How Vendor Risks Impact Compliance
Post Summary
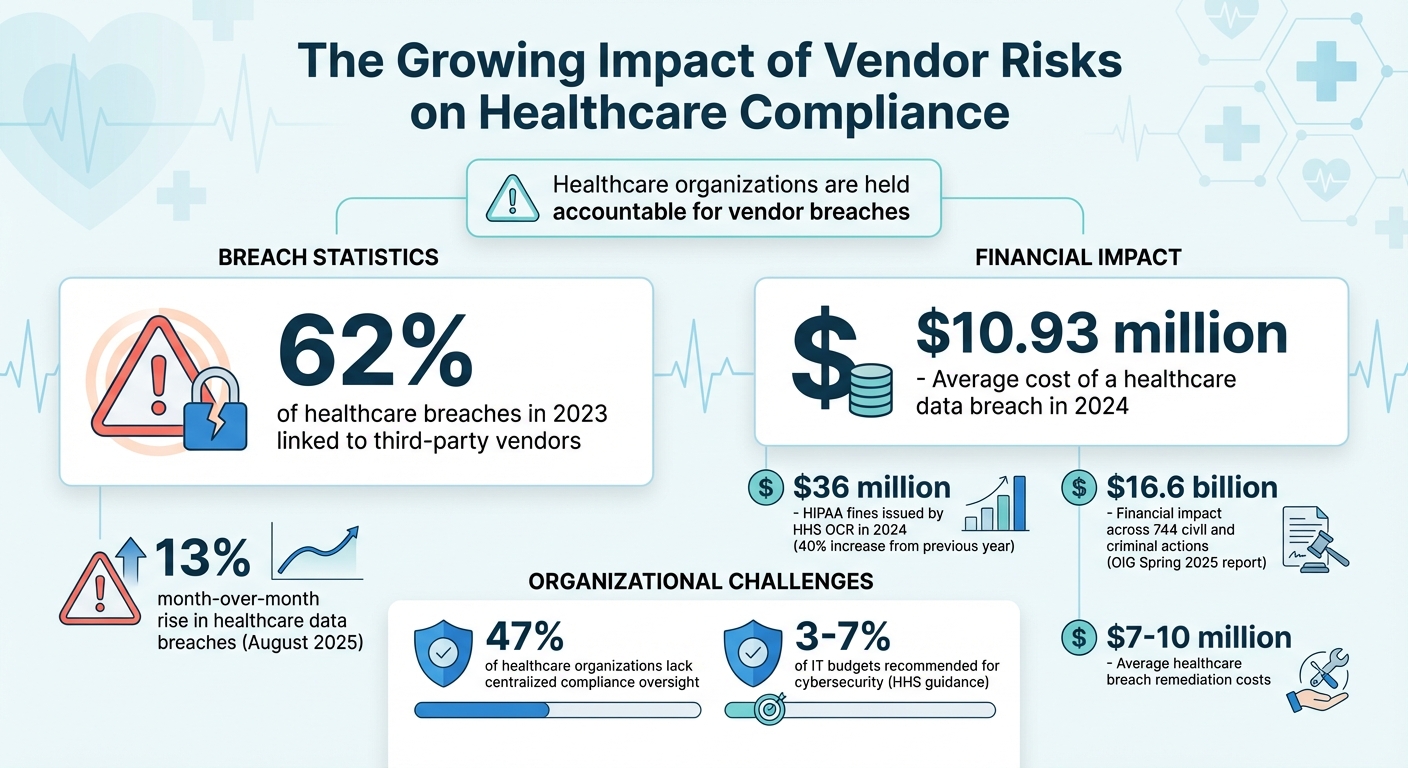
Vendor risks are a growing challenge for healthcare organizations, directly affecting compliance with regulations like HIPAA, HITECH, and CMS Conditions of Participation. If a vendor fails to secure patient data or experiences a breach, the healthcare provider is still held accountable. With 62% of healthcare breaches in 2023 linked to third-party vendors and HIPAA fines reaching $36 million in 2024, managing these risks is no longer optional.
Key takeaways:
- Third-party risks are everywhere: From EHR providers to cloud platforms, vendors introduce vulnerabilities that can lead to compliance failures.
- Regulations demand accountability: Healthcare organizations are responsible for vendor oversight, including risk assessments and breach reporting.
- Financial stakes are high: The average cost of a healthcare data breach reached $10.93 million in 2024.
- Common issues include: Poor access controls, shared credentials, and lack of continuous monitoring.
- Solutions focus on better reporting: Implementing tools like Censinet RiskOps™ can automate assessments, track risks, and provide real-time insights.
