How Vendor Failures Impact Patient Outcomes: Real-World Healthcare Case Studies
Post Summary
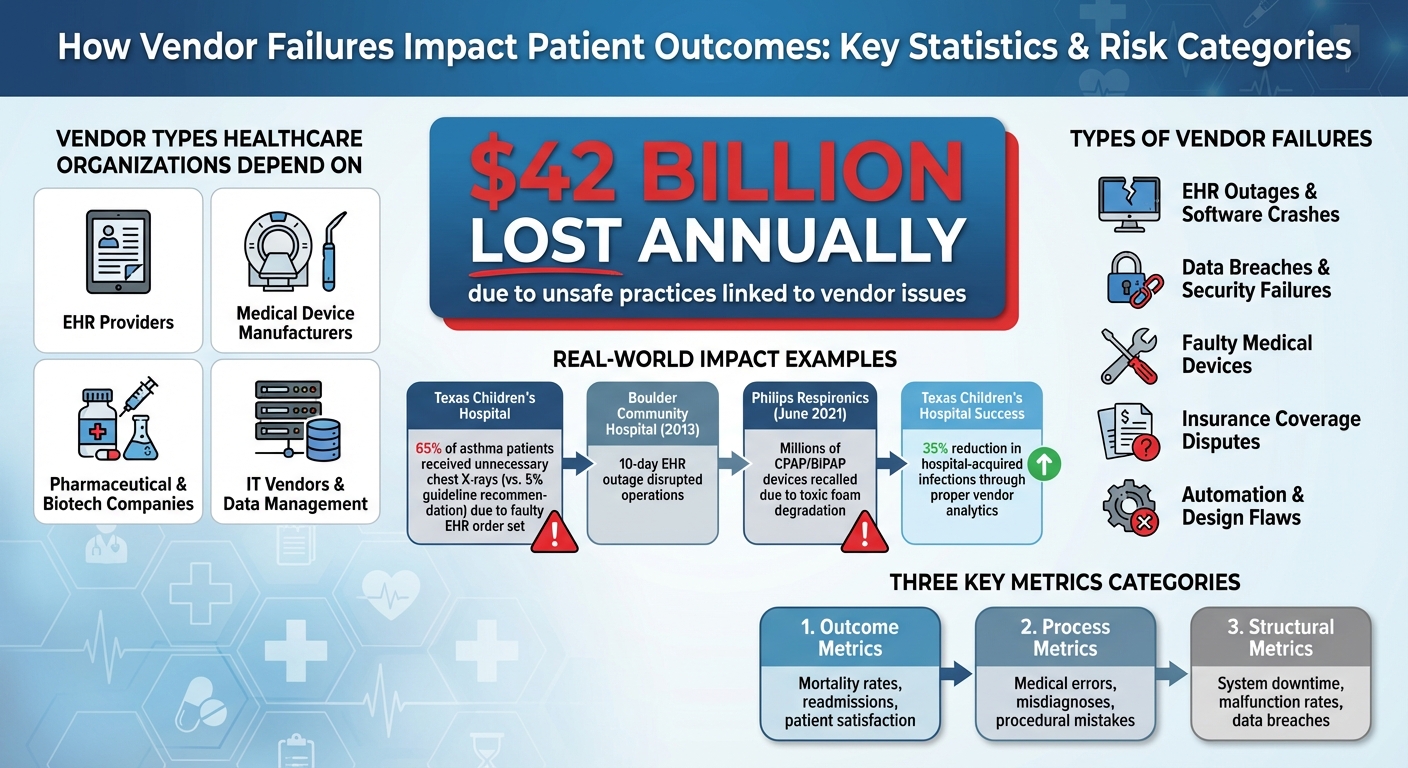
Vendor failures in healthcare can lead to serious consequences for patients and providers alike. From delayed treatments to data breaches, these issues disrupt care and jeopardize safety. Hospitals rely on thousands of vendors daily for critical services like EHRs, medical devices, and medications. When these systems falter, the ripple effects include medical errors, misdiagnoses, and even financial strain.
Key takeaways:
- $42 billion annually is lost due to unsafe practices linked to vendor issues.
- Examples include EHR outages, faulty medical devices, and insurance disputes.
- Risks range from operational failures to long-term impacts like data breaches.
- Solutions involve prioritizing high-risk vendors, involving clinical leaders in risk management, and tracking metrics like patient safety outcomes.
Vendor management isn't just about contracts - it's about protecting patient care. The article explores real incidents, practical strategies, and tools to mitigate risks effectively.
