Multi-Region or Multi-Cloud? The Architecture Decision Healthcare Can No Longer Postpone
Post Summary
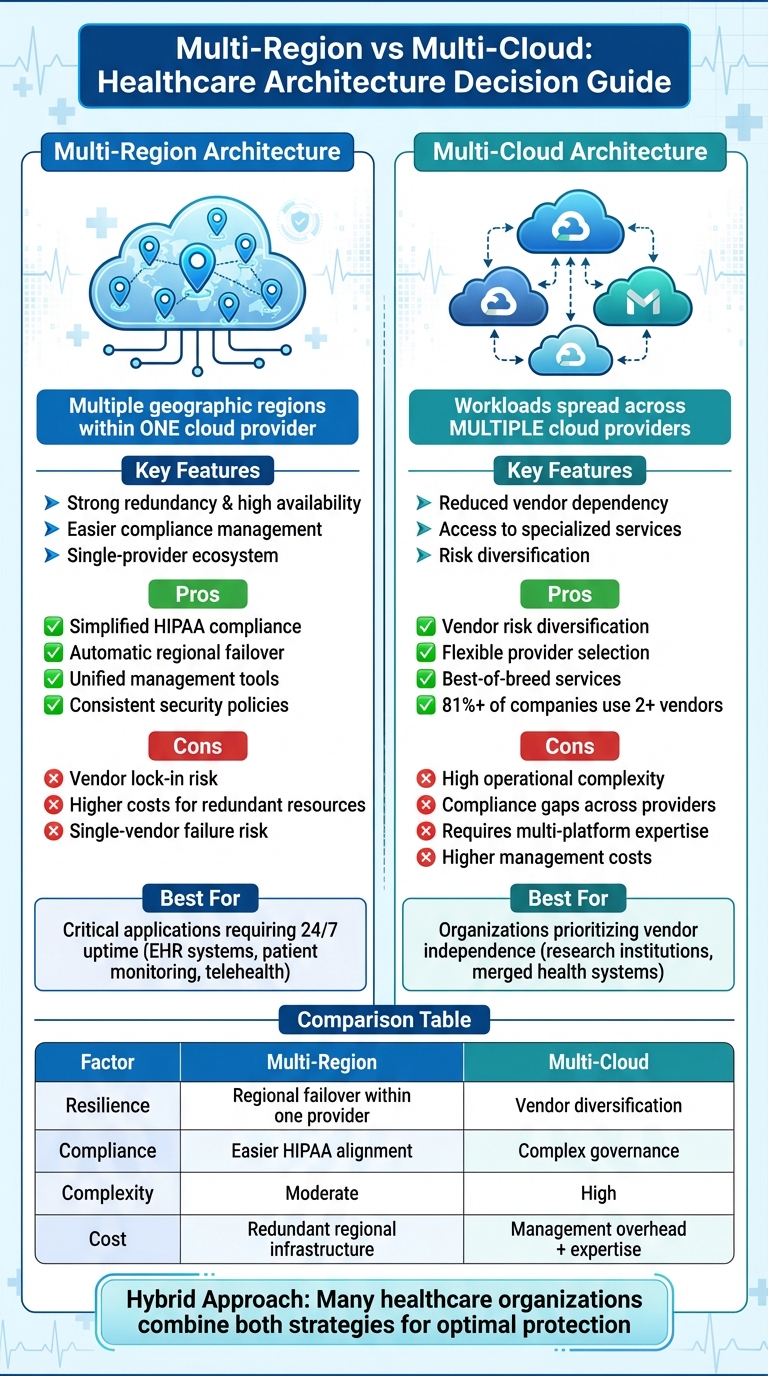
Healthcare organizations are facing a critical decision: multi-region or multi-cloud architecture? This choice directly impacts patient care, data security, and compliance with regulations like HIPAA. Here's the breakdown:
- Multi-region architecture: Uses multiple geographic regions within a single cloud provider. It offers strong redundancy, high availability, and easier compliance management but risks vendor lock-in and higher costs for redundant resources.
