How to Compare Risk Assessment Models in Healthcare
Post Summary
AI speeds detection, automates containment, and reduces manual work by up to 80%.
No—AI augments human judgment with faster insights and automation.
EHR reliance, IoT/medical devices, HIPAA rules, and large supplier networks.
Analysts verify AI outputs, leaders get clearer decision‑support, and threat intel teams gain faster context.
Through real‑time monitoring, automated isolation, guided recovery, and post‑incident analytics.
With AI oversight committees, bias testing, adversarial monitoring, and integrated GRC workflows.
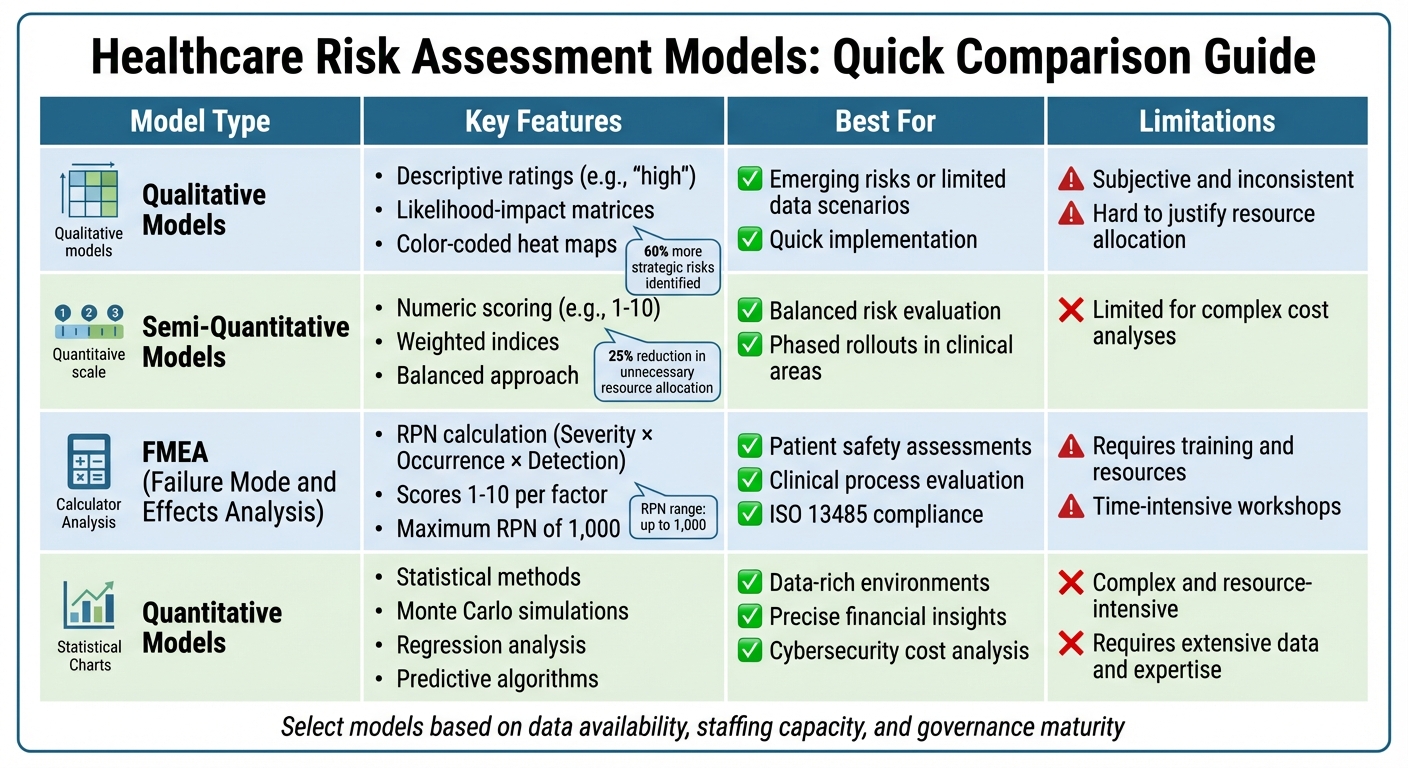
Risk assessment models are critical for healthcare organizations to manage risks like patient safety issues, IT threats, and vendor vulnerabilities. Choosing the right model ensures compliance with regulations like HIPAA and improves decision-making across teams. Here's a quick breakdown of the most common models:
To select the best model, align it with your organization's goals, data availability, staff capacity, and governance structure. Standardizing criteria like likelihood, impact, and severity ensures consistent comparisons and resource allocation.