Healthcare Vendor Failure Impact Statistics and Risk Categories
Vendor-Related Risks in Healthcare
Types of Vendors Healthcare Organizations Depend On
Healthcare organizations rely heavily on various types of vendors to ensure smooth operations and quality patient care. These include EHR providers that manage patient records, medical device manufacturers responsible for life-saving equipment, pharmaceutical and biotechnology companies, and IT vendors handling data warehouses and clinical registries [2][3].
Each of these vendors plays a pivotal role in the healthcare system. EHR systems, for instance, assist clinicians in making treatment decisions, while medical devices perform essential procedures. Data management platforms, on the other hand, help identify patients at risk of complications. When any of these vendors falter, the impact can disrupt the entire care chain, with serious consequences for patient outcomes.
How Vendor Failures Lead to Patient Harm
When vendors fail, the effects can be both immediate and severe, directly jeopardizing patient safety. For example, software crashes or ransomware attacks can render EHR systems inaccessible, delaying critical care when every second counts [1]. One alarming case occurred at Texas Children's Hospital, where a faulty EHR order set resulted in 65% of asthma patients receiving unnecessary chest X-rays - contrasting sharply with guidelines recommending only 5% [3].
Data breaches are another significant risk, eroding patient trust and exposing sensitive health information [1]. Automation flaws in EHR systems can lead to delayed diagnoses, sometimes with life-threatening consequences [4]. Outdated vendor technology or poorly designed EHR systems also contribute to communication breakdowns, which can result in misdiagnoses, medication errors, and delays in vital treatments [5].
A striking example of vendor-related harm comes from the Australian Orthopaedic Association National Joint Replacement Registry. The registry flagged issues with metal-on-metal hip replacements that released cobalt ions, causing tissue damage and requiring a higher-than-expected number of revisions [2]. These examples illustrate how vendor failures can directly undermine patient care and safety.
Recent Vendor Incidents in U.S. Healthcare
Real-life examples from the U.S. healthcare system underscore the risks associated with vendor failures. In 2013, Boulder Community Hospital in Colorado faced a 10-day EHR outage caused by a system failure. The hospital managed to avoid a complete collapse by maintaining updated paper records and regularly training staff on backup procedures. However, operations were severely hindered until the system was restored [1].
On the flip side, successful vendor partnerships can lead to significant improvements in patient care. Texas Children's Hospital offers a positive example of this. By using analytics tools provided by its EDW vendor, the hospital identified at-risk patients and ensured clinicians adhered to best practices. This approach led to a 35% reduction in hospital-acquired infections [3].
These incidents highlight the critical importance of effective vendor risk management. When systems fail, the impact can be devastating, but when they function as intended, they can dramatically enhance patient outcomes.
Case Studies: Real-World Vendor Failures
Large-Scale Vendor Failures That Disrupted Care Delivery
When vendors fail in healthcare, the consequences can ripple across entire systems, leaving patients without access to critical care. Take August 2025, for example, when patients insured by UnitedHealthcare at Johns Hopkins suddenly lost their coverage for hospital services. This disruption wasn’t due to patient error but stemmed from a breakdown in negotiations between the hospital and the insurance provider. The result? Patients were left scrambling to navigate a gap in their care.
Another alarming failure happened in June 2021 when Philips Respironics issued a recall for millions of CPAP, BiPAP, and ventilator devices. The recall was prompted by the discovery that the polyester-based polyurethane foam used in the devices could degrade, releasing toxic particles or gases into patients' airways. The fallout was massive - not only were devices pulled from the market, but patients faced significant health risks, including respiratory issues, cancer, and other injuries. The recall highlighted how vendor missteps can jeopardize patient safety and create long-term public health challenges that are still being evaluated [8].
Even the design of electronic health records (EHRs) can lead to dangerous outcomes. In December 2017, a video documented by Pew Trusts revealed how a system’s auto-refresh function caused a physician to access the wrong patient’s record. This seemingly small design flaw led to care decisions based on incorrect information. Such errors aren’t just frustrating - they introduce entirely new risks for medical mistakes that didn’t exist before [9].
Failures like these show how operational issues can disrupt care delivery, but data security breaches present an entirely different kind of challenge.
Vendor Data Breaches and Their Long-Term Effects on Patients
While operational failures create immediate disruptions, data breaches have long-lasting consequences for patients. When vendors fail to secure patient health information (PHI), they open the door to identity theft, financial fraud, and a breakdown of trust in the healthcare system. Unlike stolen credit card numbers, which can be replaced, compromised health records are permanent - patients can’t simply "reset" their medical history.
