14 Cybersecurity Clauses for Healthcare Vendor Contracts
Post Summary
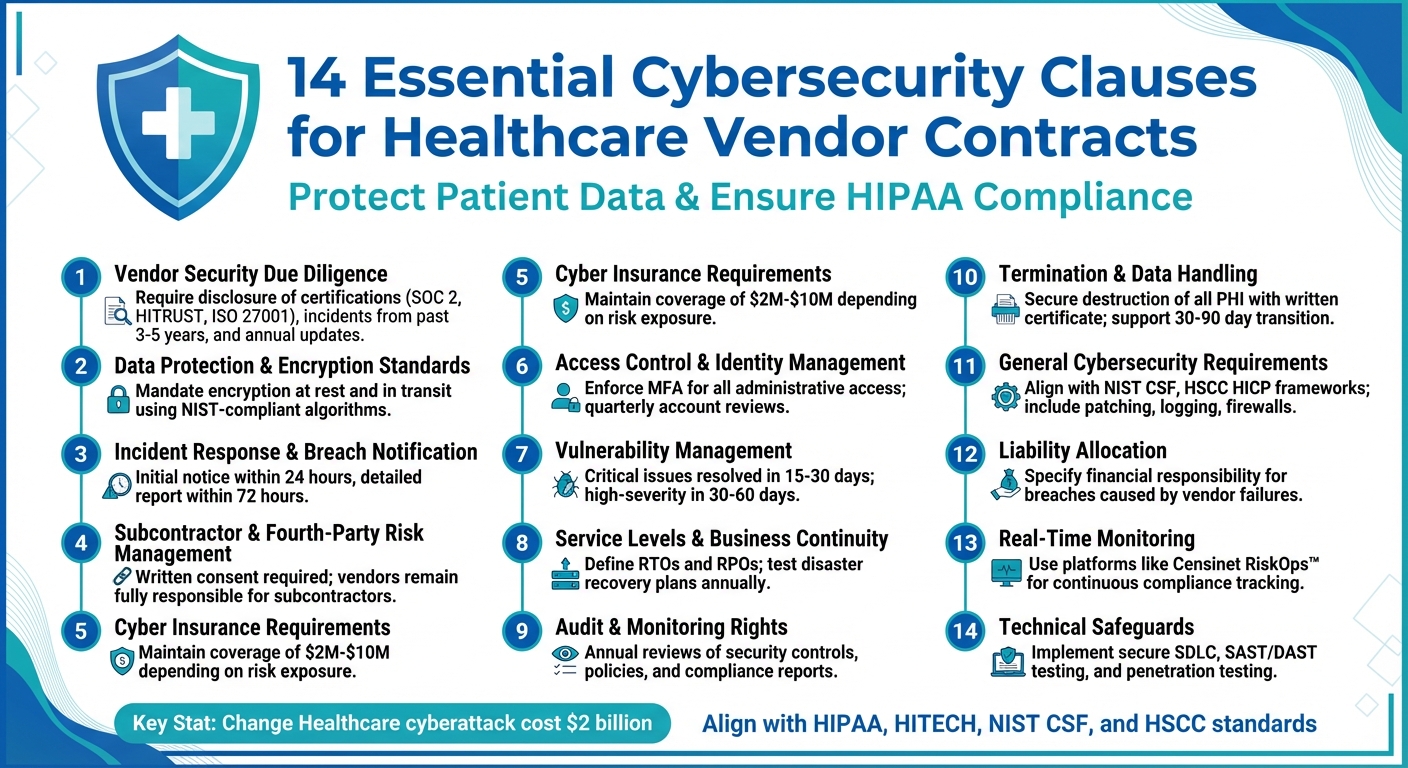
Healthcare organizations face increasing cybersecurity risks, especially from third-party vendors. Data breaches linked to vendors can disrupt patient care, violate HIPAA regulations, and result in significant financial losses, like the $2 billion Change Healthcare cyberattack. To mitigate these risks, healthcare contracts must include clear cybersecurity clauses to protect sensitive data and ensure compliance.
Key Takeaways:
- Vendors must implement strong safeguards like encryption, multi-factor authentication (MFA), and rapid breach notifications.
- Contracts should define security responsibilities, audit rights, and liability for breaches.
- Tools like Censinet RiskOps™ can streamline vendor risk assessments and compliance monitoring.
14 Essential Clauses:
- Vendor Security Disclosure: Require transparency about certifications, incidents, and audits.
