e.g., lack of redundancy), procedures (e.g., unclear runbooks), or vendor performance (e.g., slow support).
Metrics like Third-Party SLA Recovery Performance and vendor-specific MTTR provide concrete evidence of how vendors handle stress [15][3][7]. This data can inform contract revisions, including more precise RTO and RPO commitments, clear reporting requirements during incidents, and financial penalties for missed targets [15][3]. Persistent vendor underperformance should trigger due diligence, corrective action plans, or even diversification strategies to reduce reliance on a single provider for critical services [17][18].
Censinet RiskOps™ facilitates continuous, data-driven vendor risk scoring for services involving PHI, clinical applications, or supply chain dependencies. This helps healthcare organizations make better decisions about vendor selection, contract renewals, and board-level oversight of third-party risks. Brian Sterud, CIO at Faith Regional Health, emphasized the value of benchmarking:
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters" [1].
To compare performance across departments or time periods, normalize metrics like incidents per 1,000 patient-days [9][2]. Adjust targets annually or after major incidents to reflect changes in clinical risks or technology systems [3]. These insights refine your recovery framework, ensuring it evolves alongside the broader healthcare environment.
Conclusion and Key Takeaways
Post-incident recovery metrics offer a practical and measurable way to strengthen healthcare systems. By focusing on time-based metrics like mean time to recovery (MTTR), impact-based measures such as incident severity and patient harm, and quality indicators like corrective action completion, healthcare organizations can transform recovery efforts into tangible improvements in patient safety, operational efficiency, and financial performance.
Start by identifying your most critical systems - think electronic health records (EHR), picture archiving and communication systems (PACS), clinical applications, and key third-party platforms. Assign specific metric responsibilities to leaders across IT, clinical operations, and compliance departments. Set realistic targets for metrics like MTTR and recovery time objective (RTO) based on how vital each system is, and automate data collection to reduce delays caused by manual reporting. However, tracking metrics isn’t enough; they need to actively drive decision-making, process updates, and long-term learning. Centralized platforms can play a major role in this process.
For example, Censinet RiskOps™ streamlines recovery metric management by automating data collection and enabling continuous governance. The platform provides real-time dashboards tailored for clinical leaders, IT teams, and executives, eliminating the inefficiencies of spreadsheets and manual workflows. Its automated processes ensure accountability across governance, risk, and compliance teams. Additionally, benchmarking against industry standards allows organizations to secure necessary resources and maintain leadership in critical areas.
Make post-incident recovery metrics an ongoing priority. Normalize measures like incidents per 1,000 patient-days to evaluate performance across departments and over time. Adjust targets annually or after significant incidents to address changing risks and technological advancements. Engage frontline staff by showing how their reporting and participation in root cause analyses lead to faster recoveries and visible improvements. Over time, this disciplined approach to analyzing metrics will uncover trends that refine incident response plans, vendor agreements, and risk management strategies. The result? A healthcare organization that not only weathers challenges but emerges stronger and more prepared.
FAQs
What are the key post-incident recovery metrics in healthcare organizations?
Key metrics for post-incident recovery in healthcare revolve around how swiftly and effectively critical operations are restored. These include recovery time objectives (like mean time to recovery), system uptime and availability, and incident recurrence rates - all of which provide insight into the speed and reliability of recovery efforts.
Other essential metrics focus on patient safety impact, adherence to regulatory compliance, and the cost of recovery efforts. By monitoring these factors, healthcare organizations can address both operational and financial challenges, ensuring they remain resilient while protecting patient care during and after disruptions.
What is Mean Time to Recovery (MTTR) and how does it affect patient care in healthcare?
Mean Time to Recovery (MTTR) refers to the average time it takes to get systems or services back up and running after an incident. In the healthcare world, a shorter MTTR can make a big difference by keeping critical systems available. This means faster access to medical records, diagnostic tools, and treatment resources - key components of effective patient care.
When delays are minimized, healthcare providers can operate more smoothly, reduce risks to patient safety, and ensure consistent, dependable care. Quick recovery processes also play a vital role in safeguarding sensitive patient data and maintaining trust within the healthcare system.
Why is vendor performance important for healthcare organizations during post-incident recovery?
Vendor performance is a key factor in how healthcare organizations recover after an incident. It directly impacts how quickly risks are addressed and operations return to normal. Top-notch vendors help by providing swift responses, accurate threat detection, and effective remediation, all of which are essential for reducing risks to patient safety and keeping critical services running smoothly.
Working with dependable vendors allows healthcare organizations to strengthen their security measures, protect sensitive patient information, and stay compliant with regulatory requirements - all while staying focused on delivering quality patient care.


