Stark Law and Anti-Kickback Compliance: Vendor Relationship Risk Management
Post Summary
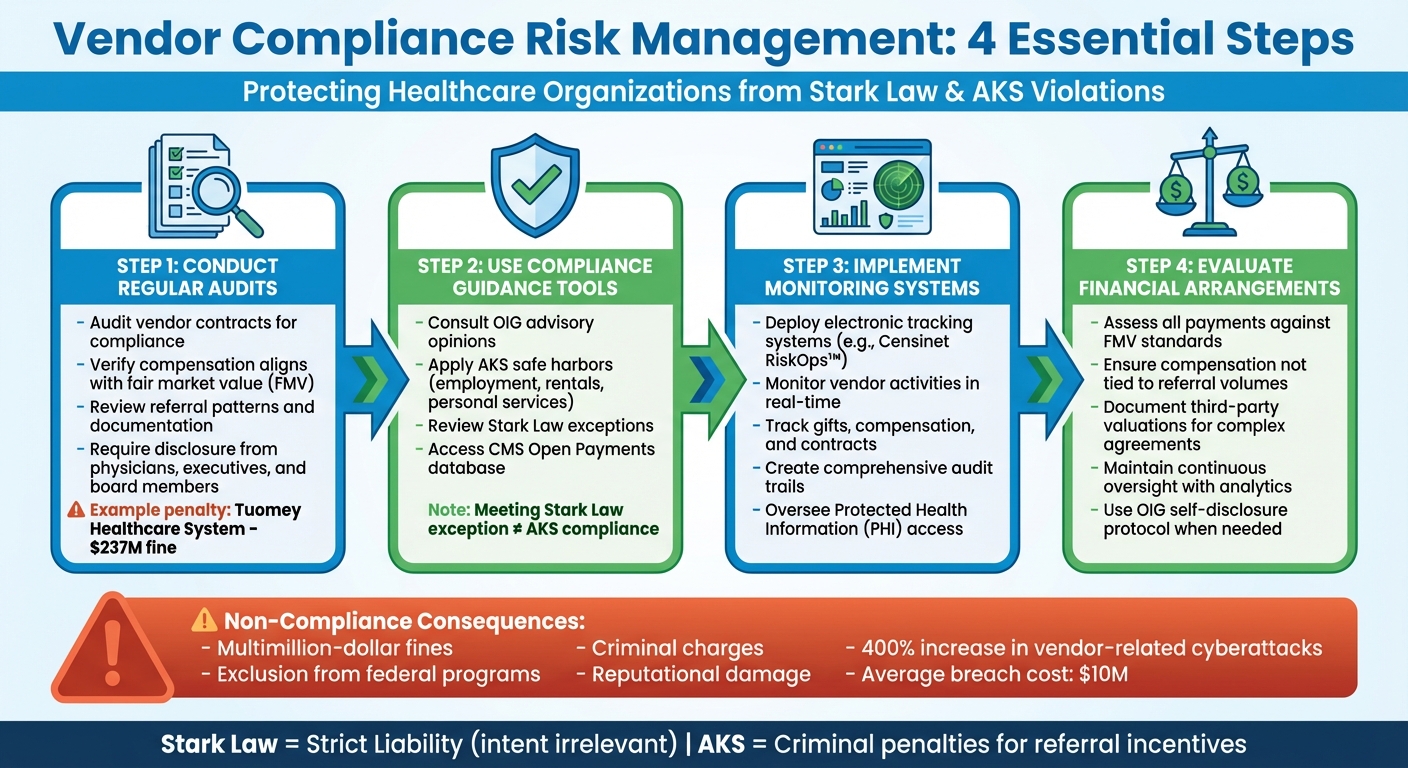
Healthcare organizations face strict legal requirements when managing vendor relationships under Stark Law and the Anti-Kickback Statute (AKS). These federal laws aim to prevent fraud and abuse by regulating financial arrangements that could influence medical decisions. Stark Law prohibits physician referrals to entities they have financial ties with unless specific exceptions apply, while AKS criminalizes any exchange of value intended to influence referrals for federally funded healthcare services.
Key Takeaways:
- Stark Law enforces a strict liability standard, meaning intent is irrelevant - any violation is actionable.
- AKS applies criminal penalties for arrangements where even one purpose is to encourage referrals.
- Non-compliance can result in severe penalties, including multimillion-dollar fines, exclusion from federal programs, and criminal charges.
- Vendor agreements involving payments, discounts, or other incentives must align with fair market value and avoid referral-based compensation.
To mitigate risks, healthcare organizations should:
- Conduct regular audits of vendor contracts to ensure compliance with legal standards.
- Use tools like CMS's Open Payments database and OIG advisory opinions for guidance.
- Implement systems like Censinet RiskOps™ for vendor risk monitoring and documentation.
- Evaluate all financial arrangements against Stark Law exceptions and AKS safe harbors.
Failure to comply can lead to financial losses, reputational harm, and operational disruptions. With enforcement becoming stricter, organizations must prioritize transparency, proper documentation, and continuous oversight to maintain compliance and protect patient trust.