- Encryption Standards: Ensure data is encrypted at rest and in transit.
- Breach Notification: Mandate incident reporting within 24–72 hours.
- Subcontractor Management: Hold vendors accountable for third-party risks.
- Cyber Insurance: Vendors must maintain adequate coverage.
- Access Control: Enforce MFA and role-based access.
- Vulnerability Management: Address critical issues within 15–30 days.
- Business Continuity: Define recovery objectives and test disaster plans.
- Audit Rights: Allow regular reviews of vendor security practices.
- Termination Protocols: Securely destroy or return data after contract ends.
- General Security Controls: Align with NIST CSF and other frameworks.
- Liability Allocation: Specify financial responsibility for breaches.
- Real-Time Monitoring: Use platforms for continuous compliance checks.
- Technical Safeguards: Include patching, logging, and secure software practices.
These clauses ensure vendors meet regulatory and security requirements, safeguarding patient data and minimizing risks. Start by reviewing your current contracts and updating them to include these provisions.
14 Essential Cybersecurity Clauses for Healthcare Vendor Contracts
Legal and Industry Requirements for Healthcare Cybersecurity
Understanding the legal landscape and industry standards is a crucial first step in drafting effective cybersecurity clauses for vendor contracts.
Primary Regulatory Requirements
In the U.S., HIPAA sets the standard for vendor cybersecurity. Its Privacy Rule, Security Rule, and Breach Notification Rule apply to business associates - vendors handling protected health information (PHI) on behalf of covered entities [5]. The Security Rule specifically mandates administrative, physical, and technical safeguards to protect electronic PHI (ePHI). These requirements are reflected in Business Associate Agreements (BAAs) that healthcare organizations sign with their vendors [5].
Recent enforcement trends have shifted contracts from broad legal language to more detailed technical safeguards. For instance, while the Breach Notification Rule requires vendors to notify covered entities of incidents within 60 days, many contracts now call for tighter timeframes, such as 24–72 hours, to align with best practices [2][4][7].
State laws add complexity. All 50 states and the District of Columbia have data breach notification laws, many of which include health or insurance data. Some states require notifications within as little as 30 days, making it essential for contracts to demand quick incident reporting from vendors. This ensures healthcare organizations can comply with applicable state rules [9]. Additionally, privacy laws like California’s Consumer Privacy Act impact vendors handling non-HIPAA data, such as wellness apps or marketing platforms. These laws require contract clauses that prohibit unauthorized data sales and ensure vendors assist with consumer rights requests [3].
These legal requirements form the foundation for industry frameworks that help refine contract terms.
Industry Standards and Guidelines
Building on regulatory mandates, industry frameworks provide actionable guidance for drafting vendor contracts. For example, the Health Sector Coordinating Council (HSCC) Model Contract Language for Medtech Cybersecurity (MC2) offers a detailed structure for defining performance, maturity, and design standards. It outlines key areas like audit and logging, intrusion detection, encryption, access management, patch management, remote access controls, and incident response - all of which can be directly included in contracts [5].
The Health Industry Cybersecurity Practices (HICP) serves as a benchmark for identifying essential security controls, while the NIST Cybersecurity Framework (CSF) organizes security requirements around five core functions: Identify, Protect, Detect, Respond, and Recover [8]. Indiana’s statewide healthcare vendor management guidance encourages referencing NIST CSF, HICP, and HSCC model language when drafting BAAs and vendor contracts [8].
The Healthcare Supply Chain Association (HSCA) provides specific recommendations for medical device suppliers. These include timely vulnerability updates, documentation such as MDS2 forms, participation in information-sharing organizations, and liability clauses. These resources streamline contract drafting by offering vetted language, ensuring consistency across vendor agreements, and addressing cyber risks that regulators consider critical to healthcare delivery organizations [5][6][8].
Third-Party Risk Management Platforms
With so many vendors to manage, manually overseeing cybersecurity requirements isn’t feasible. Platforms like Censinet RiskOps™ simplify this process by providing standardized, repeatable vendor risk assessments aligned with frameworks like HIPAA, HICP, and HSCC model language [5]. These tools include tailored questionnaires and workflows for evidence collection, enabling healthcare organizations to evaluate a vendor’s security measures before signing contracts.
