Vendor Risk Management KPIs for Healthcare: Measuring Program Effectiveness
Post Summary
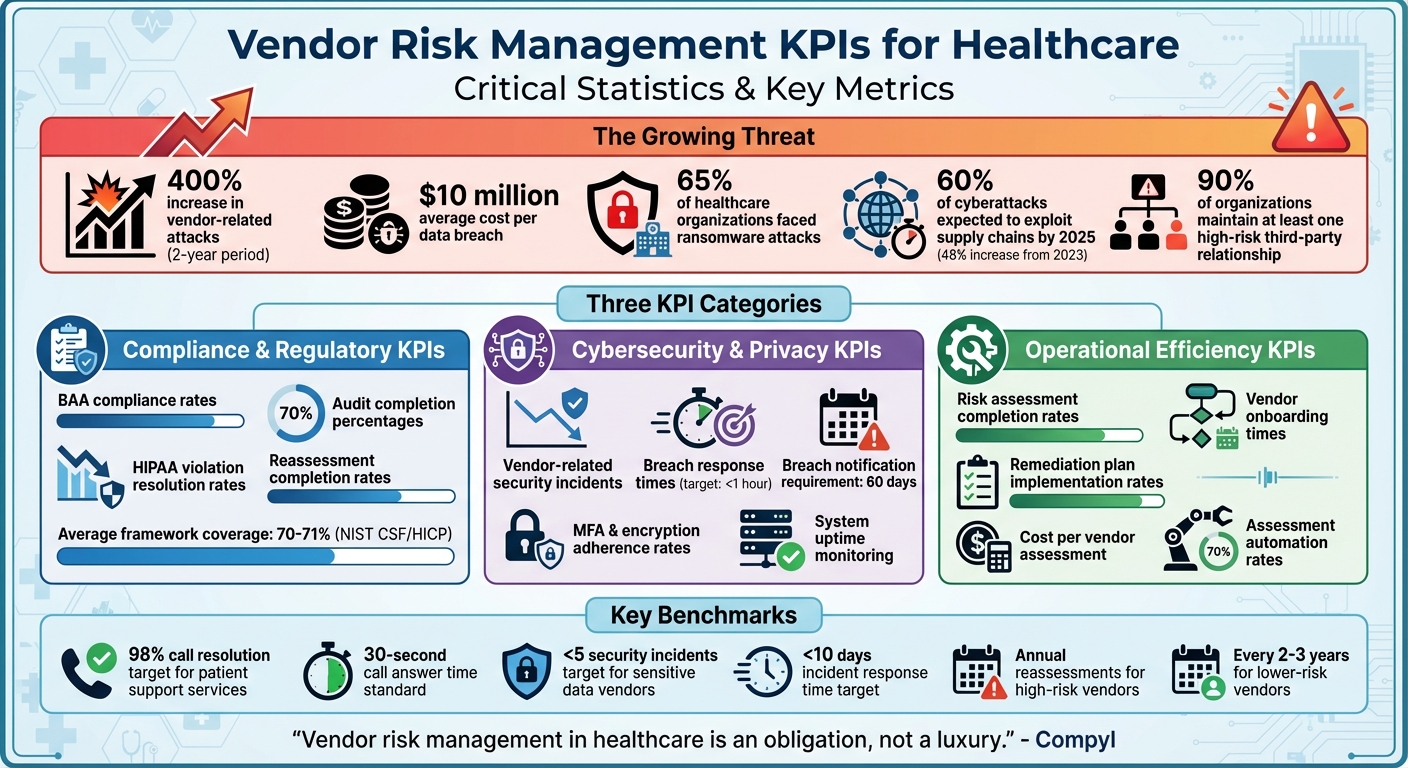
Healthcare organizations face growing risks from third-party vendors. From safeguarding patient data to complying with HIPAA and HITECH, vendor relationships require constant oversight. Key Performance Indicators (KPIs) are essential tools for measuring vendor risk management effectiveness, offering a clear way to track compliance, security, and operational performance.
Key Takeaways:
- Compliance KPIs: Measure audit completion rates, BAA compliance, and resolution of HIPAA violations.
- Cybersecurity KPIs: Track vendor-related security incidents, breach response times, and adherence to security protocols.