Quick Comparison:
Model Type
Key Features
Best For
Limitations
Qualitative
Descriptive ratings (e.g., “high”)
Emerging risks or limited data
Subjective and inconsistent
Semi-Quantitative
Numeric scoring (e.g., 1–10)
Balanced risk evaluation
Limited for complex cost analyses
FMEA
RPN (Severity × Occurrence × Detection)
Patient safety assessments
Requires training and resources
Quantitative
Statistical methods, simulations
Data-rich environments, precise insights
Complex and resource-intensive
To effectively compare models, define your goals, standardize evaluation criteria, and assess model performance. Tools like Censinet RiskOps™ can streamline this process, offering automation and benchmarking for healthcare-specific risks.
Comparison of Healthcare Risk Assessment Models: Features, Best Uses, and Limitations
Risk Domains and Evaluation Criteria in Healthcare
Main Risk Domains in Healthcare
Healthcare organizations juggle risks across six key areas: vendors and third parties, patient data, medical records, research and IRB, medical devices, and supply chain [1]. These domains are deeply interconnected. For example, a cybersecurity breach in a vendor's system could expose sensitive patient data, disrupt the operation of medical devices, and even throw supply chains into chaos - all at once. Cybersecurity acts as the linchpin here; a single vendor-related breach can set off a chain reaction of risks across multiple domains [1]. When evaluating risk assessment models, it’s critical to consider how these domains overlap. Focusing on cascading risks, rather than treating each domain as an isolated entity, ensures a more comprehensive approach to risk management.
Setting Standard Risk Criteria
To effectively evaluate and compare risk models, healthcare organizations need clear and consistent criteria. Commonly used metrics include likelihood (how probable an event is) and impact (the extent of harm, such as financial loss or threats to patient safety). In Failure Mode and Effects Analysis (FMEA) models, three additional factors - severity (S), occurrence (O), and detection (D) - combine to calculate a Risk Priority Number (RPN) that can reach up to 1,000 [2].
Standardizing these scales - such as assigning values from 1 to 10 for likelihood and impact - makes it easier to compare different models, whether they’re qualitative matrices, semi-quantitative RPNs, or fully quantitative systems. For instance, aligning FMEA thresholds with these scales can help reduce patient safety incidents and allocate resources more effectively.
Organizational Factors That Affect Model Selection
The choice of a risk assessment model depends heavily on three organizational factors: data availability, staffing capacity, and governance maturity.
Budget constraints and the ability to adapt to shifting resources also play a big role in determining which model is practical. By assessing their current data systems, staffing levels, and governance capabilities, healthcare organizations can select a risk assessment approach that aligns with their operational realities. This ensures that the model is not just aspirational but actionable, setting the stage for meaningful improvements in risk management.
Common Risk Assessment Models in Healthcare
Qualitative Risk Matrix Models
Qualitative models rely on tools like likelihood–impact matrices and color-coded heat maps to evaluate risks. Healthcare teams might use scenario-based workshops or methods like the Delphi technique, where experts independently assess risks and then reach a consensus through structured discussions [2].
The main advantage of qualitative models is their ease of implementation and adaptability. These models can be quickly adopted, even when historical data is limited, making them especially useful for addressing emerging risks like new cybersecurity threats or sudden supply chain issues. They also encourage collaboration across departments. However, subjectivity is a significant drawback. Different risk managers might interpret and rank the same risk differently, which can lead to inconsistencies and make resource allocation harder to justify [2].
Semi-Quantitative Scoring Models
Semi-quantitative models bridge the gap by assigning numeric scores to risks, offering more consistency while keeping the process manageable. A well-known example in healthcare is Failure Mode and Effects Analysis (FMEA). This method calculates a Risk Priority Number (RPN) by multiplying three factors: Severity (S), Occurrence (O), and Detection (D), each scored from 1 to 10. The RPN can range up to 1,000 [2].
Organizations using weighted indices for operational risks have reported identifying 60% more strategic risks and cutting unnecessary resource allocation by 25% [2]. These models are particularly effective for phased rollouts in high-priority clinical areas and align with standards like ISO 13485, ensuring consistency for regulatory compliance. However, they may fall short when detailed cost-benefit analyses are needed [2]. Despite their limitations, semi-quantitative models provide a solid foundation for transitioning to data-intensive approaches.
Quantitative and Statistical Models
Quantitative models take a more data-driven approach, using advanced tools and statistical methods to deliver precise risk assessments. These models rely on techniques like Monte Carlo simulations, regression analysis, and predictive algorithms to calculate expected financial losses and probabilities of specific events. For example, estimating the annual cost of ransomware attacks involves analyzing historical breach data, recovery expenses, and downtime impacts.