- Multi-cloud architecture: Spreads workloads across multiple cloud providers. It reduces vendor dependency and allows access to specialized services but comes with higher complexity, potential compliance gaps, and increased management costs.
Both approaches have advantages and challenges. Multi-region setups excel in availability and regulatory alignment, while multi-cloud strategies provide flexibility and risk distribution. Healthcare providers must weigh their risk tolerance, compliance needs, and technical capabilities to choose the right path - or consider a hybrid approach that combines the strengths of both.
| Factor | Multi-Region | Multi-Cloud |
|---|---|---|
| Resilience | Single-provider redundancy; regional failover | Vendor risk diversification |
| Compliance | Easier within one ecosystem | Complex governance across providers |
| Complexity | Moderate | High |
| Cost | Higher for redundant regional resources | Higher for management and expertise |
Start by identifying your most critical systems and evaluating your team’s readiness to manage either architecture. The right choice depends on your organization’s priorities and capabilities.
Multi-Region vs Multi-Cloud Architecture Comparison for Healthcare
1. Multi-Region Architecture
Multi-region architecture involves deploying redundant application and database instances across different geographic regions. This setup ensures that if one region experiences downtime, another can seamlessly take over, maintaining uninterrupted service [1].
Cybersecurity and Resilience
The standout feature of multi-region architecture is its built-in redundancy. By replicating data and applications across multiple regions, organizations can shield themselves from threats like ransomware attacks, natural disasters, or infrastructure failures. If one region encounters a breach or data loss, the replicated data in other regions ensures operations continue with minimal disruption [1].
Compliance and Regulatory Alignment
In the healthcare sector, multi-region setups are often used to align with HIPAA requirements. While HIPAA doesn’t explicitly demand that data stays within U.S. borders, it does call for stringent safeguards to protect Protected Health Information (PHI). Multi-region architecture supports these safeguards by enabling robust data replication and backup. It also helps organizations meet broader data privacy regulations across different regions [1][3][4].
Operational Complexity and Cost
While the benefits of multi-region architecture - such as high availability and enhanced risk management - are clear, adopting this approach comes with challenges. It requires more complex operations and higher infrastructure costs, particularly when using traditional databases [1]. Managing parallel systems demands detailed monitoring and additional training. Despite these hurdles, many healthcare organizations view it as a practical solution to mitigate risks from regional outages [2].
Healthcare-Specific Use Cases
Multi-region architecture is particularly valuable for healthcare applications, enhancing data storage, analytics, and operational reliability [1]. It’s especially critical for systems like real-time patient monitoring, electronic health records (EHR) for hospital networks, and telehealth platforms. These applications rely on consistent access to patient data, even during regional disruptions. While this setup provides focused resilience, it differs from the flexibility offered by multi-cloud architectures, which will be explored in the next section.
2. Multi-Cloud Architecture
Multi-cloud architecture involves spreading workloads across multiple cloud providers. For healthcare organizations, this approach allows them to tap into the strengths of different providers, helping them meet operational needs and adhere to compliance standards. Beyond reducing risks, this setup opens the door to addressing key aspects like cybersecurity, compliance, and cost management.
Cybersecurity and Resilience
One of the standout benefits of a multi-cloud strategy is its ability to enhance security through vendor diversification. If one cloud provider faces an outage or a breach, operations can shift to another, minimizing disruptions. This setup also strengthens disaster recovery efforts by eliminating single points of failure. However, such resilience comes with a caveat - it demands advanced security expertise to manage the complexities of multiple platforms effectively.