- Operational KPIs: Monitor risk assessment completion rates, vendor onboarding times, and remediation plan implementation.
With vendor-related attacks increasing by 400% and breaches costing nearly $10 million on average, healthcare providers must prioritize data-driven KPIs to mitigate risks and ensure patient safety. Automated tools and centralized platforms can simplify KPI tracking, enabling healthcare organizations to respond faster and reduce vulnerabilities effectively.
Healthcare Vendor Risk Management KPIs: Key Statistics and Metrics
Main Categories of Vendor Risk Management KPIs
In healthcare, vendor risk management KPIs fall into three primary categories: regulatory compliance, cybersecurity, and operational performance. These metrics are essential for safeguarding patient data and maintaining clinical operations.
Why does this matter? Vendor-related attacks have surged by over 400% in just two years, and the cost of an average data breach has skyrocketed to nearly $10 million. On top of that, more than 65% of healthcare organizations have faced at least one ransomware attack [2]. These staggering numbers highlight the urgent need for healthcare providers to monitor both immediate threats and long-term compliance requirements.
"Vendor risk management in healthcare is an obligation, not a luxury." - Compyl [2]
Let’s dive into each KPI category.
Compliance and Regulatory KPIs
Compliance KPIs ensure vendors meet legal and regulatory standards, including HIPAA and HITECH requirements. These metrics often cover vendor compliance rates, audit completion percentages, and the number of vendors with valid Business Associate Agreements (BAAs). Since HIPAA applies to third-party vendors as much as it does to healthcare entities, organizations are ultimately accountable for their vendors’ compliance [2].
But effective compliance tracking isn’t just about checking boxes. It involves monitoring violations found during audits, assessing the severity of those issues, and measuring the completion rate of corrective actions. Instead of relying on generic compliance declarations, healthcare organizations should demand concrete evidence, like detailed audit logs or certifications. Certifications such as HITRUST, SOC 2 Type 2 reports, or ISO 27001 provide a more reliable measure of ongoing compliance [2].
Cybersecurity and Privacy KPIs
Cybersecurity KPIs are critical for protecting sensitive patient data from breaches and cyberattacks. Key metrics include the number of vendor-related security incidents, breach response times, and adherence to security protocols like multi-factor authentication (MFA) and encryption. With ransomware incidents in hospitals doubling between 2022 and 2023, these KPIs have become indispensable [3].
To evaluate vendor security, many organizations use risk scorecards based on frameworks like the NIST Cybersecurity Framework. Monitoring system uptime for essential tools, such as electronic health record (EHR) systems, is also vital - downtime can directly impact patient care. Industry leaders aim for breach detection and response times under one hour, with the gold standard being near-instantaneous action. Regulations also require organizations to notify affected individuals within 60 days of discovering a breach, making timely reporting another critical metric [3].
Operational Efficiency and Risk Lifecycle KPIs
Operational KPIs assess the overall effectiveness of a vendor risk management program. Key metrics include risk assessment completion rates, onboarding times for high-risk vendors, and the implementation rates of remediation plans. These indicators help identify bottlenecks and streamline the risk management process.
For example, tracking risk assessments ensures that both security and compliance reviews are completed on schedule. Onboarding times for high-risk vendors should also be monitored to minimize delays in addressing potential vulnerabilities. Importantly, vendor risk assessments shouldn’t stop after initial onboarding. Instead, they should be performed regularly, with the frequency determined by the vendor’s risk level [2].
How to Define and Implement KPIs in Healthcare
Creating effective KPIs in healthcare requires a deep understanding of your operational needs and compliance obligations. These metrics should align with safeguarding patient information, adhering to HIPAA regulations, and evaluating vendor contributions to your goals. Here's how to approach it.
Aligning KPIs with Organizational Goals
Your KPIs should directly support your organization's primary objectives. Focus on the vendor relationships that have the biggest impact on critical areas like patient safety, compliance with regulations, and operational stability. Each KPI should tie back to one of these priorities to ensure measurable and meaningful outcomes. For example, if patient safety is a key focus, consider KPIs that measure timely care delivery or error reduction.
Setting KPI Definitions and Benchmarks
Once you've identified the KPIs, define how you'll measure them. Make sure they meet the S.M.A.R.T. criteria - Specific, Measurable, Achievable, Relevant, and Time-bound. Collaborate with your vendors to establish clear performance metrics and ensure they understand both your expectations and the risks involved.