These models are often reserved for mature healthcare organizations dealing with financial risks or cybersecurity threats, where precise calculations can directly inform decisions about budgets and insurance coverage. However, their complexity can be a barrier. Quantitative models require extensive data, specialized expertise, and significant time, making them less practical for smaller organizations or those lacking robust historical records. They work best in environments with strong governance structures and dedicated analytics teams [2].
How to Compare Risk Assessment Models in Healthcare
When comparing risk assessment models, it’s essential to build on the foundational risk domains and standardized criteria previously discussed. This process helps healthcare organizations select the most suitable model - whether it's a qualitative heat map, a semi-quantitative FMEA, or a quantitative statistical approach - by balancing technical precision with practical workflows. The goal is to match the model to the organization’s specific risk areas and operational needs.
Step 1: Define Your Comparison Goals
Start by clearly outlining your objectives. Are you looking to standardize models across departments to avoid inconsistencies in vendor risk assessments? Do you plan to use different models for specific risk domains - like FMEA for patient safety and quantitative methods for cybersecurity? Or is your aim to align existing practices with regulations such as HIPAA or ISO 31000?
For example, a regional healthcare network that implemented FMEA across clinical departments identified 60% more strategic risks and reduced excess capital allocation by 25% [2]. This case illustrates how setting clear goals can lead to better resource management. Forming cross-functional committees early in the process ensures that evaluation criteria remain consistent across teams [2].
Once your goals are established, the next step is to standardize the criteria used to compare the models.
Step 2: Standardize Risk Criteria and Scales
Consistency is key when comparing different models. Use uniform scales across all models to ensure fairness. For qualitative models, adopt standardized likelihood-versus-impact matrices with consistent color-coding. For semi-quantitative methods, calculate Risk Priority Numbers (RPN = Severity × Occurrence × Detection, with a maximum score of 1,000) using identical 1–10 scales for each factor [2][3]. Weighted scoring systems should also follow the same point ranges and thresholds across departments.
To ensure everyone is on the same page, provide training on these standardized scales, starting with high-priority clinical processes. Some healthcare networks have successfully combined FMEA with ISO 31000 frameworks, creating a shared risk language that helps teams prioritize risks effectively [2].
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." - Brian Sterud, CIO, Faith Regional Health
With uniform criteria established, you can move on to evaluating how well each model performs and fits into your organization’s workflows.
Step 3: Evaluate Model Performance and Fit
Assess each model’s performance using metrics like calibration, ROC curves, and predictive range to confirm its accuracy in risk prediction. Calibration ensures that predicted risks align with observed outcomes, which is especially important for readmission risk models [4]. ROC curves (Receiver Operating Characteristic) highlight the trade-off between sensitivity and specificity, with the area under the curve serving as a measure of predictive accuracy [4]. Predictive range evaluates how well models stratify risk by comparing event rates in high- and low-risk groups, aiding clinical decision-making [4].
Beyond performance, consider how well each model integrates into your workflows.
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required." - Terry Grogan, CISO, Tower Health
The ideal model should address healthcare-specific risks - like those involving vendors, patient data, medical devices, and supply chains - while minimizing manual processes. This ensures the model is not only effective but also practical for everyday use.
sbb-itb-535baee
Using Censinet RiskOps™ to Compare and Manage Risk Models

Applying Multiple Risk Models with Censinet RiskOps™
Censinet RiskOps™ is a cloud-based platform designed specifically for healthcare, using AI to simplify and strengthen risk management. It allows healthcare organizations to compare multiple risk models on a single platform. This is particularly useful in tackling complex challenges like managing risks tied to third-party vendors dealing with patient health information (PHI), clinical applications, medical devices, and supply chains. By replacing outdated, manual spreadsheet-based processes, the platform streamlines operations [1].
The platform supports phased implementation, starting with high-priority areas. It uses automated workflows to recalculate risk scores, helping organizations create a standardized risk language across departments [2]. These features also enable collaborative benchmarking, enhancing overall risk management strategies.
Collaboration and Benchmarking Features
Censinet RiskOps™ takes collaboration to the next level by connecting users to an extensive network of over 50,000 vendors and products. This collaborative risk network enables the sharing of cybersecurity and risk data, fostering collective insights that improve risk management. One standout feature is the Cybersecurity Benchmarks solution, which allows healthcare organizations to compare their risk outputs and program effectiveness against industry peers. This helps identify weaknesses and secure the resources needed to address them [1].
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with."
– James Case, VP & CISO, Baptist Health
Organizations like Faith Regional Health benefit greatly from these benchmarking tools, using them to measure their performance against industry standards and stay ahead in critical areas [1].
