Healthcare Predictive Analytics Vendor Risk: Data Quality and Model Reliability
Post Summary
Predictive analytics in healthcare can improve patient outcomes and lower costs, but relying on third-party vendors introduces risks. The two biggest concerns are data quality and model reliability. Poor data - like incomplete records or biased datasets - can lead to flawed predictions, while unreliable models might perpetuate inequities or fail to adapt to changing patient needs.
Key takeaways:
- Data Quality Issues: Unstructured and fragmented data, inconsistent coding, and bias in datasets can lead to inaccurate predictions.
- Model Reliability Problems: Vendors often use "black box" algorithms with limited transparency and insufficient bias testing, risking errors and inequities in patient care.
- Vendor Risk Management: Healthcare organizations must evaluate vendor practices, including data validation, bias testing, and model governance, while maintaining continuous oversight.
Data Quality Risks in Predictive Analytics Vendors
Frequent Data Quality Problems
Did you know that 80% of electronic healthcare data is unstructured? This includes things like clinical notes and imaging reports, which hold valuable insights but are tough for predictive analytics to process effectively [6][9]. When vendors build predictive models using this kind of data, several challenges crop up. For instance, incomplete records and inconsistent coding across healthcare facilities - such as missing lab results, incomplete medication histories, or varying diagnosis codes - can lead to inaccurate outputs.
Another common issue is data fragmentation. Healthcare data often comes from multiple sources, like electronic health records, insurance claims, lab systems, and wearable devices. These systems rarely integrate smoothly, leading to duplicates, conflicting information, or outdated records. Without proper reconciliation, vendors risk working with messy, unreliable data. In fact, poor data quality has been called an "epidemic" in healthcare, significantly hampering disease prevention efforts [6].
These data quality issues aren't just technical problems - they directly affect patient care, as explored in the next section.
How Poor Data Quality Affects Patient Care
When predictive models are built on flawed data, the results can be disastrous for patient care. Unreliable predictions might lead to misdiagnoses, medication errors, or ineffective treatments [7][8]. Imagine a scenario where a model trained on incomplete data fails to identify a patient at risk for septic shock. Missing this critical window for intervention could have life-threatening consequences.
Bias in the data adds another layer of concern. For example, research has shown that some diagnostic models unfairly disadvantage certain groups. One study revealed that Black patients often had to exhibit worse kidney function than White patients to qualify for the same treatments, highlighting how biased training data can skew results [9].
Additionally, when vendor datasets underrepresent minority populations or low-income communities, the models tend to perform poorly for these groups. This not only reduces prediction accuracy but also reinforces existing healthcare disparities.
How to Evaluate Vendor Data Practices
To tackle these data quality challenges, healthcare organizations need to take a hard look at vendor data practices before signing any contracts. Start by asking vendors to clearly document their data sources. If a vendor can't explain where their data comes from, how it's collected, or how often it's updated, consider it a red flag. Prioritize vendors who use standardized data entry protocols and conduct regular audits to catch errors early [8].
Another key area to evaluate is the vendor's validation processes. Ask how they verify data accuracy, handle missing information, and reconcile discrepancies across sources. Reliable vendors often use anomaly detection systems to identify outliers or unusual patterns that could signal data quality issues [8]. They should also have strong methods for working with unstructured data - like clinical notes and imaging reports - ensuring they extract insights from all available information [6][9].
Finally, pay attention to how vendors manage data integration across multiple systems. Request detailed documentation on their approach to unifying data streams and maintaining consistency [5][3]. Vendors should also demonstrate a commitment to ongoing staff training and uphold stringent data governance practices to ensure quality [8].
Carefully evaluating these practices is an essential step in managing vendor risks effectively.
Model Reliability Risks: Bias, Validation, and Governance
When it comes to maintaining trust and ensuring patient safety, the reliability of predictive models is just as important as the quality of the data they rely on.