Managing vendor risks requires a clear inventory of vendors, standardized assessments, and continuous monitoring to stay ahead of compliance challenges.
Healthcare Vendor Risk Statistics and Compliance Costs 2023-2024
How Vendor Risks Lead to Compliance Failures
In the healthcare sector, vendor vulnerabilities can lead to regulatory violations, enforcement actions, and operational disruptions. Understanding how these risks arise is crucial for healthcare organizations aiming to pinpoint the weakest areas in their compliance programs. Let’s dive into some specific vulnerabilities that often result in compliance challenges.
Common Vendor Network Weaknesses
One recurring issue is poor access controls. Many healthcare organizations fail to revoke a vendor's access when contracts end, support tickets close, or personnel changes occur. These dormant accounts can become easy targets for unauthorized access.[2] Another major problem is the use of shared credentials and shadow IT - when individual departments engage vendors without going through proper security reviews. This lack of oversight creates blind spots in the organization's risk management process.
Fourth-party risks add another layer of complexity. Vendors often rely on subcontractors or cloud providers, introducing additional risks. These extended networks mean a single weak link can cascade into broader security threats. Unfortunately, traditional risk assessments often fail to capture these downstream vulnerabilities, leaving organizations exposed.
These gaps don’t just create theoretical risks - they often result in tangible compliance violations.
Compliance Violations Caused by Vendor Risks
Weak vendor security practices can lead to specific violations of regulations like HIPAA, which regulators actively enforce. Regulatory fines are a stark reminder of the consequences of overlooking vendor assessments. When vendors lack proper safeguards, healthcare organizations are held accountable for breaches of the Security Rule.
One common issue involves Business Associate Agreement (BAA) breaches. Vendors are required to protect patient health information, follow breach notification timelines, and report security incidents. When they fail to meet these obligations, both the vendor and the healthcare organization can come under regulatory scrutiny. The OIG’s Spring 2025 report revealed a staggering $16.6 billion in financial impact across 744 civil and criminal actions, highlighting the severe monetary risks of compliance failures.[3]
Beyond data privacy, vendor risks can jeopardize patient safety and clinical operations. For instance, disruptions in EHR access, malfunctioning medical devices, or compromised clinical decision support systems can lead to violations of standards set by The Joint Commission and CMS Conditions of Participation. Even if these issues originate with a vendor, healthcare organizations bear the responsibility for maintaining safe, continuous care delivery. Accreditation and participation status may be at risk.
Reporting Failures That Create Exposure
Inconsistent or inadequate risk assessments often prevent organizations from spotting vendor vulnerabilities before they escalate. Many healthcare teams rely on unstructured spreadsheets to track vendor responses, leading to incomplete evaluations and missed warning signs. Without standardized scoring models, it becomes nearly impossible to compare vendor risks or prioritize remediation efforts effectively.
"You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare." - Matt Christensen, Sr. Director GRC, Intermountain Health[1]
Another critical gap is the lack of continuous monitoring. Vendors may change their security practices, introduce new subcontractors, or experience incidents without reporting them. Without up-to-date data, compliance teams risk relying on outdated information, which can undermine their ability to demonstrate due diligence. This disconnect between risk assessments and real-time conditions opens the door to enforcement actions.[2][3]
Building Effective Vendor Risk Reporting Programs
The compliance failures mentioned earlier don’t have to be a given. Healthcare organizations can implement structured vendor risk reporting systems that meet regulatory standards while offering real-time insight into potential risks. It all begins with knowing exactly who your vendors are and understanding the risks they bring to the table.
Creating a Comprehensive Vendor Inventory
To tackle compliance challenges head-on, building a thorough vendor inventory is a must. This inventory should detail vendor names, contract specifics, access methods, data flows, and the roles each vendor plays - whether they handle PHI, support clinical systems, or manage medical devices. Without this foundation, assessing risk and demonstrating accountability to auditors becomes nearly impossible.
One common challenge is the presence of vendors operating outside of formal procurement channels, often through shadow IT. To address this, healthcare organizations can use platforms that tap into collaborative risk networks, simplifying the inventory process by utilizing existing vendor data. For instance, Censinet RiskOps™ leverages a network of over 50,000 vendors and products in the healthcare sector, enabling organizations to quickly identify and document their vendor relationships.[1]
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with." - James Case, VP & CISO, Baptist Health[1]
Transitioning from manual tracking to centralized, data-driven platforms allows organizations to maintain accurate and current vendor inventories, which are critical for compliance.