Continuous Improvement in Risk Assessment
Censinet RiskOps™ ensures risk assessment processes stay current by integrating real-world data from its collaborative network and adapting to regulatory updates. This approach allows healthcare organizations to continuously refine their risk models. By aligning automated updates with standardized risk criteria, the platform strengthens the shared risk language established across teams.
Phased rollouts make this process manageable - starting with training teams on standardized scales and then automating workflows for multiple models. This enables organizations to adjust priorities based on recalculated risk scores [2]. Additionally, Censinet AI™ accelerates tasks like automating vendor questionnaires, summarizing documents, and generating detailed risk reports. This blend of automation and human oversight ensures healthcare organizations can scale their risk management efforts to keep pace with emerging threats and compliance demands.
Conclusion: Selecting the Right Risk Assessment Approach
Key Points for Healthcare Organizations
When it comes to choosing a risk assessment model, healthcare organizations need to ensure it aligns with their goals, risk tolerance, and regulatory responsibilities. The right model should address specific areas like patient safety, cybersecurity, vendor management, or supply chain challenges. It’s also crucial that the model complies with regulations such as HIPAA, HITECH, and Joint Commission standards while being practical for day-to-day use by staff.
Consistency in risk criteria is just as important as selecting the model itself. As noted earlier, standardizing scoring scales across the organization ensures that a "high" risk in one area, like patient safety, is interpreted the same way as a "high" risk in another, such as cybersecurity. This shared understanding helps teams allocate resources more efficiently and communicate effectively with leadership. Organizations that adopt a unified risk language and scoring system often see better collaboration and outcomes.
Ease of use is non-negotiable. Even the most well-designed model won’t deliver results if it’s too complicated for clinicians, IT staff, or compliance teams to implement. Healthcare-specific tools are essential due to the industry’s unique demands. Consider factors like training needs, integration into existing workflows, and the ability to scale across multiple facilities when evaluating your options.
Next Steps for Implementation
To embed a consistent risk assessment process, start with a clear plan of action. Begin by reviewing your current risk assessments to identify gaps and inconsistencies. Next, establish enterprise-wide criteria for assessing risks. This could include standardized scales for likelihood and impact (e.g., 1–5 or 1–10), financial loss thresholds in USD, and patient safety severity levels that everyone can easily understand.
Once you’ve assessed your current practices, it’s time to put your chosen methodology into action. Pilot the approach with one or two high-priority areas, such as vendor cybersecurity risks or medication safety concerns. Use this trial phase to refine templates and workflows based on real-world feedback. After making any necessary adjustments, gradually roll out the model across the organization.
Set up a regular review schedule - quarterly for fast-changing areas like cybersecurity and annually for others. Monitor performance metrics such as incident rates, response times, and financial losses to ensure the model is effective. Tools like Censinet RiskOps™ can streamline this process by providing standardized frameworks, automated workflows, and benchmarking data from over 50,000 healthcare vendors. This helps shift your approach from reactive to structured and well-organized, making risk management more efficient and impactful.
FAQs
What should healthcare organizations look for in a risk assessment model?
When choosing a risk assessment model, healthcare organizations should prioritize factors such as precision, relevance to the organization's specific risks, and how easily it can be put into practice. The model should align with established industry standards and have the flexibility to incorporate new data as threats and vulnerabilities change over time.
It’s also crucial to evaluate whether the model offers practical insights that can drive action, integrates smoothly with current systems, and supports ongoing risk management efforts. These capabilities are key for addressing risks tied to patient data, clinical tools, and other essential aspects of healthcare operations.
Why are standardized risk criteria important for comparing healthcare models?
Standardized risk criteria play a key role in evaluating healthcare models by providing a uniform framework for assessment. With this approach, organizations can measure and compare different models using the same set of benchmarks, ensuring evaluations are both precise and consistent.
This standardization not only enhances transparency but also supports better decision-making. It enables healthcare organizations to craft stronger risk management strategies while fostering alignment among stakeholders. Moreover, it encourages smoother collaboration across teams and institutions, ultimately benefiting the broader healthcare system.
Why is data availability important when choosing a risk assessment model?
When it comes to choosing a risk assessment model, the availability of data is absolutely key. Why? Because the quality and breadth of data directly influence how accurate and dependable the model will be. With detailed and reliable data, the model can pinpoint vulnerabilities, anticipate potential risks, and offer insights that help guide smarter decisions.
On the flip side, if the data is lacking or incomplete, the model's results might fall short - leading to gaps in understanding and potentially undermining your organization's ability to manage risks effectively. Having strong, reliable data is the foundation for generating assessments you can trust.
