Vendor Risk vs. Industry Benchmarks: What to Measure
Post Summary
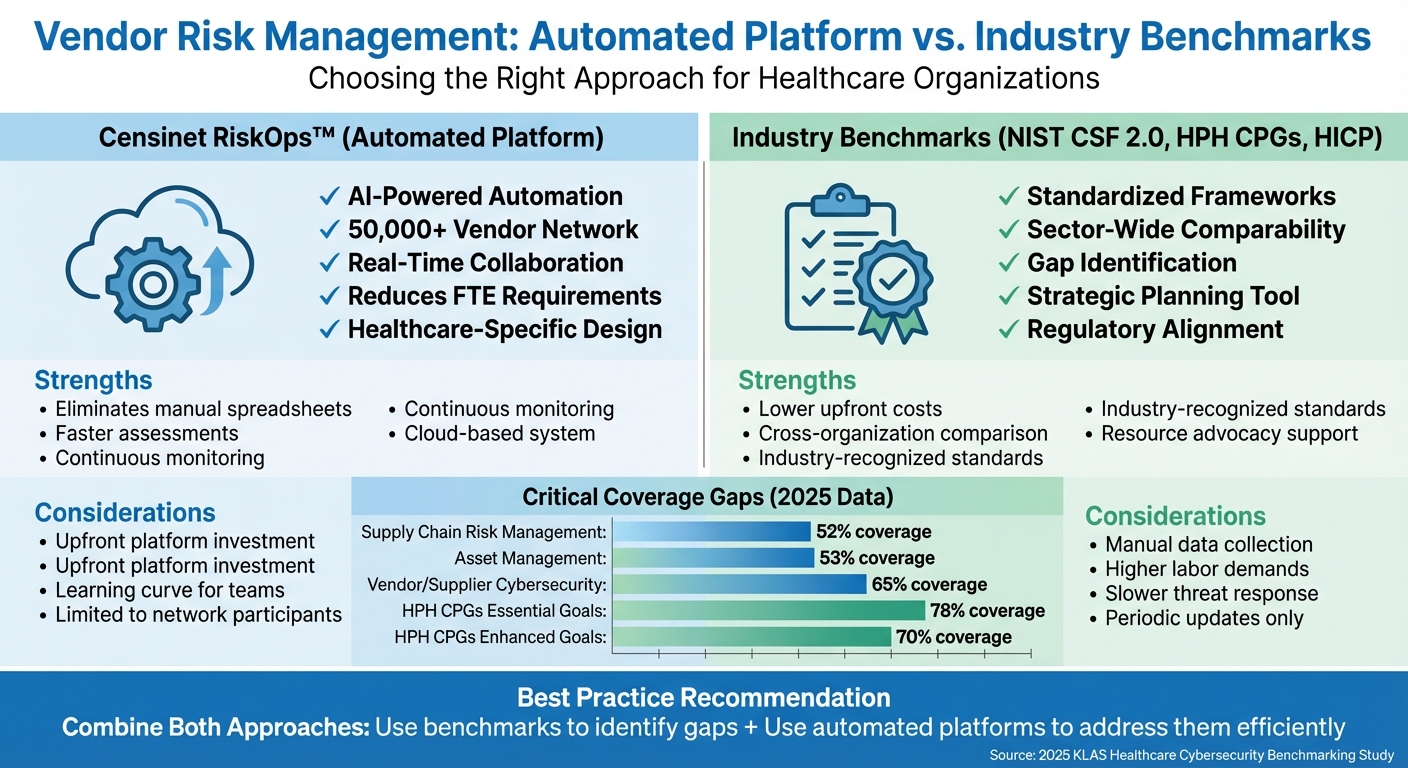
Benchmarks reveal cybersecurity gaps and help prioritize improvements.
It automates vendor assessments and provides real‑time collaboration across 50,000+ vendors.
NIST CSF 2.0, HPH CPGs, and HICP.