"The key to setting valuable KPIs is to understand your organization's goals, work with the vendor, and think S.M.A.R.T." - Venminder Experts [1]
For example, in patient support services, you might set targets like resolving 98% of calls or answering calls within 30 seconds. For vendors managing sensitive data, metrics could include "fewer than five security incidents" or "incident response times under 10 days" [1]. Use historical data and industry standards to set realistic benchmarks, and establish strong data governance practices to maintain these standards.
Maintaining Data Accuracy and Governance
KPIs are only as good as the data behind them. Reliable and timely data is essential, so validate your sources regularly. Conduct routine audits to catch errors or inconsistencies early and to ensure vendors are providing complete and accurate information.
Assign clear roles for managing each KPI, including responsibilities for data collection and validation. This accountability ensures that your organization can trust the data driving its decisions and maintain compliance with healthcare regulations.
Top KPIs for Measuring Vendor Risk Program Performance
Keeping tabs on the right metrics is essential to gauge how well your vendor risk program safeguards your organization. Below are key performance indicators (KPIs) that provide insight into compliance, security, and operational efficiency. These metrics collectively help evaluate the program's overall health.
Regulatory and Compliance KPIs
Start by tracking BAA compliance rates, which show the percentage of vendors with up-to-date Business Associate Agreements. It's also critical to monitor HIPAA audit findings resolution rates, which measure how quickly vendors address compliance issues. Another key metric is reassessment completion rates, ensuring timely reviews - annually for high-risk vendors and every two to three years for lower-risk ones.
For context, the average coverage of NIST CSF and HICP in healthcare organizations is around 70%–71% [4]. Organizations using NIST CSF as their primary cybersecurity framework report smaller year-over-year increases in cybersecurity insurance premiums - about one-third of what non-NIST CSF organizations experience [4]. Moreover, higher adoption of Supply Chain Risk Management, a key part of NIST CSF's Identify function, is linked to lower increases in insurance premiums [4].
Security Incident and Remediation KPIs
Track the number of vendor-related security incidents annually to identify recurring issues or vendors that require closer scrutiny. Measure the average incident resolution time, comparing when an issue was first detected to when it was fully resolved, to evaluate responsiveness from both vendors and your internal team. Setting clear targets for resolving critical issues ensures timely action. Additionally, monitor the reduction in high-risk vendors over time to demonstrate that your program is effectively lowering risk exposure.
Operational Efficiency KPIs
Operational metrics build on compliance and security insights, offering a deeper look at how resources are used and processes are managed. Key metrics include the cost per vendor assessment, assessment automation rates, and due diligence completion times. These indicators help balance thoroughness with efficiency, ensuring your program is both effective and streamlined.
sbb-itb-535baee
Using Technology to Manage KPIs
Manually tracking vendor risk KPIs can be a tedious and error-prone process, often leading to inaccuracies that undermine the reliability of your data. Automated platforms offer a solution by pulling information directly from existing systems and providing real-time updates. These tools not only improve accuracy but also save time and resources by centralizing data streams into one cohesive system.
Centralizing KPI Data with Censinet RiskOps

Censinet RiskOps simplifies vendor risk management by acting as a centralized hub for all your data. It consolidates assessments, compliance documents, and related activities into a single platform, eliminating the need to sift through emails or shared drives. This streamlined approach ensures that KPIs - such as BAA compliance rates, reassessment completion rates, and vendor-related incident counts - are always up-to-date and reflect the true state of your vendor risk management efforts.
Automating KPI Measurement with Censinet AI

Censinet AI takes automation to the next level, dramatically speeding up the risk assessment process. Vendors can complete security questionnaires in seconds, not weeks, thanks to the AI’s ability to summarize evidence, document key details, and identify fourth-party exposures. It also generates detailed risk summary reports, making it easier to track metrics like assessment completion times and cost per vendor assessment. Importantly, automation doesn’t replace human involvement - it complements it. Risk teams still configure rules and review workflows to ensure that the technology supports informed decision-making. This combination of speed and oversight prepares data for effective visualization and actionable insights.