Compliance and Regulatory Alignment
While multi-cloud offers operational flexibility, it also introduces compliance hurdles. For healthcare providers, ensuring HIPAA compliance in a multi-cloud environment can be particularly tricky. Different cloud providers often have varying security settings, logging mechanisms, and policy frameworks, which can lead to gaps in oversight [5]. Each provider's unique approach to identity management, logging, and controls makes enforcing consistent governance across platforms a challenge [5][6]. Moreover, when data is distributed across multiple data centers and regions, maintaining audit trails and access controls becomes more complicated - a critical concern for meeting HIPAA requirements. To navigate these challenges, healthcare organizations must design unified compliance frameworks that work seamlessly across all cloud providers.
Operational Complexity and Cost
Healthcare's demand for uninterrupted service adds another layer of complexity to managing a multi-cloud environment. Without careful planning, a multi-cloud setup can lead to inefficiencies, higher costs, and management headaches [7]. To address these issues, adopting a "multicloud-by-design" approach is key. This means investing in specialized tools and expertise to ensure consistent monitoring, governance, and policy enforcement across all platforms.
Healthcare-Specific Use Cases
In healthcare, multi-cloud strategies are often shaped by necessity and innovation. For example, research institutions rely on multi-cloud setups to access high-performance computing for genomic analysis while keeping patient data compliant with HIPAA. Similarly, large health systems managing mergers and acquisitions may inherit cloud commitments from the organizations they acquire, making a multi-cloud approach less of a choice and more of a practical requirement. These examples highlight how multi-cloud can address the unique needs of the healthcare sector.
sbb-itb-535baee
Advantages and Disadvantages of Each Approach
This section highlights the key benefits and challenges of multi-region and multi-cloud architectures, focusing on resilience, compliance, and cost considerations. Both approaches offer strengths, but they also come with complexities that healthcare IT teams must weigh carefully before making decisions.
Multi-region architecture simplifies operations by staying within the same cloud provider's ecosystem. This makes it easier to maintain consistent security policies and meet compliance requirements, especially for HIPAA. For instance, many healthcare providers enhance the resilience of their electronic health records (EHRs) by deploying across multiple Availability Zones and Regions within a single cloud provider [3]. However, this approach comes with downsides, such as vendor lock-in and the cost of maintaining redundant resources across regions, even when they aren't fully utilized [1][12].
Multi-cloud architecture, on the other hand, spreads risk by using multiple cloud providers. This setup allows organizations to choose vendors with specific compliance certifications, offering a level of flexibility that multi-region setups can't match. In fact, more than 81% of companies already use two or more cloud vendors, with many hospitals relying on three or more [8]. But this flexibility introduces operational complexity. As Stuart Scott, Cloud Portfolio Director at QA, aptly notes:
"Resilience isn't something you buy – it's something you architect" [2].
Managing different security models, APIs, and compliance frameworks across various platforms requires specialized expertise. This complexity increases the risk of compliance gaps, which is particularly concerning given HIPAA's strict requirements for data retention and access controls. Fragmented policies across providers can make unified HIPAA governance a challenge [5][6][9][10].
From a cost perspective, multi-region setups incur expenses for duplicated infrastructure, while multi-cloud strategies drive costs through duplicated services and the need for expertise across multiple platforms [11][12]. Ultimately, the decision comes down to your organization's risk tolerance, budget, and technical capabilities.
| Factor | Multi-Region | Multi-Cloud |
|---|---|---|
| Resilience | Automatic traffic routing between regions; single-vendor failure risk | Diversifies vendor risks but requires more coordination |
| Compliance | Easier to maintain consistent HIPAA policies within one ecosystem | Flexible provider selection but increases risks of policy gaps |
| Operational Complexity | Moderate; unified management tools and APIs | High; demands expertise across multiple platforms |
| Cost Structure | Redundant regional resources; predictable vendor pricing | Duplicated services and higher management overhead |
This comparison underscores how each approach aligns with the unique operational and security needs of the healthcare industry.