Only ~52% coverage of supply‑chain risk controls in NIST CSF 2.0.
Benchmarks identify weaknesses; automation fixes them faster and at scale.
Many devices have poor asset visibility and require specialized vendor controls.
Healthcare organizations face increasing challenges in managing vendor risks, especially with sensitive patient data and critical systems at stake. Key takeaway: Combining automated tools like Censinet RiskOps™ with frameworks such as NIST CSF 2.0, HPH CPGs, and HICP can improve vendor risk management while addressing security gaps. Here's how:
Quick Comparison:
Feature
Censinet RiskOps™
Industry Benchmarks
Automation
AI-powered, reduces manual effort
Manual data collection
Vendor Network
50,000+ vendors
Broader sector-wide scope
Resource Efficiency
Cuts FTE needs, upfront cost
Higher labor demands
The best approach? Use benchmarks to pinpoint weaknesses and platforms like Censinet to address them efficiently.
Censinet RiskOps vs Industry Benchmarks for Healthcare Vendor Risk Management
1. Censinet RiskOps™

Censinet RiskOps™ is a cloud-based risk exchange specifically designed to help healthcare organizations tackle vendor risk management challenges. By connecting healthcare delivery organizations with an extensive vendor ecosystem, it reshapes the way third-party risks are evaluated and managed, offering a more streamlined and effective approach [1].
Supply Chain Risk Management
One of the platform's standout features is its ability to close the supply chain risk management gap. According to the 2025 KLAS Healthcare Cybersecurity Benchmarking Study, only 52% of organizations currently achieve adequate supply chain risk coverage [4]. Censinet RiskOps™ addresses this by moving away from outdated, manual questionnaire-based assessments.
Terry Grogan, CISO at Tower Health, shared how the platform has improved efficiency:
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required."
By automating processes and enabling collaborative data sharing, the platform allows organizations to oversee vendors more effectively with fewer resources. Its AI-driven tools speed up tasks like completing security questionnaires and summarizing evidence, directly addressing the 65% gap in vendor and supplier cybersecurity requirements identified under the HPH CPG "Essential" goals [4].
In addition to enhancing supply chain resilience, RiskOps™ also streamlines broader vendor network management.
Vendor Network Management
RiskOps™ replaces cumbersome spreadsheet-based tracking with a centralized system for managing vendors. This collaborative approach fosters a sense of community among healthcare organizations. James Case, VP & CISO at Baptist Health, highlighted the benefits:
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with."
The platform also provides customizable risk scoring models, weighing factors like cybersecurity readiness, compliance with regulations (such as HIPAA, state privacy laws, and FDA medical device guidance), and data handling practices. Organizations can compare vendor performance against industry benchmarks to identify weaknesses and incorporate these insights into procurement and contract negotiations. This ensures a more informed and proactive approach to managing vendor risks.
2. Industry Benchmarks (NIST CSF 2.0, HPH CPGs, HICP)

Healthcare organizations rely on frameworks like NIST CSF 2.0, HPH CPGs, and HICP to establish clear cybersecurity benchmarks and pinpoint vendor risk gaps [4][2]. These standards not only help define internal expectations but also provide a foundation for evaluating vendor performance.
Supply Chain Risk Management
The updated NIST CSF 2.0 introduces a "Govern" function, which emphasizes supply chain oversight. Despite this, the average coverage for this function stands at just 52%, highlighting a major vulnerability [4].
The HPH CPGs outline Essential and Enhanced performance goals, with vendor and supplier cybersecurity requirements showing the lowest Essential-goal coverage at 65% [4]. This indicates that many healthcare organizations struggle to enforce baseline cybersecurity standards across their supply chain. Such gaps can leave sensitive data, like protected health information (PHI), and critical services exposed. Addressing these shortcomings is crucial for creating consistent and effective vendor risk management practices.