What Makes a Predictive Model Reliable
For a predictive model to be considered reliable, it must undergo thorough validation, continuous calibration, and rigorous bias testing. Validation involves testing the model on new data sets to confirm it performs well across various patient groups. Calibration ensures the model's predictions align with outcomes observed in real-world scenarios over time. This is especially critical in healthcare, where patient demographics, treatment protocols, and conditions can change rapidly. To keep up, performance monitoring must be an ongoing process. Vendors should regularly audit for performance drift to ensure accuracy and fairness. These practices, building on earlier efforts to ensure data quality, are key to strengthening vendor risk management [1].
Typical Vendor Model Weaknesses
Beyond validation, transparency is a common challenge for many vendors. Some rely on "black box" systems, where the decision-making processes are hidden, eroding trust among clinicians. Another frequent issue is insufficient bias testing. As Deloitte highlights:
Algorithms behind computer processes are known to be biased unless very clear risk controls and assurance processes are actively engaged and addressed. Computer systems reflect the implicit values of the people coding and training them. [2]
When models are developed using data that fail to represent diverse patient populations, there’s a risk they’ll work well for certain groups but fall short for others. Additionally, limited external validation - where models are tested only with internal data - can obscure flaws that might emerge in real-world clinical environments.
How to Assess Vendor Model Governance
Evaluating a vendor’s model governance starts with reviewing their model logic documentation. Vendors should clearly explain how their models work and outline the risk controls in place. If they can't, it might signal deeper issues [2]. Robust version control is another critical element - vendors should maintain detailed records of model updates, changes in training data, and performance metrics over time.
A human-in-the-loop approach is also essential, as it allows clinicians to complement machine-generated recommendations with their expertise. Clear guidelines should specify when clinicians can override the model’s suggestions, ensuring accountability remains shared between human and machine decisions [2]. Lastly, look for evidence of a multidisciplinary review process. Effective governance often involves collaboration among clinical, technical, and ethical experts to ensure the model is reliable, fair, and aligned with patient care goals.
sbb-itb-535baee
How to Manage Predictive Analytics Vendor Risks
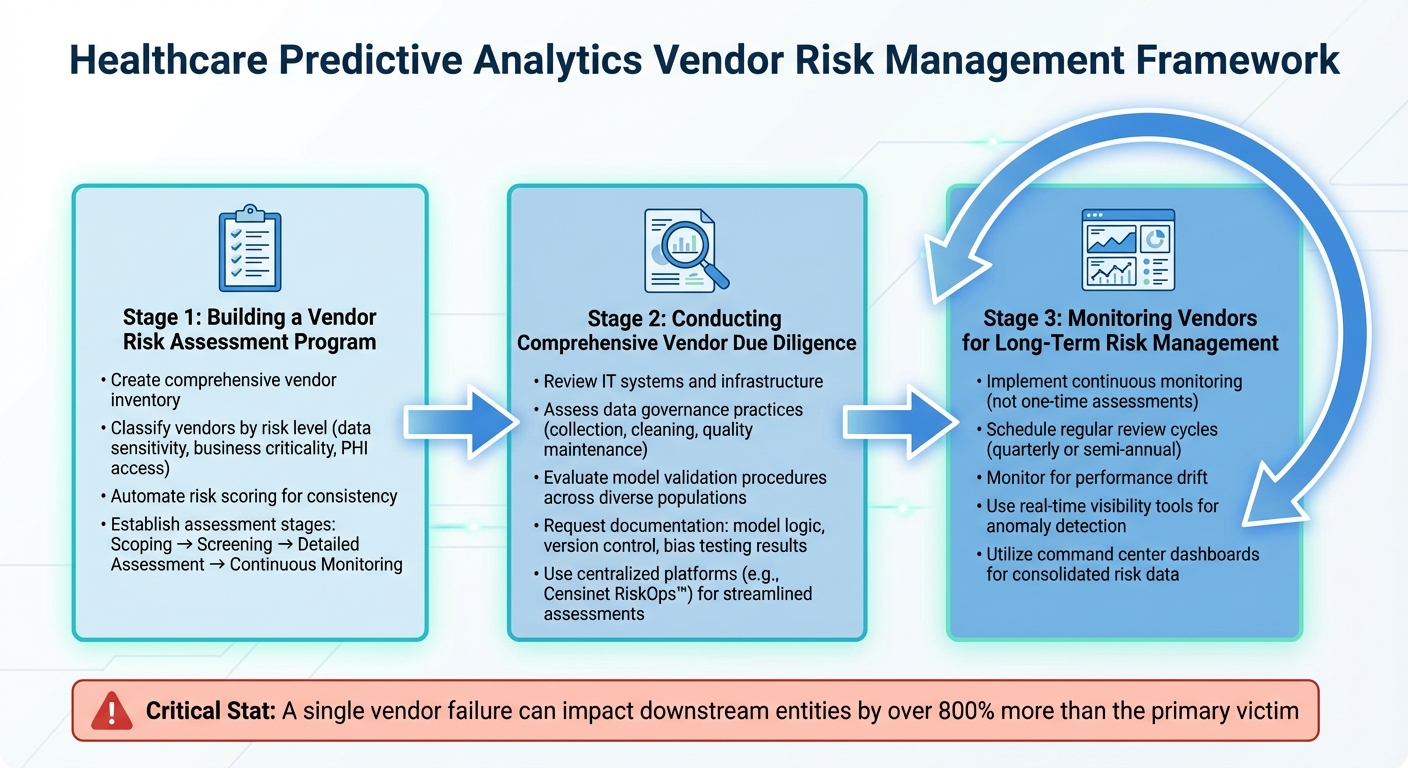
Healthcare Vendor Risk Management: 3-Stage Assessment Framework