Standardizing Risk Assessments and Reporting
Once a detailed inventory is in place, the next step is to standardize how vendor risks are assessed and reported. Frameworks like NIST CSF, HITRUST, and ISO 27001 offer structured methods that bring consistency to risk evaluations. Standardized reporting tools - such as executive summaries, heat maps, and scorecards - help compliance leaders, security teams, and board members clearly understand the most pressing vendor risks and how they’re being managed.[2][3]
Streamlining these processes also boosts efficiency.
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required." - Terry Grogan, CISO, Tower Health[1]
By replacing disorganized spreadsheets with purpose-built platforms, healthcare organizations can handle more assessments without sacrificing quality.
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." - Brian Sterud, CIO, Faith Regional Health[1]
Using recognized frameworks not only demonstrates diligence to regulators but also supports the case for investing in cybersecurity. This is particularly critical as the Department of Health and Human Services (HHS) recommends allocating 3–7% of IT budgets to cybersecurity, with healthcare breach remediation costs averaging $7–10 million.[3]
With standardized processes in place, the focus must shift to keeping vendor risk data up to date.
Implementing Continuous Monitoring
Annual risk assessments are no longer enough. Vendor practices and subcontractor arrangements can change quickly, making continuous monitoring essential. Automated alerts, periodic reassessments, and real-time data sharing ensure compliance teams have up-to-date information and can act swiftly to address new risks.[2][3]
HHS now emphasizes real-time monitoring of vendor-submitted data and rigorous due diligence, especially for high-risk programs like Medicare Advantage risk adjustment.[3] Triggers such as vendor security incidents, subcontractor changes, or negative media reports should prompt immediate risk reviews. Cloud-based risk exchanges and collaborative networks make it easier for healthcare organizations and vendors to share data, enabling a shift from static assessments to dynamic risk management.[1]
Platforms designed specifically for ongoing risk reduction allow organizations to adapt to changes in resources, budgets, and workforce, ensuring vendor risk reporting remains aligned with compliance requirements over time.
sbb-itb-535baee
Using Technology for Vendor Risk Management
Manually tracking vendor risks just doesn't cut it anymore. With 62% of healthcare breaches in 2023 linked to third-party vendors and the average cost of a healthcare data breach expected to hit $10.93 million in 2024[2], healthcare organizations need the right technology to keep up with ever-changing threats and strict regulations.
Streamlining Assessments with Censinet RiskOps™

Censinet RiskOps™ is an AI-powered risk management platform designed to automate vendor risk assessments. It taps into a network of over 50,000 vendors and products to collect and store key compliance documents like BAAs, SOC 2 Type 2 reports, HITRUST certifications, incident response plans, encryption standards, and insurance records. Each document is tied to specific regulatory requirements, such as HIPAA Security Rule standards or HITECH provisions[4][5]. This level of automation ensures that risk documentation is accurate and always up to date.
This shift from manual to automated workflows is critical, considering that 47% of healthcare organizations lack centralized compliance oversight across their systems[2]. Automating these processes not only saves time but also reduces the risk of non-compliance.
Improving Visibility and Collaboration
Centralized dashboards provide real-time insights into vendor risks. Tools like heat maps and scorecards make it easy to pinpoint the vendors with the highest risk and prioritize remediation efforts. The platform also offers benchmarking capabilities, allowing organizations to compare their cybersecurity posture against industry standards. This can be a game-changer when advocating for cybersecurity budgets, especially since the Department of Health and Human Services (HHS) recommends allocating 3–7% of IT budgets to cybersecurity[3].
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters."
– Brian Sterud, CIO, Faith Regional Health[1]
Collaboration is another area where the platform shines. Instead of requiring vendors to fill out the same questionnaires for multiple organizations, Censinet Connect™ lets them share completed security assessments and documentation across the network. This not only makes the process smoother for vendors but also allows for continuous monitoring of any changes in vendor practices, subcontractor arrangements, or security incidents - all in real time[1].
The result? Enhanced visibility and audit-ready documentation with minimal friction.
Generating Audit-Ready Compliance Documentation
Visibility and proactive monitoring naturally lead to better documentation. When auditors from the OCR or CMS come knocking, healthcare organizations need to show clear, systematic oversight of their vendors. Censinet RiskOps™ helps by generating detailed reports for each vendor, including assessments performed, dates, responsible parties, control results, residual risk ratings, and documented remediation steps - all mapped to specific regulatory requirements[4][5].
The platform also keeps a detailed log of every key action - whether it's issuing assessments, tracking vendor responses, approving risks, or handling exceptions. This comprehensive audit trail ensures organizations can demonstrate due diligence, reducing the risk of penalties. It's worth noting that HIPAA violation fines issued by HHS OCR reached $36 million in 2024, a 40% increase from the previous year, largely due to insufficient risk assessments and delayed breach notifications[2].