4-Step Vendor Compliance Risk Management Process for Healthcare Organizations
How to Identify and Assess Compliance Risks in Vendor Partnerships
Managing compliance risks in vendor partnerships requires a structured approach. Regular audits, clear documentation, and efficient tracking are key steps to staying ahead of potential issues.
Auditing Vendor Contracts and Financial Relationships
Conducting regular audits of vendor contracts is a cornerstone of effective compliance management. These reviews should focus on ensuring that compensation structures align with fair market value and are not tied to referral volumes. For instance, the Tuomey Healthcare System was penalized $237 million under Stark Law for compensation arrangements linked to referrals, while Scripps Health in San Diego settled for $1.5 million over allegations of paying above fair market value for physician referrals [7]. These examples highlight the critical need for transparent documentation of financial relationships, referral patterns, and written agreements with clearly defined terms [4].
Organizations should also implement robust disclosure processes. Physicians, executives, directors, and board members should be required to disclose any relationships that could influence clinical or purchasing decisions. Verifying provider timesheets against contract terms ensures that services are being delivered as agreed [4]. Additionally, using official guidance and safe harbor criteria can help refine risk assessments and bolster compliance efforts.
Using OIG Advisory Opinions and Safe Harbors
Beyond audits, organizations can rely on governmental guidelines to navigate compliance requirements. The Office of Inspector General (OIG) provides advisory opinions that offer formal interpretations of healthcare laws in specific scenarios. These opinions help organizations better understand their obligations and avoid missteps.
Safe harbors under the Anti-Kickback Statute, for example, protect certain arrangements - like employment relationships, fair-market rentals, and bona fide personal services contracts - when regulatory requirements are fully met [1]. Similarly, Stark Law includes exceptions that allow physician referrals under defined conditions [8]. However, it’s important to note that meeting a Stark Law exception doesn’t automatically shield an arrangement from Anti-Kickback Statute violations. Each arrangement must be assessed under both laws independently [5]. In cases of uncertainty, consulting with experienced healthcare attorneys is a prudent step to ensure compliance [8].
Tools for Risk Identification and Documentation
Leveraging digital tools can significantly enhance risk management in vendor relationships. Electronic tracking systems allow for real-time monitoring of compliance risks. These tools can track provider activities, gifts, non-monetary compensation, and contracts, creating comprehensive audit trails. They also help organizations oversee access to protected health information and manage financial dealings as they happen [3][1].
Another resource is the CMS Open Payments database, which provides publicly available data to enhance transparency and identify potential conflicts of interest [4]. Organizations should also familiarize themselves with the OIG’s self-disclosure protocol. This protocol allows for voluntary reporting of violations, often resulting in reduced penalties [6].
With enforcement efforts becoming more rigorous and penalties increasingly difficult to insure - sometimes even leading to personal liability for healthcare executives - investing in robust tracking and documentation systems is a wise strategy for mitigating legal risks [4].
Strategies to Reduce Vendor Relationship Risks
Managing vendor relationships comes with its challenges, but with the right strategies, organizations can minimize risks and maintain compliance. By conducting thorough risk assessments and implementing targeted solutions, healthcare providers can ensure fair practices, streamline processes, and safeguard against potential violations. Here’s how:
Fair Market Value (FMV) Evaluations
Ensuring vendor payments align with fair market value (FMV) is a cornerstone of compliance with Stark Law and the Anti-Kickback Statute. Payments must reflect prevailing market rates and avoid any connection to referral volumes. Even minor deviations can lead to violations under Stark Law’s strict liability rules[1].
To stay compliant, organizations should regularly review all compensation arrangements, such as physician contracts, lease agreements, and service contracts. Detailed documentation and FMV analyses are essential, especially for complex agreements, where third-party valuations can provide an added layer of assurance[8]. Regular monitoring, supported by accessible contract terms and analytics, helps identify anomalies and ensures adherence to established standards[9].
Once FMV compliance is established, attention shifts to onboarding and monitoring processes to further reduce risks.
Vendor Onboarding and Monitoring with Censinet RiskOps™
A thorough vendor onboarding process is critical for maintaining compliance over time. Censinet RiskOps™ simplifies this by offering a centralized platform that supports in-depth due diligence before entering into financial agreements. This platform enables healthcare organizations to evaluate vendor security protocols, review incident response strategies, and monitor adherence to regulatory requirements.
Censinet RiskOps™ also allows organizations to assign vendors to risk tiers based on factors like data sensitivity, system access, and potential breach impact. High-risk vendors are continuously monitored through automated tracking of vulnerabilities and security assessments. The platform integrates AI to streamline tasks such as completing questionnaires, reviewing evidence, and generating detailed risk reports. Its real-time risk visualization feature provides compliance teams with a comprehensive view of vendor relationships, which proves invaluable during audits or investigations.
Censinet Connect™ for Vendor Risk Questionnaires
Managing vendor risk questionnaires is often a daunting task for healthcare providers, with nearly half reporting that the volume of assessments feels overwhelming[10]. Censinet Connect™ tackles this issue by automating the questionnaire process, making it faster and more efficient. By accelerating evidence reviews, this tool allows compliance teams to dedicate more time to managing higher-risk vendor relationships while ensuring consistent oversight across all partnerships.