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare." - Matt Christensen, Sr. Director GRC, Intermountain Health [1]
Censinet RiskOps connects over 50,000 vendors and products through a collaborative risk network, allowing organizations to share and benchmark security assessments instead of duplicating efforts [1]. The platform centralizes documentation, monitors compliance, and automates security tracking, reducing administrative burdens. One health system reported that using Censinet RiskOps freed up three full-time employees to return to their primary roles while enabling more risk assessments with only two dedicated staff members [1]. This efficiency allows security teams to focus on analyzing risks rather than managing spreadsheets.
14 Required Cybersecurity Clauses for Vendor Contracts
In healthcare, vendor contracts have become more than just legal agreements - they now serve as enforceable frameworks for cybersecurity. For vendors handling Protected Health Information (PHI) under HIPAA business associate agreements, these contracts establish specific security standards that safeguard patient data while minimizing organizational risk. The following clauses are drawn from established frameworks and legal guidance to set clear, enforceable security controls in healthcare IT contracts.
Each clause is designed to directly address HIPAA/HITECH requirements and align with industry standards like NIST CSF. Instead of relying on vague assurances, these clauses demand measurable commitments. For instance, a vendor might be required to "encrypt PHI in transit and at rest using NIST-compliant standards" and provide annual written proof of compliance. This approach transforms contracts into actionable tools for managing vendor risks from start to finish.
1. Vendor Security Due Diligence
Vendors must fully disclose their security practices, including any incidents from the past 3–5 years, current certifications (like SOC 2, HITRUST, or ISO 27001), and any ongoing regulatory investigations. They should also reveal whether they share or sell data with third parties and under what legal basis.
Contracts should require vendors to update this information annually and notify the healthcare organization of any significant changes, such as losing a certification or making major system updates. Supporting documentation - such as SOC 2 or HITRUST reports, penetration test summaries, and business continuity plans - should be provided. For higher-risk vendors, the contract might mandate independent SOC 2 Type II or HITRUST assessments at set intervals to ensure ongoing compliance.
2. Data Protection and Encryption Standards
Contracts must enforce strict encryption controls. PHI and other sensitive data should be encrypted both in transit and at rest using industry-standard algorithms. Key management practices should follow industry norms, with role-based access controls and audit logs maintained for security-related events.
In cloud or multi-tenant environments, the agreement should require data segregation and documented data flows that meet U.S. regulatory expectations. The healthcare organization should have the right to review encryption configurations, key management processes, and independent security assessments. Vendors must also provide written certification confirming encryption compliance after any significant system changes. These requirements should align with current best practices, such as those outlined in the HSCC Health Industry Cybersecurity Practices and NIST guidelines, covering anti-malware measures, logging, and patching.
3. Incident Response and Breach Notification
Contracts should clearly define a "security incident" (any unauthorized access, use, or modification of information) and distinguish it from a "breach" of unsecured PHI, which requires legal notification under HIPAA/HITECH.
Vendors must follow a tiered notification process: initial notice within 24 hours and a detailed report within 72 hours. The report should include the scope of the incident, affected data types, compromised systems, and immediate containment actions. While HIPAA allows up to 60 days for breach notification, many state laws and best practices call for much faster timelines, sometimes as short as 30 days.
Vendors must fully cooperate with forensic investigations, provide reports, and implement corrective actions within agreed timeframes. They should also cover all reasonable costs tied to breach notification, credit monitoring, regulatory defense, and fines if the breach results from their failure to meet contractual obligations.
4. Subcontractor and Fourth-Party Risk Management
Many vendors rely on subcontractors for services involving PHI or critical systems, which can introduce additional risks. Contracts should require vendors to obtain written consent from the healthcare organization before involving subcontractors who will access PHI or critical systems.
Subcontractors must sign agreements that impose the same security, privacy, and audit obligations as the primary contract. Vendors remain fully responsible for their subcontractors' actions. For high-risk services, such as hosting electronic health records, the contract might require subcontractors to hold specific certifications or participate in incident response testing. Vendors should also notify the healthcare organization of any changes to their subcontractor list and assist with necessary risk assessments.
5. Cyber Insurance Requirements
Cyber insurance provides financial protection when security measures fail. Contracts should require vendors to maintain policies with coverage limits that reflect the potential exposure of PHI. Vendors must provide proof of coverage at the start of the contract and during renewals, and notify the healthcare organization of any changes.
Policies should cover network security liability, privacy liability, media liability, data restoration, business interruption, regulatory investigations, fines (where insurable), and costs related to notification or credit monitoring. Coverage terms should not exclude failures to meet the "industry standard" controls outlined in the contract. For critical vendors, higher coverage limits or excess policies might be necessary, and healthcare organizations should periodically reassess these limits as breach costs and regulatory penalties evolve.