Medical Device Security
The HICP framework tackles key cyber threats - such as ransomware, phishing, and medical device vulnerabilities - by offering practical, threat-based controls [4]. These controls align with NIST CSF standards and extend to device manufacturers and vendors. By benchmarking medical device vendors against HICP practices, organizations can evaluate compliance with secure configuration requirements, patching protocols, and system logging standards.
However, asset management - a critical component for tracking medical devices and their associated vendors - shows only 53% coverage within NIST CSF 2.0's Identify function [4]. This low score reveals a lack of centralized visibility into vendor-linked critical assets, complicating risk assessments for medical device suppliers. Strengthening asset tracking and aligning these insights with vendor risk management are essential steps for improved security.
Data Protection and Loss Prevention
When using HPH CPGs as a benchmark, organizations report an average of 78% coverage of Essential goals and 70% coverage of Enhanced goals [4]. However, gaps in vendor and supplier cybersecurity requirements can hinder consistent data protection for PHI, clinical applications, and other sensitive patient information.
The HHS Spring 2025 Report underscores the financial benefits of rigorous vendor benchmarking. For instance, Medicare Advantage plans reduced $7.5 billion in risk exposure by adopting HICP-like frameworks that included real-time monitoring and clinical validation [5].
Vendor Network Management
A 2025 KLAS study highlights third-party risk and asset management as areas needing improvement across both NIST CSF 2.0 and HPH CPGs [2]. Many healthcare entities still take a reactive approach rather than leveraging these frameworks to maintain continuous vendor oversight. Developing a centralized inventory of vendors tied to critical assets - such as electronic health records (EHRs), imaging systems, clinical applications, and medical devices - enables organizations to map vendors to specific NIST CSF categories and HPH CPG control areas. This approach supports more focused and effective assessments [3].
Here’s a summary of key benchmark areas for vendor risk comparisons:
Benchmark Area
2025 Average Coverage
Framework Source
Supply chain risk management
NIST CSF 2.0 (Govern)
Asset management
NIST CSF 2.0 (Identify)
Vendor/supplier cybersecurity requirements
HPH CPGs
sbb-itb-535baee
Advantages and Disadvantages
Let’s delve into the trade-offs between Censinet RiskOps™ and industry benchmarks, focusing on how each approach aligns with resources, organizational maturity, and operational goals.
Censinet RiskOps™ stands out for its automation and efficiency. By leveraging AI-driven assessments and a cloud-based system, it eliminates the need for manual tasks like chasing down questionnaires or managing spreadsheets. With a network of over 50,000 vendors [1], it offers real-time collaboration and continuous risk management. However, adopting this platform requires upfront investment and may involve a learning curve for teams accustomed to traditional methods.
On the other hand, industry benchmarks - such as NIST CSF 2.0, HPH CPGs, and HICP - provide standardized frameworks that can be applied across various healthcare organizations. These benchmarks help teams identify gaps and advocate for resources by comparing their practices against sector-wide standards. For instance, a 2025 KLAS study involving 69 organizations revealed that benchmarks exposed critical gaps, like only 52% coverage in supply chain risk management [2][4]. While benchmarks are invaluable for strategic planning, their application often demands manual interpretation and can be slower to respond to new threats.
Here’s a side-by-side look at the key differences:
Aspect
Censinet RiskOps™
Industry Benchmarks
AI-powered, reducing manual effort
Relies on manual data collection and analysis
Designed for patient data, PHI, and medical devices
Generic frameworks that may need customization
Cloud-based system linking over 50,000 vendors
Static guidelines updated periodically
Cuts down on FTE needs but requires platform investment
Lower upfront costs but higher ongoing labor demands
Limited to network participants
Enables sector-wide benchmarking
This comparison can help organizations decide how best to align their vendor risk strategies with their specific needs.
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare."
These words from Matt Christensen, Sr. Director GRC at Intermountain Health, highlight a critical challenge [1]. Combining both approaches - using benchmarks to pinpoint priority areas and platforms like Censinet RiskOps™ to address those areas efficiently - can create a well-rounded vendor risk management strategy.