Visualizing KPIs with Dashboards
Dashboards transform complex data into clear, real-time insights. Executives can quickly gauge high-level trends, such as overall risk reduction or the percentage of vendors meeting compliance standards. Meanwhile, operational teams can dive into detailed work lists to address overdue assessments or unresolved security issues. Advanced features, like risk trend analysis and correlation, reveal hidden patterns and connections, enabling teams to shift from reacting to incidents to proactively preventing risks. These tools empower organizations to stay ahead in managing vendor risks effectively.
Conclusion
Healthcare organizations can no longer afford to treat vendor risk management as a simple checkbox exercise. With vendor attacks surging by over 400% and breaches averaging nearly $10 million, the need for a metric-driven approach has never been more urgent [2].
The stakes are even higher when considering that by 2025, more than 60% of cyberattacks are expected to exploit supply chain vulnerabilities - a sharp 48% increase from 2023 [6]. This alarming trend highlights the pressing need for swift and well-informed action.
To tackle these challenges, healthcare organizations must embrace data-driven decision-making. By focusing on measurable KPIs like compliance rates, incident response times, and assessment completion rates, organizations can shift from a reactive stance to a more strategic approach. These metrics provide the visibility needed to pinpoint weaknesses, allocate resources effectively, and deliver meaningful insights to leadership. As KPMG aptly points out, "While you may trust the third parties you work with, the risks associated with third-party interactions cannot be outsourced", emphasizing the importance of ongoing, data-informed oversight [6].
Technology plays a crucial role in this transformation. Automated tools streamline data collection and enable real-time KPI tracking, offering actionable insights as they happen. When paired with clear benchmarks, routine reassessments, and executive-level reporting, technology elevates vendor risk management from a compliance necessity to a strategic advantage.
Success lies in setting S.M.A.R.T. KPIs tailored to your organization’s specific risk landscape [1], embedding robust security clauses in vendor contracts [6], and taking immediate action when metrics signal an issue [5]. With nearly 90% of organizations maintaining at least one high-risk third-party relationship capable of causing a breach, the time to refine your measurement framework is now [6].
FAQs
What are the best practices for implementing vendor risk management KPIs in healthcare organizations?
Healthcare organizations can effectively manage vendor risks by tracking key performance indicators (KPIs) that align with their objectives. Metrics like vendor compliance rates, incident response times, and risk assessment completion rates are particularly useful. To make these KPIs impactful, they should be clear, measurable, and actionable.
Start by working closely with vendors to set clear expectations and establish dependable methods for gathering performance data. Regular reviews of these KPIs can help spot patterns and identify areas that need attention. Using the S.M.A.R.T. criteria - Specific, Measurable, Achievable, Relevant, and Time-bound - can ensure the metrics are practical and meaningful. Embedding these KPIs into vendor contracts or service-level agreements (SLAs) also promotes accountability and encourages better performance.
By keeping a close eye on these metrics and making adjustments as needed, healthcare organizations can reduce third-party risks, improve compliance, and bolster their cybersecurity defenses.
What’s the difference between compliance, cybersecurity, and operational KPIs in vendor risk management?
Compliance KPIs are essential for monitoring how effectively an organization follows regulations, internal policies, and industry standards. Examples of these metrics include audit completion rates, the number of policy violations, and vendor certification statuses - all of which help ensure accountability and adherence.
Cybersecurity KPIs zero in on safeguarding sensitive data and systems. Key metrics in this category include the number of security incidents, average response times to threats, and the percentage of vulnerabilities resolved. These indicators highlight how well an organization is managing its security risks.
Operational KPIs focus on the efficiency and reliability of processes. Metrics such as service availability, on-time delivery rates, and error or defect counts provide insight into how smoothly operations are running. When combined, these KPIs offer a well-rounded picture of vendor performance and the overall effectiveness of risk management strategies.
Why should healthcare organizations use automated tools to track vendor risk management KPIs?
Automated tools play a key role in tracking vendor risk management KPIs, offering real-time insights, minimizing human error, and speeding up data collection with greater precision. These tools empower healthcare organizations to keep a close eye on vendor compliance, response times to incidents, and other essential metrics with improved efficiency.
With automation, potential risks can be spotted earlier, regulatory requirements are easier to meet, and the organization’s cybersecurity defenses are bolstered. This efficient process not only saves valuable time but also helps uphold the rigorous standards that the healthcare industry demands.