Technical and Operational Security Requirements
Contracts in the healthcare sector must go beyond legal terms and insurance policies to outline the specific technical measures vendors are expected to follow. These details turn general promises into actionable steps, like requiring multi-factor authentication (MFA) for administrators or addressing critical vulnerabilities within a set timeframe, typically 15–30 days. A key resource for these requirements is the HSCC Model Contract Language for Medtech Cybersecurity (MC2), which offers guidance on areas like access management, network security, data protection, logging, and patching. These technical controls bring cybersecurity promises to life in vendor agreements, ensuring compliance with both legal and industry standards.
Healthcare organizations increasingly rely on platforms like Censinet RiskOps™ to monitor these technical requirements continuously. Instead of relying solely on annual attestations, these platforms provide real-time oversight of vendor controls - covering areas like access management, patch schedules, and disaster recovery testing. This approach ensures ongoing compliance across clinical applications, medical devices, and supply chain partners. The following sections outline the specific technical measures that help maintain strong cybersecurity practices.
6. Access Control and Identity Management
Contracts should mandate MFA for all administrative and remote access to systems containing protected health information (PHI). Preferred methods include app-based one-time passwords, FIDO2, or hardware tokens, while SMS-only authentication should be avoided in high-risk scenarios. Role-based access control (RBAC) is essential, with clearly defined roles and formal workflows for access changes.
User account management is equally important. Vendors should document user provisioning processes, conduct quarterly reviews of accounts with PHI access, and deactivate accounts within 24 hours when employees leave or change roles. For remote vendor support, contracts should require secure VPN access with MFA, pre-approved access windows, detailed session logging, and real-time monitoring capabilities to terminate sessions if needed.
Privileged access deserves special attention. Vendors should implement just-in-time access elevation, use dedicated administrator accounts, and maintain session logs. Where possible, privileged access management (PAM) tools should be used, and shared administrative credentials should only be allowed under strict, documented "break-glass" procedures. Centralized logging of all authentication events - such as successful logins, failed attempts, and privilege escalations - should be required, along with integration with the organization’s identity platforms (e.g., SSO/SAML or SCIM) for better monitoring and correlation.
7. Vulnerability Management and Secure Development
Strong access controls must be complemented by rigorous vulnerability management and secure development practices. Vendors should maintain a documented vulnerability management program, performing monthly internal and external scans as well as post-change scans. Contracts must set clear timelines for addressing vulnerabilities based on their severity: critical issues within 15–30 days, high-severity issues within 30–60 days, and medium-severity issues within 90 days. For medical devices, these timelines should align with safety considerations outlined in HSCC and FDA guidance.
When immediate patching isn't possible due to potential disruptions to clinical workflows, vendors must apply compensating controls like network segmentation, enhanced monitoring, or access restrictions. They should also document any remaining risks for the healthcare organization to review and accept.
For software and SaaS providers, contracts should require a secure software development lifecycle (SSDLC). This includes incorporating security from the design phase, conducting threat modeling for PHI-related features, adhering to secure coding standards, and providing mandatory annual security training for developers. Additional measures include static and dynamic code analysis (SAST/DAST), managing third-party components with a software bill of materials and dependency scanning, and regular penetration testing by independent experts. Vendors should avoid hard-coded credentials, enforce secure defaults (e.g., encryption enabled by default), and maintain detailed change management records for any updates that impact security or compliance.
8. Service Levels and Business Continuity
Service Level Agreements (SLAs) should specify performance metrics, such as 99.9% uptime for critical applications, along with methods for measuring compliance, maintenance schedules, and penalties for failing to meet these standards. Business continuity plans must include well-defined recovery time objectives (RTOs) and recovery point objectives (RPOs) tailored to clinical risks. For example, core electronic health record systems might require an RTO of four hours or less and an RPO of 15 minutes or less. These targets should be validated through regular testing.
Vendors must maintain encrypted backups that are tested regularly and stored offsite or in geographically redundant locations. Contracts should specify backup frequency and retention policies that align with the healthcare organization’s needs and regulatory requirements. Vendors should also demonstrate successful restore tests at least once a year. For cloud and managed services, contracts should detail how infrastructure resilience - such as multi-region deployments and failover mechanisms - supports RTO and RPO targets. Vendors should also share performance and outage data with the organization.