Conclusion
Managing vendor risk in healthcare demands careful planning and a balanced approach. With breach costs averaging between $7 million and $10 million, healthcare organizations cannot afford to overlook the importance of accurate vendor assessments [5]. The real challenge lies not in picking between automated tools and established benchmarks but in understanding how each plays a unique role in a comprehensive risk management strategy.
This is where Censinet RiskOps™ steps in to ease the operational load. By automating vendor assessments across a network of more than 50,000 vendors, it eliminates the tedious tasks of managing spreadsheets and chasing down questionnaires [1]. This level of automation boosts efficiency, enabling teams to complete more assessments with fewer resources while maintaining consistency and quality.
On the strategic side, industry benchmarks such as NIST CSF 2.0 and HPH CPGs provide clear, actionable guidance. These frameworks help organizations prioritize their efforts, ensuring limited resources are allocated effectively. For many, this means dedicating 3-7% of their IT budgets to robust vendor risk programs [5].
The strongest strategies combine these two elements. By using benchmarks to pinpoint vulnerabilities and automated solutions to address them, healthcare organizations can achieve continuous, compliant vendor risk management. This approach ensures the protection of patient data, medical devices, and supply chain operations while optimizing resources and maintaining high standards.
FAQs
How does Censinet RiskOps™ help healthcare organizations manage vendor risks more effectively?
Censinet RiskOps™ transforms vendor risk management for healthcare organizations by utilizing AI-driven continuous risk assessments. This advanced platform cuts down on manual tasks, optimizes workflows, and delivers actionable insights by comparing performance to industry benchmarks.
With Censinet RiskOps™, healthcare providers can efficiently pinpoint vulnerabilities, prioritize necessary improvements, and strengthen their cybersecurity defenses. It plays a crucial role in protecting sensitive areas such as patient data, clinical systems, medical devices, and supply chains, creating a safer and more compliant operational environment.
How does Censinet RiskOps™ compare to industry benchmarks for managing vendor risks?
Censinet RiskOps™ is purpose-built for healthcare organizations, offering AI-driven tools for risk management and continuous assessments. These tools address the unique challenges of the healthcare sector by simplifying workflows, automating key processes, and fostering collaboration to manage vendor risks more effectively.
Traditional industry benchmarks may provide general guidelines for evaluating vendor risks, but they often fall short when it comes to real-time data, automation, and a healthcare-specific approach. Censinet RiskOps™ bridges this gap by helping organizations pinpoint vulnerabilities, prioritize necessary improvements, and protect critical assets like patient information, clinical systems, and supply chains.
Why should healthcare organizations use automated tools alongside industry benchmarks for vendor risk management?
Healthcare organizations can better manage vendor risks by combining automated tools with industry benchmarks. This strategy enables ongoing identification of vulnerabilities, more efficient risk assessments, and targeted improvements driven by real-time data and specific metrics.
By integrating automation and benchmarking, organizations can strengthen their cybersecurity defenses, focus on addressing the most critical risks, and stay aligned with industry standards. This approach is crucial for safeguarding sensitive patient information, addressing third-party risks, and ensuring the smooth operation of clinical systems and supply chains.