Managing vendor risks effectively requires a structured approach for both initial evaluations and ongoing oversight.
Building a Vendor Risk Assessment Program
Start by creating a comprehensive inventory of all vendors that have access to your data. Then, classify these vendors based on their risk levels, taking into account factors like the sensitivity of the data they handle, their importance to your business operations, and whether they access protected health information. This classification ensures that high-risk vendors are prioritized for more thorough assessments. Automating risk scoring can help maintain consistency across evaluations.
Your program should include clear stages: begin with scoping to understand the nature of each vendor relationship, followed by initial screening to identify potential red flags. For vendors that pass the screening, conduct detailed assessments, and implement continuous monitoring to track their performance over time. Once vendors are categorized, focus on verifying their technical and operational safeguards in depth.
Conducting Comprehensive Vendor Due Diligence
Once your vendor inventory is in place, move on to a deeper evaluation. This due diligence process should include a thorough review of the vendor's IT systems, data management practices, and infrastructure [11]. Assess how they govern data - specifically, how they collect, clean, and maintain its quality. Also, review their model validation procedures to ensure their tools are tested across diverse patient populations.
Request documentation that includes details about their model logic, version control systems, and results from bias testing. Platforms like Censinet RiskOps™ can streamline this process by centralizing risk data and automating assessments. Its collaborative features allow teams from clinical, technical, and compliance departments to contribute their insights during vendor evaluations. This step lays the groundwork for ongoing vigilance and monitoring.
Monitoring Vendors for Long-Term Risk Management
Vendor assessments shouldn’t be a one-and-done task. Continuous monitoring is critical to safeguarding patient safety while ensuring the benefits of predictive analytics are maintained [1] [4] [10] [11]. Regular reviews help identify issues like performance drift - where models that once delivered accurate predictions begin to falter due to changes in patient demographics or clinical practices.
Set up regular review cycles, such as quarterly or semi-annual assessments, to reassess vendor risks. Real-time visibility tools are particularly useful for detecting anomalies in data access or transactions that might indicate security breaches [1]. Platforms like Censinet RiskOps™ provide command center dashboards that consolidate risk data from all vendors, making it easier to spot trends and respond quickly to emerging concerns.