Related Blog Posts
- ISO 27001 Risk Assessment: Qualitative Methods for Healthcare
- What Is Qualitative Vendor Risk Scoring?
- Vendor Risk Assessment Methods for Healthcare: Quantitative vs. Qualitative Approaches
- Vendor Risk Assessment Methods for Healthcare: Quantitative vs. Qualitative Approaches
{"@context":"https://schema.org","@type":"FAQPage","mainEntity":[{"@type":"Question","name":"What should healthcare organizations look for in a risk assessment model?","acceptedAnswer":{"@type":"Answer","text":"<p>When choosing a risk assessment model, healthcare organizations should prioritize factors such as <strong>precision</strong>, <strong>relevance to the organization's specific risks</strong>, and <strong>how easily it can be put into practice</strong>. The model should align with established industry standards and have the flexibility to incorporate new data as threats and vulnerabilities change over time.</p> <p>It’s also crucial to evaluate whether the model offers <strong>practical insights</strong> that can drive action, integrates smoothly with current systems, and supports <strong>ongoing risk management efforts</strong>. These capabilities are key for addressing risks tied to patient data, clinical tools, and other essential aspects of healthcare operations.</p>"}},{"@type":"Question","name":"Why are standardized risk criteria important for comparing healthcare models?","acceptedAnswer":{"@type":"Answer","text":"<p>Standardized risk criteria play a key role in evaluating healthcare models by providing a uniform framework for assessment. With this approach, organizations can measure and compare different models using the same set of benchmarks, ensuring evaluations are both precise and consistent.</p> <p>This standardization not only enhances transparency but also supports better decision-making. It enables healthcare organizations to craft stronger risk management strategies while fostering alignment among stakeholders. Moreover, it encourages smoother collaboration across teams and institutions, ultimately benefiting the broader healthcare system.</p>"}},{"@type":"Question","name":"Why is data availability important when choosing a risk assessment model?","acceptedAnswer":{"@type":"Answer","text":"<p>When it comes to choosing a risk assessment model, the availability of data is absolutely key. Why? Because the quality and breadth of data directly influence how accurate and dependable the model will be. With detailed and reliable data, the model can pinpoint vulnerabilities, anticipate potential risks, and offer insights that help guide smarter decisions.</p> <p>On the flip side, if the data is lacking or incomplete, the model's results might fall short - leading to gaps in understanding and potentially undermining your organization's ability to manage risks effectively. Having strong, reliable data is the foundation for generating assessments you can trust.</p>"}}]}
Key Points:
How does AI strengthen healthcare incident response?
- Cuts threat detection time by up to 90% via continuous monitoring
- Automates alert correlation to reduce false positives
- Speeds containment, isolating compromised systems and accounts
- Enhances recovery sequencing based on clinical criticality
- Reduces manual workloads by 80%, enabling strategic focus
What makes healthcare an especially difficult environment for AI‑enabled incident response?
- Ransomware can halt clinical operations, impacting patient safety
- Medical devices and IoMT often can’t be taken offline
- Strict HIPAA/HITECH requirements increase documentation needs
- Large vendor ecosystems create supply‑chain vulnerabilities
- Legacy systems make detection and patching difficult
How does AI change roles within incident response teams?
- IR leads gain real‑time decision support and simplified prioritization
- SOC analysts shift from manual triage to validating AI signals
- Threat intel analysts receive faster insight from unstructured data sources
- Cyber + data science teams jointly oversee model performance
- Clinical/compliance leaders see clearer PHI and workflow impact indicators
How does AI enhance each phase of the NIST incident response lifecycle?
- Preparation: Simulates realistic attacks and identifies weak points
- Detection: Finds anomalies across EHRs, IoMT, networks, and vendors
- Containment: Automates quarantine of devices, credentials, or cloud assets
- Recovery: Prioritizes restoration based on clinical urgency
- Post‑incident review: Builds timelines, root‑cause analysis, and updated detection logic
How can organizations govern AI safely and responsibly?
- AI oversight committees to manage bias, drift, and adversarial risks
- AI risk registers integrated into GRC workflows
- Pre‑deployment testing for accuracy and fairness
- Continuous monitoring for model drift and anomalous behavior
- Quarterly audits to validate performance and policy alignment
How does Censinet RiskOps™ support AI‑driven incident response programs?
- Centralizes AI‑specific risks across vendors, devices, and applications
- Automates third‑party AI assessments using healthcare‑specific criteria
- Tracks vulnerabilities and incidents in real time
- Benchmarks AI readiness against peer organizations
- Unifies cybersecurity, compliance, and clinical impact data for governance