With these strategies in place, organizations can confidently navigate the complexities of vendor relationships, ensuring both compliance and operational efficiency.
sbb-itb-535baee
Continuous Monitoring and Auditing Practices
Keeping a close eye on operations through continuous monitoring and regular audits is key to staying compliant with Stark Law and the Anti-Kickback Statute. These practices help organizations spot compliance issues early, making it easier to address them before they escalate. By integrating these efforts with earlier vendor risk assessments, organizations create a seamless system of oversight.
Protocols for Continuous Oversight
To ensure effective oversight, organizations need clear procedures for tracking vendor activities, referral patterns, contracts, and the handling of Protected Health Information (PHI). This helps identify any irregularities. It's essential to have protocols in place to confirm that vendor agreements and payment structures consistently align with legal and ethical standards throughout the entire partnership.
Conclusion
Managing vendor relationships in healthcare requires ongoing attention and a commitment to compliance. Laws like the Stark Law and the Anti-Kickback Statute aren’t just bureaucratic hurdles - they’re critical safeguards designed to prevent conflicts of interest and keep medical decisions focused on patient care, not financial gain. Ignoring these regulations can lead to serious financial and reputational consequences.
On top of legal risks, cybersecurity threats make vendor management even more challenging. Recent stats show a staggering 400% increase in vendor-related attacks, with over 65% of healthcare organizations falling victim to ransomware. The financial toll? Nearly $10 million per breach on average[2]. Beyond the numbers, these incidents can derail operations and, most importantly, put patient safety at risk.
To stay compliant and secure, healthcare organizations need more than just good intentions - they need strong systems. This includes fair market value evaluations, regular contract audits, and ongoing monitoring. Tools like Censinet RiskOps™ help simplify this process by automating workflows, providing real-time vendor oversight, and flagging risks early. Together, these efforts ensure compliance with laws like HIPAA, Stark Law, and the Anti-Kickback Statute, which are interconnected. A failure in one area can ripple through an entire compliance program, making a culture of accountability essential. Leadership must set the tone, ensuring every vendor partnership aligns with ethical and patient-centered care.
As regulations evolve, such as CMS initiatives like the "Regulatory Sprint to Coordinated Care", healthcare organizations must treat vendor risk management as an ongoing effort rather than a one-off task. By maintaining strong oversight, leveraging advanced technology, and prioritizing patient safety, organizations can confidently navigate these complex challenges while upholding their commitment to quality care.
FAQs
What is the difference between the Stark Law and the Anti-Kickback Statute?
The Anti-Kickback Statute (AKS) is a criminal law designed to prevent unethical practices in healthcare. It prohibits offering, paying, soliciting, or accepting anything of value as a way to influence or reward referrals for services covered by federal healthcare programs. To prove a violation, intent must be established, and the consequences are severe - ranging from hefty fines to possible imprisonment.
The Stark Law, in contrast, is a civil law based on strict liability. This means it doesn’t require proof of intent. It specifically prohibits physicians from referring patients for certain designated health services to entities where they or their immediate family members have a financial relationship. Violating this law can result in fines, exclusion from federal healthcare programs, and the obligation to repay claims.
Simply put, the AKS focuses on intent and applies broadly to all referrals, whereas the Stark Law zeroes in on physician self-referrals and does not consider intent.
How can healthcare organizations ensure their vendor agreements meet fair market value requirements?
Healthcare organizations can stay on top of fair market value compliance by conducting routine, well-documented fair market value assessments. These evaluations are essential for confirming that compensation agreements align with market norms and industry benchmarks.
Equally important is the need to periodically review and update vendor contracts. This ensures agreements reflect current market conditions and remain free from any connection to the volume or value of referrals. By maintaining diligent oversight and following these practices, organizations can minimize compliance risks while upholding both legal and ethical standards.
What are the best strategies to manage compliance risks in vendor relationships under Stark Law and the Anti-Kickback Statute?
To manage compliance risks in vendor relationships effectively, start by performing detailed risk assessments to uncover potential vulnerabilities. It's also crucial to establish Business Associate Agreements (BAAs) with applicable vendors to ensure they meet required legal and ethical standards. Keep a close eye on compliance by conducting regular reviews and vendor audits to verify ongoing adherence to regulations.
In addition, adopt secure onboarding and offboarding processes to maintain control over vendor access and protect sensitive data. Utilize tools like compliance dashboards, real-time monitoring systems, and audit logs to identify and address risks before they escalate. These measures not only protect your organization but also help ensure compliance with regulations like Stark Law and the Anti-Kickback Statute.
Related Blog Posts
- CMS Compliance and Vendor Risk: Medicare Requirements for Healthcare Organizations
- Healthcare Vendor Risk and Medicare Advantage: CMS Star Ratings Impact
- Revenue Cycle Vendor Risk Management: Protecting Healthcare Financial Operations
- Ambulatory Surgery Center Vendor Risk: Specialized Equipment and Safety Considerations