Disaster recovery plans should address scenarios like ransomware attacks, data corruption, and service outages. These plans must include clear roles, communication protocols, and escalation paths. Vendors should participate in periodic joint disaster recovery exercises, such as tabletop drills or technical failover tests, to ensure that failover procedures work as intended and that RTO and RPO goals are met. Critical clinical workflows - like e-prescribing, imaging, and lab results - should either continue uninterrupted or have safe contingency measures in place during an incident. For essential cloud and SaaS services, vendors need to outline their failover architecture, prioritize restoring PHI access and clinical capabilities, and commit to timely communication and updates during extended outages.
sbb-itb-535baee
Compliance Monitoring and Contract Termination
Ensuring compliance with technical and operational security clauses isn’t just about having controls in place - it’s about making sure they’re working. This is where robust compliance monitoring becomes essential. Healthcare organizations must include clear audit and monitoring rights in every vendor contract. These shouldn’t be vague commitments to cooperate but explicit rights to review key documents like security policies, training records, penetration test results, and independent assessments (e.g., SOC 2, HITRUST, or ISO 27001 reports) on a set schedule. Contracts should also require vendors to stay compliant with HIPAA, the HIPAA Security Rule, and relevant state privacy laws throughout the partnership. Prompt notification of any investigations or significant noncompliance is equally critical. A lack of oversight, as seen in incidents like the Change Healthcare ransomware attack, can lead to serious financial and operational risks.
Tools like Censinet RiskOps™ help healthcare organizations go beyond annual compliance checks by enabling continuous monitoring. Unlike yearly audits, continuous monitoring provides real-time insights into vendor compliance. Through a collaborative risk network, vendors can share security questionnaires, supporting evidence, and compliance updates. This approach ensures ongoing visibility into vendor security practices, highlights gaps before they escalate into major issues, and aligns vendor performance with industry standards. By bridging technical controls with active oversight, organizations can manage risks in real time.
9. Audit and Monitoring Rights
To make oversight effective, contracts need to establish specific audit and monitoring rights. These rights should allow healthcare organizations to review vendor security controls, policies, and procedures either annually or upon reasonable request. Vendors should provide access to documents such as SOC 2 reports, penetration test results, vulnerability scans, and relevant certifications. Additionally, healthcare organizations should retain the right to conduct their own audits - whether remotely or onsite - with reasonable notice. The Health Sector Coordinating Council’s Model Contract Language for Medtech Cybersecurity (MC2) offers detailed clauses that can be directly integrated into vendor agreements to streamline negotiations and clarify expectations.
Vendors should also commit to providing regular security reports, ideally quarterly or annually, covering areas like access management, patch status, and incident summaries. For any critical gaps identified, vendors must submit remediation plans within 15–30 days. These reports allow healthcare organizations to maintain oversight without creating unnecessary administrative burdens. If a vendor demonstrates repeated or significant failures, the contract should allow for termination for cause.
10. Termination and Data Handling
When a contract ends, vendors must handle patient data with the same level of security as during the partnership. Termination clauses should require vendors to securely destroy all protected health information (PHI), including backups, logs, and archived data. If legal requirements mandate retaining certain data, vendors must continue to protect it under contract-like obligations. A written certificate of destruction, confirming permanent deletion using industry-standard methods, should be provided.
In cases where the healthcare organization needs data returned, contracts should define the format, encryption standards, and timeline for secure transfer. Additionally, vendors must support operations during the offboarding process, typically for 30–90 days. This includes providing secure access to data and technical documentation to ensure clinical systems remain operational. For critical systems, joint transition planning between the vendor and healthcare organization is essential to avoid disruptions to patient care and data security.
11. General Cybersecurity Requirements
Contracts should include baseline cybersecurity requirements tied to established frameworks like NIST CSF, HSCC HICP, or JSP2. Key measures should cover access control, regular patching, logging and monitoring, encryption for data at rest and in transit, routine backups, firewall protection, and timely security updates.
Given the evolving nature of cybersecurity standards, these clauses should be written with flexibility. For instance, contracts can specify that vendors must adhere to the latest NIST CSF and HICP standards. This ensures requirements remain aligned with industry best practices without the need for constant contract updates. This flexibility is particularly important in light of HIPAA Security Rule updates, which provide covered entities one year plus 60 days to revise business associate agreements after a rule is finalized.
Finally, the general cybersecurity clause should address liability, indemnification, and cyber insurance requirements. Vendors should carry adequate insurance coverage - typically between $2 million and $10 million, depending on the level of risk exposure - and name the healthcare organization as an additional insured party. This ensures financial protection in the event of a breach or other security incident.