For high-stakes programs like Medicare Advantage risk adjustment, where HHS emphasizes real-time monitoring and rigorous oversight of vendor-submitted data, the platform offers tools to track submissions, reconcile activity with clinical data, and document oversight decisions[3]. This capability is especially crucial given the 13% month-over-month rise in healthcare data breaches in August 2025, driven by ransomware attacks[3][6]. By staying audit-ready year-round, organizations can focus on reducing risks instead of scrambling to prepare documentation when it's too late.
Conclusion
Benefits of Better Vendor Risk Reporting
Vendor risk reporting plays a crucial role in ensuring patient safety and maintaining the resilience of healthcare organizations. By adopting structured reporting frameworks, organizations gain real-time insights into vendor activities and improve overall operational efficiency. Consider this: 62% of healthcare breaches in 2023 were tied to third-party vendors, and the average cost of a breach is projected to reach a staggering $10.93 million in 2024[2]. These numbers highlight the immense financial and reputational risks at stake.
A strong reporting system does more than just mitigate risks - it streamlines operations. With a robust program, organizations can perform more assessments with fewer resources, eliminate time-consuming manual processes, and produce audit-ready documentation that satisfies regulatory requirements. This not only saves money but also frees up security teams to focus on strategic priorities instead of administrative burdens.
Better reporting also empowers healthcare leaders to secure the resources they need. By benchmarking their cybersecurity posture against industry standards and identifying gaps in vendor oversight, they can present compelling arguments for budget increases. This is particularly important as the Department of Health and Human Services (HHS) suggests allocating 3–7% of IT budgets to cybersecurity[3].
Given these advantages, it’s clear that healthcare organizations must act decisively to strengthen their vendor risk management practices.
Next Steps for Healthcare Organizations
To harness the benefits of robust vendor risk reporting, healthcare organizations should take three essential steps:
- Create a complete vendor inventory: Ensure every third party with access to patient data, systems, or facilities is accounted for.
- Standardize risk assessments: Use frameworks aligned with regulatory requirements like HIPAA, HITECH, and state privacy laws.
- Adopt continuous monitoring: Focus on ongoing oversight for high-risk vendors instead of relying on annual reviews.
Platforms like Censinet RiskOps™ can simplify these processes by automating vendor assessments, centralizing documentation, and offering real-time dashboards that provide a clear view of risks across the organization. With HIPAA fines reaching $36 million in 2024 - a 40% jump from the previous year[2], and regulators putting more pressure on vendor oversight, manual risk management is no longer a viable option. Now is the time to align your risk reporting practices with compliance requirements and protect your organization from escalating threats.
FAQs
How can healthcare organizations effectively manage vendor risks to ensure compliance?
To manage vendor risks and ensure compliance, healthcare organizations should begin with detailed risk assessments for all vendors. This process helps pinpoint vulnerabilities tied to patient data, clinical systems, and supply chains.
Ongoing monitoring plays a key role here. Tools like Censinet RiskOps™ can simplify assessments while offering real-time insights. Beyond that, organizations should implement solid risk mitigation plans, enforce strict compliance policies, and foster open communication with vendors to address issues together. Regularly updating these practices to align with industry standards and new threats keeps the approach proactive and effective.
How does continuous vendor monitoring help healthcare organizations stay compliant?
Continuous vendor monitoring plays a crucial role in helping healthcare organizations stay compliant by providing real-time insights into vendor-related risks. This forward-thinking approach enables organizations to spot and address potential problems early, ensuring they meet regulatory standards like HIPAA and HITRUST.
By simplifying risk assessments and automating essential tasks, continuous monitoring eases the burden of manual work. It also boosts the organization’s ability to handle vulnerabilities effectively. Beyond compliance, this approach protects vital areas such as patient data, clinical systems, and medical devices, ensuring they remain secure and reliable.
How do vendor compliance failures financially impact healthcare organizations?
When vendors in healthcare fail to meet compliance standards, the financial consequences can be staggering. Organizations could face hefty fines, legal penalties, and significant expenses tied to remediation efforts and operational changes. For instance, breaches of regulations like HIPAA can result in fines that climb into the millions, not to mention the costs of addressing the breach and implementing corrective actions.
The financial impact doesn’t stop there. Non-compliance can severely tarnish an organization’s reputation, undermine patient trust, and even lead to lawsuits. These ripple effects often compound the financial burden, underscoring the importance of proactive vendor risk management to protect both regulatory compliance and financial health.