The lack of national standards for health information technology and insufficient focus on privacy have left the healthcare system vulnerable [6]. When vendor systems are breached, patients often endure years of monitoring their credit, dealing with fraudulent medical claims, and living with the anxiety that their sensitive health information - such as details about mental health, substance abuse, or chronic illnesses - could fall into the wrong hands. This exposure isn’t just a privacy concern; it’s a deeply personal violation that can have a profound psychological impact.
Breaches also create practical challenges for care delivery. Patients affected by breaches may withhold critical details during medical visits, fearing that their information might not remain private. This lack of transparency leads to incomplete records, increasing the risk of misdiagnoses and perpetuating safety issues long after the breach itself has been addressed. The damage, both emotional and practical, is often felt for years.
sbb-itb-535baee
Practical Vendor Risk Management for Patient Safety
How to Identify and Prioritize Patient-Critical Vendors
Once healthcare organizations understand vendor-related risks, the next step is identifying which vendors are essential to patient care. Not every vendor carries the same level of risk. For instance, a medical device manufacturer or an electronic health record provider has a much greater potential to affect patient outcomes compared to an office supply vendor. To manage this effectively, healthcare organizations should classify vendors based on their direct impact on patient care.
Start by asking: Does a vendor’s failure directly disrupt the delivery of care? Vendors handling protected health information (PHI), supporting clinical systems, managing medical devices, or controlling critical supply chains should be classified as essential. These vendors demand more thorough assessments and ongoing monitoring. Tools like Censinet RiskOps can help by assigning risk scores, allowing organizations to focus their resources on the vendors that have the greatest influence on patient safety.
"We must, must, must stop thinking about systems primarily in technicians' terms. We must remember that the purpose of healthcare is to deliver care, and tools must support the workers who do that" [10].
Creating Risk Governance Frameworks With Clinical Input
To effectively manage vendor risks, it’s crucial to involve clinical stakeholders who can provide insights into how vendor failures might affect patient outcomes. Clinical leaders - such as chief medical officers, chief nursing information officers, and frontline clinicians - have a unique understanding of how disruptions translate into patient harm, offering perspectives that technical teams might miss.
One approach is to adopt models like the American Academy of Neurology's QMR Subcommittee [11], which integrates clinical expertise to evaluate care processes. Healthcare organizations can create similar subcommittees dedicated to vendor-related risks. These teams can establish patient-focused outcome measures, such as patient-reported experiences and satisfaction scores, to assess whether vendor services support or hinder care quality. By weaving clinical insights into risk governance, organizations can address risks that directly impact patient outcomes.
Encouraging physicians, nurses, and caregivers to actively identify and report vendor-related risks further strengthens these frameworks. When clinical staff understand their role in reporting safety concerns tied to vendors, patient safety extends beyond the bedside to encompass every vendor relationship. This collaborative approach ensures that vendor management directly contributes to safeguarding patient care.
Measuring and Reporting Vendor Risk Impact on Patient Outcomes
Metrics for Tracking Vendor Risk and Patient Safety
Healthcare organizations need clear, measurable ways to connect vendor performance with patient safety. These metrics typically fall into three categories: outcomes, processes, and structural factors [11].
Outcome metrics focus on what happens to patients during care. This includes tracking indicators like mortality rates, disease progression, functional disability, quality of life, and patient satisfaction [11]. When vendor issues arise, specific adverse events, such as serious injuries linked to technology errors, should be closely monitored [7]. Other important measures include readmission rates and physiological markers. Patient-reported experiences and satisfaction scores also provide valuable insights into how vendor disruptions affect care quality [11].
Process metrics evaluate the actions clinicians take on behalf of patients. In cases where vendor technology fails, these metrics can highlight issues like medical errors, misdiagnoses, or procedural mistakes caused by malfunctions [7]. They help pinpoint how vendor problems interfere with the delivery of care.
Structural metrics assess the systems and infrastructure that support care delivery. This includes tracking system downtime, malfunction rates, and data breaches that compromise patient privacy [7]. While these metrics don't directly measure patient outcomes, they highlight vendor performance issues that pose risks.
To effectively monitor these metrics over time, healthcare organizations can use patient registries [11]. These tools enable long-term tracking of how vendor performance impacts patient populations. It's also essential to maintain human oversight and implement failsafe measures when integrating technology, alongside robust protections for medical data [7].