Related Blog Posts
- Healthcare Vendor Breach Response: Best Practices
- Building Vendor Risk Frameworks for Healthcare IT
- Healthcare Benchmark Study Reveals Vendor Risk Management Consumes 20% of IT Resources
- Key Metrics for Vendor Risk Dashboards
{"@context":"https://schema.org","@type":"FAQPage","mainEntity":[{"@type":"Question","name":"How does Censinet RiskOps™ help healthcare organizations manage vendor risks more effectively?","acceptedAnswer":{"@type":"Answer","text":"<p>Censinet RiskOps™ transforms vendor risk management for healthcare organizations by utilizing <strong>AI-driven continuous risk assessments</strong>. This advanced platform cuts down on manual tasks, optimizes workflows, and delivers actionable insights by comparing performance to industry benchmarks.</p> <p>With Censinet RiskOps™, healthcare providers can efficiently pinpoint vulnerabilities, prioritize necessary improvements, and strengthen their cybersecurity defenses. It plays a crucial role in protecting sensitive areas such as patient data, clinical systems, medical devices, and supply chains, creating a safer and more compliant operational environment.</p>"}},{"@type":"Question","name":"How does Censinet RiskOps™ compare to industry benchmarks for managing vendor risks?","acceptedAnswer":{"@type":"Answer","text":"<p>Censinet RiskOps™ is purpose-built for healthcare organizations, offering <strong>AI-driven tools for risk management</strong> and continuous assessments. These tools address the unique challenges of the healthcare sector by simplifying workflows, automating key processes, and fostering collaboration to manage vendor risks more effectively.</p> <p>Traditional industry benchmarks may provide general guidelines for evaluating vendor risks, but they often fall short when it comes to <strong>real-time data, automation, and a healthcare-specific approach</strong>. Censinet RiskOps™ bridges this gap by helping organizations pinpoint vulnerabilities, prioritize necessary improvements, and protect critical assets like patient information, clinical systems, and supply chains.</p>"}},{"@type":"Question","name":"Why should healthcare organizations use automated tools alongside industry benchmarks for vendor risk management?","acceptedAnswer":{"@type":"Answer","text":"<p>Healthcare organizations can better manage vendor risks by combining automated tools with industry benchmarks. This strategy enables ongoing identification of vulnerabilities, more efficient risk assessments, and targeted improvements driven by real-time data and specific metrics.</p> <p>By integrating automation and benchmarking, organizations can strengthen their cybersecurity defenses, focus on addressing the most critical risks, and stay aligned with industry standards. This approach is crucial for <a href=\"https://censinet.com/perspectives/8-best-practices-for-patient-data-protection\">safeguarding sensitive patient information</a>, addressing third-party risks, and ensuring the smooth operation of clinical systems and supply chains.</p>"}}]}
Key Points:
Why should healthcare organizations benchmark vendor risk?
- Reveals systemic gaps in supply‑chain security
- Supports resource justification using measurable weaknesses
- Aligns vendor expectations with national cybersecurity standards
- Improves defensibility during audits, oversight, or OCR investigations
How does Censinet RiskOps™ improve vendor risk management?
- AI‑powered automation reduces manual assessment work
- Shared vendor assessments shorten onboarding time
- Centralized vendor profiles eliminate spreadsheets
- Customizable risk scoring aligns to PHI handling and clinical criticality
What do NIST CSF 2.0 and HPH CPGs expose about supply‑chain risks?
- NIST CSF 2.0 “Govern” function shows only ~52% supply‑chain coverage
- HPH CPG Essential goals show only 65% vendor‑security requirement coverage
- Asset visibility remains weak, especially for medical devices
- Poor subcontractor transparency continues to create hidden risk
How do benchmarks improve medical device vendor oversight?
- HICP threat‑based controls highlight required security baselines
- NIST Identify/Protect functions map to device patching, configurations, and logging
- Asset tracking gaps (~53%) reveal missing visibility into device inventories
- Benchmarking ensures compliance across manufacturers and device suppliers
What advantages do automated platforms offer over manual frameworks?
- Continuous monitoring instead of annual reviews
- Real‑time evidence updates for SOC 2, certifications, and incidents
- AI‑driven questionnaire completion accelerates vendor responses
- Collaboration networks reduce duplicated assessments across organizations
Why combine benchmarks with automated TPRM platforms?
- Benchmarks show what “good” looks like
- Platforms operationalize those standards through alerts and workflows
- Automation reduces FTE load, freeing teams for higher‑value work
- Benchmark‑guided scoring strengthens procurement decisions