Conclusion: Protecting Healthcare Through Better Vendor Risk Management
The healthcare predictive analytics market is growing at an impressive pace, offering exciting opportunities to enhance patient outcomes. However, this growth also brings heightened risks related to data quality and the reliability of predictive models. These risks underscore the importance of maintaining strict and continuous oversight of vendors. Faulty predictions can jeopardize patient safety, lead to compliance issues, and put sensitive health data at risk - making consistent monitoring an absolute necessity.
Predictive models aren’t static; they need regular updates to align with changes in regulations, clinical practices, and patient demographics. As mentioned earlier, frequent vendor evaluations are crucial to ensure compliance and protect patient outcomes. Without this ongoing vigilance, potential risks can quickly spiral out of control, harming patient care and the organization’s reputation. Over-reliance on automated systems without proper human oversight can also result in errors, misinterpretations, and ethical challenges, ultimately affecting the quality and fairness of care.
Failing to properly oversee vendors can have severe consequences. Organizations might face data breaches, hefty fines, lawsuits, financial losses, and reputational harm. Alarmingly, the ripple effects of a single vendor failure can impact downstream entities by over 800% more than the primary victim [11]. This shows how one weak link in the chain can disrupt the entire healthcare ecosystem.
Tools like Censinet RiskOps™ can play a pivotal role in managing these challenges. By centralizing risk data, automating assessments, and providing real-time visibility into vendor performance, this platform simplifies the process of identifying potential issues. Its command center dashboards offer a consolidated view of all vendors, enabling quicker detection of emerging risks. Additionally, Censinet AI™ accelerates risk assessments while keeping human oversight in the loop, allowing healthcare organizations to scale their efforts without compromising safety or control. The platform also promotes collaboration among clinical, technical, and compliance teams, ensuring vendor practices are evaluated thoroughly.
FAQs
What steps can healthcare organizations take to ensure the quality of data from predictive analytics vendors?
Healthcare organizations can maintain high-quality data from predictive analytics vendors by implementing strong validation processes. This can involve leveraging AI-powered tools to automatically verify and standardize incoming data, cross-referencing information with reliable external databases, and keeping comprehensive audit logs to spot and resolve discrepancies.
Beyond validation, it's crucial to set up clear data governance policies. Organizations should require vendors to meet strict quality benchmarks and regularly evaluate the performance of predictive models to ensure they deliver accurate and reliable results. These practices not only reduce the risks tied to flawed or biased models but also help organizations stay compliant with healthcare regulations.
What are the risks of relying on 'black box' algorithms in healthcare predictive analytics?
Relying on 'black box' algorithms for healthcare predictive analytics can pose serious challenges. These models often operate without clarity, making it hard to understand or explain how they arrive at specific decisions. This lack of insight can result in misdiagnoses, jeopardize patient safety, and even lead to legal complications if outcomes can’t be adequately explained.
Another concern is the potential for bias within these models. If the training data is flawed or doesn’t represent diverse populations, the predictions may reflect those same shortcomings. Without proper validation, the risk of inaccurate forecasts grows, eroding trust and leading to poor decisions in both clinical and operational settings. Addressing these issues requires a careful review of vendor practices, maintaining high standards for data quality, and insisting on detailed documentation about how these models are built and tested.
How does ongoing vendor monitoring help ensure reliable predictive models in healthcare?
Keeping a close eye on vendors is essential for ensuring the reliability of predictive models in healthcare. Regular monitoring helps spot risks early, such as data quality issues, biases, or inaccuracies that could throw off a model's performance. It also ensures that the models meet healthcare cybersecurity standards, making them dependable for critical decision-making.
By staying ahead of potential issues, like data breaches or faulty algorithms, healthcare organizations can address vulnerabilities before they affect patient outcomes. This ongoing oversight protects the integrity of predictive analytics, allowing for more confident and accurate decision-making.
Related Blog Posts
- Custom Vendor Risk Scoring: Key Benefits for HDOs
- Machine Learning Vendor Risk Assessment: Data Quality, Model Validation, and Compliance
- Clinical Decision Support AI Vendors: Risk Management and Patient Safety Considerations
- Healthcare AI Data Governance: Privacy, Security, and Vendor Management Best Practices