By focusing on these metrics, healthcare providers can build a solid foundation for communicating vendor risks to leadership.
Communicating Vendor Risk to Boards and Leadership
Executives and board members need actionable insights that clearly connect vendor performance to healthcare quality. This includes focusing on structure, process, and outcome metrics [11]. It's crucial to emphasize how vendor failures - whether direct or indirect - can impact patient outcomes, which are the ultimate indicators of patient safety and care quality [11].
"The overall objective of health care is to improve the health of patients, and the health of patients is assessed through outcome measures."
– Eric M Cheng, MD, MS, Department of Neurology, VA Greater Los Angeles Healthcare System [11]
Highlighting care processes under clinicians' control is particularly effective, as these processes can be heavily disrupted by vendor failures [11]. For example, a large study involving elderly patients showed a strong link between well-executed care processes and reduced mortality rates [11][12]. This data can make a compelling case to leadership.
Tools like Censinet RiskOps simplify this communication by providing dashboards and standardized reporting templates. These tools centralize real-time risk data, presenting it in a way that helps executives quickly grasp the connection between vendor performance and patient safety. The platform's command center visualizes risks, ensuring critical issues are addressed by the right teams without delay.
When presenting patient outcomes to leadership, it's vital to adjust for patient risk levels. This ensures fair comparisons across different populations and strengthens the argument for allocating additional resources to vendor risk management [11].
Applying Lessons Learned and Improving Over Time
Addressing systemic vulnerabilities is a critical step in improving vendor risk management. Healthcare organizations should reframe cybersecurity as an ethical responsibility tied to patient safety, public trust, and transparency - not just as a technical issue [13]. This mindset helps integrate vendor risk management into the organization's culture.
"Cybersecurity in healthcare must therefore be reframed not as an IT concern but as an ethical responsibility tied to online safety, transparency and public trust."
– Ann Gates, Honorary Associate Professor, The University of Nottingham [13]
To maintain consistent oversight, align digital audits with clinical governance reviews [13]. For any digital incidents or breaches, document everything - timestamps, screenshots, and correspondence. This systematic approach supports digital forensics, aids recovery efforts, and provides clear evidence for reporting [13].
It's also important to recognize that systemic vulnerabilities and process gaps are often the root cause of digital incidents and adverse events - not individual mistakes [13]. When vendor failures occur, organizations should investigate broader system and process issues that allowed the failure to affect patient care. If negligence is involved, legal action can hold responsible parties accountable and encourage safer practices in the future [7].
Finally, healthcare organizations should establish clear stewardship for digital assets. This includes creating standard practices for managing professional accounts, documenting recovery protocols, and designating validation contacts [13]. These measures formalize accountability and ensure that lessons learned lead to improved practices over time.
FAQs
How can healthcare organizations identify and prioritize vendors that pose the highest risks to patient safety?
Healthcare organizations can better manage high-risk vendors by conducting thorough risk assessments. These evaluations should consider factors like how sensitive the data is, the level of system access provided, and the vendor's role in daily operations. Regularly reviewing vendors' security measures and examining potential weak points in the supply chain are also essential to staying ahead of potential issues.
By concentrating on vendors whose failures could disrupt services, cause errors, or lead to system downtime, organizations can take proactive steps to safeguard patient safety. Implementing a risk-based prioritization system helps ensure that resources are allocated to address the most pressing threats efficiently.
How can healthcare organizations reduce the impact of vendor-related data breaches on patient trust and care?
To minimize the risk of vendor-related data breaches, healthcare organizations need to take a proactive stance on cybersecurity. This means regularly performing risk assessments, setting up robust vendor management policies, and ensuring all vendors adhere to HIPAA regulations and cybersecurity standards.
It's also crucial to have well-defined incident response plans in place to handle breaches swiftly and efficiently. Ongoing staff training on cybersecurity best practices and closely monitoring vendor access to sensitive patient information are key measures to safeguard both patient trust and the quality of care.
What are the long-term effects of vendor failures on patient outcomes in healthcare?
Vendor issues in healthcare can have far-reaching consequences for patient care. When supply chains are disrupted, critical medical supplies and equipment may become scarce. This can lead to delayed treatments, limited access to necessary care, and even jeopardize patient safety.
On top of that, these disruptions can heighten the risk of problems like infections or medical errors, shaking confidence in the healthcare system. Consistent and dependable vendor performance plays a key role in delivering quality care and safeguarding patient health in the long run.