Conclusion
The choice of architecture should align closely with your healthcare organization's specific risk profile and compliance needs. Multi-region architecture is ideal for ensuring high availability in critical applications where downtime isn't an option. It also simplifies maintaining consistent HIPAA compliance within a single provider's ecosystem. On the other hand, multi-cloud architecture is better suited for organizations that prioritize reducing vendor dependency and need the flexibility to select providers with particular compliance certifications. However, managing this setup requires advanced technical expertise due to its complexity.
That said, many healthcare organizations find that combining elements from both approaches offers the best protection. A hybrid strategy blends the reliability of multi-region setups for mitigating physical failures with the flexibility of multi-cloud systems to guard against configuration errors. This approach provides a more comprehensive safeguard and reflects the operational challenges discussed earlier.
To move forward, focus on practical steps. Begin by identifying your tier-0 applications - those systems where disruptions could lead to immediate financial, legal, or patient safety issues [1]. These should be prioritized for enhanced resilience. Then, take a hard look at your team’s skill set. If multi-cloud expertise is lacking, diving in too quickly could create vulnerabilities, particularly since configuration drift remains a significant cause of data leaks in multi-cloud environments [8].
Ultimately, your decision should hinge on your organization's risk tolerance, regulatory obligations, and operational readiness - not on following industry trends. Take time to map out your compliance requirements, weigh the true costs of redundancy and management, and develop a roadmap that your IT team can confidently implement and sustain over time.
FAQs
What’s the difference between multi-region and multi-cloud architectures in healthcare?
A multi-region architecture involves distributing applications and data across several geographic locations within the same cloud provider. This setup boosts availability, supports disaster recovery efforts, and minimizes the impact of regional outages. It’s an effective way to enhance resilience without significantly complicating your infrastructure.
In contrast, a multi-cloud architecture relies on multiple cloud providers to host workloads. This strategy promotes vendor independence and can add another layer of resilience. However, it comes with its own set of challenges, including increased complexity in managing systems, ensuring security, and meeting compliance standards - particularly tricky in healthcare, where regulations are stringent.
The best choice depends on your organization’s unique requirements, such as your risk tolerance, compliance obligations, and operational objectives.
How do multi-region and multi-cloud architectures affect HIPAA compliance?
When it comes to HIPAA compliance, both multi-region and multi-cloud architectures come with their own set of considerations.
A multi-region architecture offers enhanced data redundancy and availability. By spreading data across multiple regions, this setup helps protect patient information during regional outages. It aligns with HIPAA's privacy and security requirements by minimizing the risk of data loss and ensuring that operations can continue without interruption.
Meanwhile, a multi-cloud strategy adds a layer of complexity. Ensuring consistent security controls, encryption protocols, and audit processes across different cloud platforms can be a tough challenge. To stay compliant with HIPAA, organizations must prioritize strong encryption practices, robust identity management systems, and continuous monitoring across all platforms.
Whichever approach is chosen, success hinges on thorough planning and diligent oversight to meet HIPAA standards effectively.
What should healthcare organizations evaluate when deciding between a multi-region or multi-cloud architecture?
When choosing between a multi-region or multi-cloud architecture, healthcare organizations need to weigh a few key factors to ensure the best fit for their needs:
- Cybersecurity and compliance: The architecture must provide strong data protection and meet strict regulatory standards like HIPAA.
- Operational complexity: Think about how manageable the system will be across multiple regions or cloud platforms.
- Resilience and redundancy: Look at how well each option can handle outages and maintain uninterrupted service.
- Cost considerations: Factor in expenses for infrastructure, ongoing maintenance, and scalability.
By carefully matching these considerations to your organization's unique goals and risk management strategies, you can choose an approach that balances efficiency with compliance.
Related Blog Posts
- Ultimate Guide to Data Residency in Healthcare Cloud
- When Multi-AZ Isn't Enough: What the AWS US-EAST-1 Failure Taught Us About True Resilience
- The AWS Outage Exposed Cloud Vulnerabilities - What It Means for Healthcare Business Continuity
- The 30-40% Problem: Why Healthcare's Over-Reliance on US-EAST-1 Is a Patient Safety Risk