Conclusion
Cybersecurity clauses play a crucial role in safeguarding patient data and maintaining the integrity of clinical operations in U.S. healthcare. Each vendor relationship introduces potential risks to Protected Health Information (PHI) and care environments. High-profile incidents, like the Change Healthcare cyberattack, highlight the severe financial and operational fallout that can occur when third-party risks aren't properly addressed through contracts. By incorporating the 14 clauses discussed in this article into vendor agreements and business associate agreements (BAAs), healthcare organizations can establish clear expectations around critical areas such as encryption, incident notification, audit rights, liability allocation, and cyber insurance.
These clauses do more than just ensure compliance - they strengthen operational resilience. By aligning with HIPAA, HITECH, and other regulatory standards, they promote technical safeguards and continuous monitoring. Tools like the Health Sector Coordinating Council's Model Contract for Medtech Cybersecurity (MC2 v.2) are paving the way for an industry standard, simplifying negotiations and ensuring consistent protections across multiple vendors. Additionally, the updated HIPAA Security Rule provides a one year plus 60 days timeline[2] for organizations to revise existing BAAs, offering a clear opportunity to review and improve vendor contracts. Strong cybersecurity clauses also help protect clinical operations, reducing the risk of vendor-related cyberattacks or outages that could disrupt care or compromise patient safety.
To make these clauses actionable, use them as a checklist for procurement, legal, IT, security, and compliance teams to integrate into RFPs, contract templates, and renewal processes. Adjust the requirements based on vendor risk - implementing stricter controls for vendors managing PHI or critical systems, while applying lighter but consistent protections for lower-risk services. Platforms like Censinet RiskOps™ can streamline this process by centralizing third-party risk assessments, monitoring vendor compliance, benchmarking cybersecurity readiness, and facilitating collaborative remediation efforts. These tools not only enhance efficiency but also empower organizations to manage vendor risks more effectively.
Start by reviewing your current vendor contracts and BAAs to identify gaps in the 14 key clause areas, focusing first on vendors handling PHI and critical systems. Update contract templates to include these clauses, ensuring stronger security terms for all new and renewed agreements. Establish a collaborative review process involving legal, compliance, security, privacy, and procurement teams to assess exceptions and weigh risk tradeoffs before finalizing agreements. Strengthen your third-party risk management program to maintain ongoing visibility into vendor security practices and clause adherence. Finally, schedule regular reassessments - at least annually - for high-risk vendors to confirm that contractual obligations are being met and remain effective.
FAQs
What key cybersecurity clauses should healthcare organizations include in vendor contracts?
Healthcare organizations must prioritize cybersecurity clauses in their vendor contracts to safeguard patient data and meet regulatory requirements. These clauses should address several key areas:
- Data protection and encryption: Ensure sensitive information is securely stored and transmitted.
- Incident response and breach notification: Define clear steps and timelines for addressing security breaches.
- Access controls and user authentication: Limit access to authorized personnel only.
- Regular risk assessments and audits: Identify potential vulnerabilities and address them proactively.
- Compliance with HIPAA and other regulations: Ensure vendors adhere to all applicable legal standards.
By including these provisions, organizations can better protect patient information while holding vendors accountable for maintaining robust security practices.
What steps can healthcare organizations take to ensure vendors meet cybersecurity requirements?
Healthcare organizations can strengthen their cybersecurity posture by embedding well-defined and enforceable cybersecurity clauses into vendor contracts. These clauses should clearly specify security expectations, compliance requirements, and detailed protocols to protect sensitive patient data.
Beyond contractual measures, performing thorough risk assessments before engaging with vendors is essential. Regular audits can further help uncover and mitigate potential vulnerabilities. Tools like Censinet RiskOps™ offer a practical solution for simplifying the management of third-party risks, ensuring ongoing compliance and fostering effective partnerships with vendors.
Why is it essential to include rapid breach notification in healthcare vendor contracts?
Rapid breach notification plays a crucial role in healthcare vendor contracts. It enables organizations to respond promptly to security incidents, minimizing the risk of exposing sensitive patient information. This quick action is essential for meeting regulatory requirements, such as HIPAA, which demands immediate measures to protect patient privacy.
When healthcare organizations act swiftly, they can better protect patient safety, reduce the chances of legal or financial repercussions, and uphold trust with both patients and stakeholders. Clearly defining breach notification terms in vendor agreements is a smart way to strengthen the protection of critical data.


