Best Practices for Third-Party Data Exchange Security
Post Summary
It refers to the strategies and practices used to protect sensitive data shared between organizations and third-party vendors.
It prevents data breaches, ensures compliance with regulations, and protects sensitive information like PHI and PII.
Risks include data breaches, lack of encryption, poor vendor security practices, and insufficient monitoring.
Best practices include vendor risk assessments, data encryption, continuous monitoring, and implementing strong contractual agreements.
Frameworks like SOC 2, ISO 27001, and HIPAA ensure vendors meet security and privacy standards
Tools like Censinet RiskOps™ automate risk assessments, monitor vendor security, and ensure compliance.
- Zero Trust and Least Privilege: Always verify identities and limit access to only what’s necessary.
- Defense in Depth: Use layers of security like encryption, HTTPS, and multi-factor authentication.
- Continuous Risk Management: Regularly monitor vendors and update security measures as threats evolve.
- Authentication and Authorization: Implement standards like OAuth 2.0 and SMART on FHIR for secure access.
- Session and Token Security: Use short-lived tokens, enforce TLS, and monitor for suspicious activity.
- Encryption and Data Integrity: Encrypt data during transport, use digital signatures, and verify integrity.
- Vendor Governance: Vet vendors thoroughly, enforce strong contracts, and monitor compliance continuously.
- Monitoring and Incident Response: Centralize logs, detect anomalies, and collaborate on response plans.
Healthcare organizations must prioritize secure third-party integrations to ensure accurate data, protect PHI, and maintain trust in clinical workflows. Tools like Censinet RiskOps™ can help streamline risk assessments and vendor oversight.
Core Security Principles for Third-Party Data Exchange
Protecting third-party data exchange in healthcare hinges on three main principles: Zero Trust, defense in depth, and continuous risk management. These frameworks shape how organizations verify identities, layer security measures, and maintain vigilance as clinical integrations grow more complex. Let’s break down how each principle strengthens healthcare data security.
Zero Trust and Least Privilege
Zero Trust is built on a clear idea: assume nothing, verify everything. Every user, device, and third-party must continuously prove their identity and authorization - whether they’re inside or outside the network. This mindset is especially critical as healthcare organizations increasingly rely on API-driven interoperability using FHIR and SMART on FHIR standards.
In practice, Zero Trust for third-party integrations means enforcing standards-based authentication protocols like OAuth 2.0 and OpenID Connect for every API request. For instance, a cloud-based patient engagement app must authenticate itself and obtain tokens with narrowly defined scopes, ensuring it can access only the data it needs.
The least privilege principle works hand-in-hand with Zero Trust. It ensures that each integration is granted only the minimal permissions required to function. For example, a billing service might only access procedure codes and insurance details, limiting exposure in case of a breach. By restricting access, this approach contains potential damage if a vendor account is compromised.
Defense in Depth
Defense in depth takes a layered approach to security, applying protections across multiple areas - like networks, applications, identities, and data. This way, even if one layer fails, others remain in place to safeguard sensitive information. Key measures include HTTPS with TLS for secure communication, API gateways, multi-factor authentication, and encryption. Techniques like cryptographic checksums and digital signatures further ensure data integrity and authenticity.
This multi-layered strategy also extends to vendor governance. Healthcare entities must hold their business associates accountable by requiring robust safeguards through Business Associate Agreements and maintaining continuous oversight of their security practices.
Continuous Risk Management
Third-party risk isn’t static - it evolves as vendors update systems, new vulnerabilities surface, and cyber threats grow more sophisticated. Continuous risk management recognizes that a one-time security assessment at the start of a contract isn’t enough to protect clinical integrations over the long haul.
To stay ahead, healthcare organizations need to consistently monitor vendors, apply timely security updates, and reassess risks whenever vendors make significant platform changes. Tools like centralized logging with tamper-proof storage and automated anomaly detection (e.g., spotting unusual access patterns from a specific vendor) are vital for identifying and addressing potential issues early.
Platforms such as Censinet RiskOps™ simplify third-party risk management by automating workflows, enabling ongoing monitoring, and fostering collaboration. By creating a cloud-based risk exchange, these platforms allow organizations and vendors to securely share cybersecurity and risk data. This moves beyond static questionnaires to a proactive approach that adapts to changing systems and threats. Together, these principles lay the groundwork for implementing technical controls in areas like authentication, authorization, and session security.
Authentication, Authorization, and Session Security
When it comes to protecting clinical data, authentication, authorization, and session security play a vital role. These technical controls, grounded in the principles of Zero Trust and defense in depth, ensure that identities are verified, permissions are managed effectively, and sessions are safeguarded. Let’s explore how these measures translate into actionable strategies.
Standards-Based Authentication
For healthcare integrations, sticking to established standards like OAuth 2.0, OpenID Connect (OIDC), and SMART on FHIR is essential. Each of these frameworks brings something to the table:
- OAuth 2.0 lays down the foundation for secure authorization.
- OIDC builds on this by adding a layer of identity verification.
- SMART on FHIR extends both, tailoring them specifically for clinical data.
This trio allows third-party applications - like patient portals or tools for clinicians - to request access tokens with clearly defined scopes. For instance, a token might be scoped to patient/Observation.read, granting access to view lab results for a specific patient.
Tokens issued through SMART on FHIR are tightly scoped, restricted by both patient and resource type, which significantly limits exposure. Multi-factor authentication (MFA) is a must for all workforce users accessing protected health information (PHI). By integrating with a centralized identity provider, organizations can streamline enforcement of policies and maintain comprehensive audit logs across all clinical systems.
Fine-Grained Authorization
Once authentication is in place, authorization ensures that access is limited to what’s necessary. A combination of role-based access control (RBAC) and attribute-based access control (ABAC) provides a layered approach:
- RBAC assigns permissions based on predefined roles, such as clinician, billing specialist, or administrator.
- ABAC refines these permissions further by factoring in real-time attributes like patient relationship, location, time of access, device security, or intended use.
For example, a billing application might have a role that allows access to procedure codes and insurance details. However, ABAC rules could restrict this access to only those patients the billing specialist is actively handling during business hours. This layered strategy ensures that even if credentials are compromised, the attacker’s access is severely limited. To enhance security further, organizations should design scopes that align with clinical workflows and avoid granting overly broad permissions like "all data."
Session and Token Security
Securing sessions and tokens is critical to preventing unauthorized access. Here’s how organizations can achieve this:
- Use short-lived access tokens (valid for only a few minutes) and securely bind refresh tokens to specific clients and devices.
- Revoke tokens immediately upon logout or any sign of compromise.
- Implement JWTs (JSON Web Tokens) with built-in safeguards like integrity checks, audience restrictions, expiration times, and instant revocation when necessary.
To counter token replay attacks, ensure endpoints enforce TLS 1.2 or higher and reject all non-HTTPS traffic. Logging token usage is another crucial step - track details like IP addresses, device identifiers, application IDs, and accessed resources. Anomalies, such as geographically impossible logins or unusually high access volumes, should trigger alerts for further investigation.
Session management should also be robust. Tie sessions to both the user and their device, enforce idle and absolute timeouts that align with clinical workflows, and provide users with straightforward options to terminate sessions remotely across devices. This is especially important given that 59% of healthcare organizations report incidents stemming from third-party access [8].
Encryption, Data Integrity, and Privacy
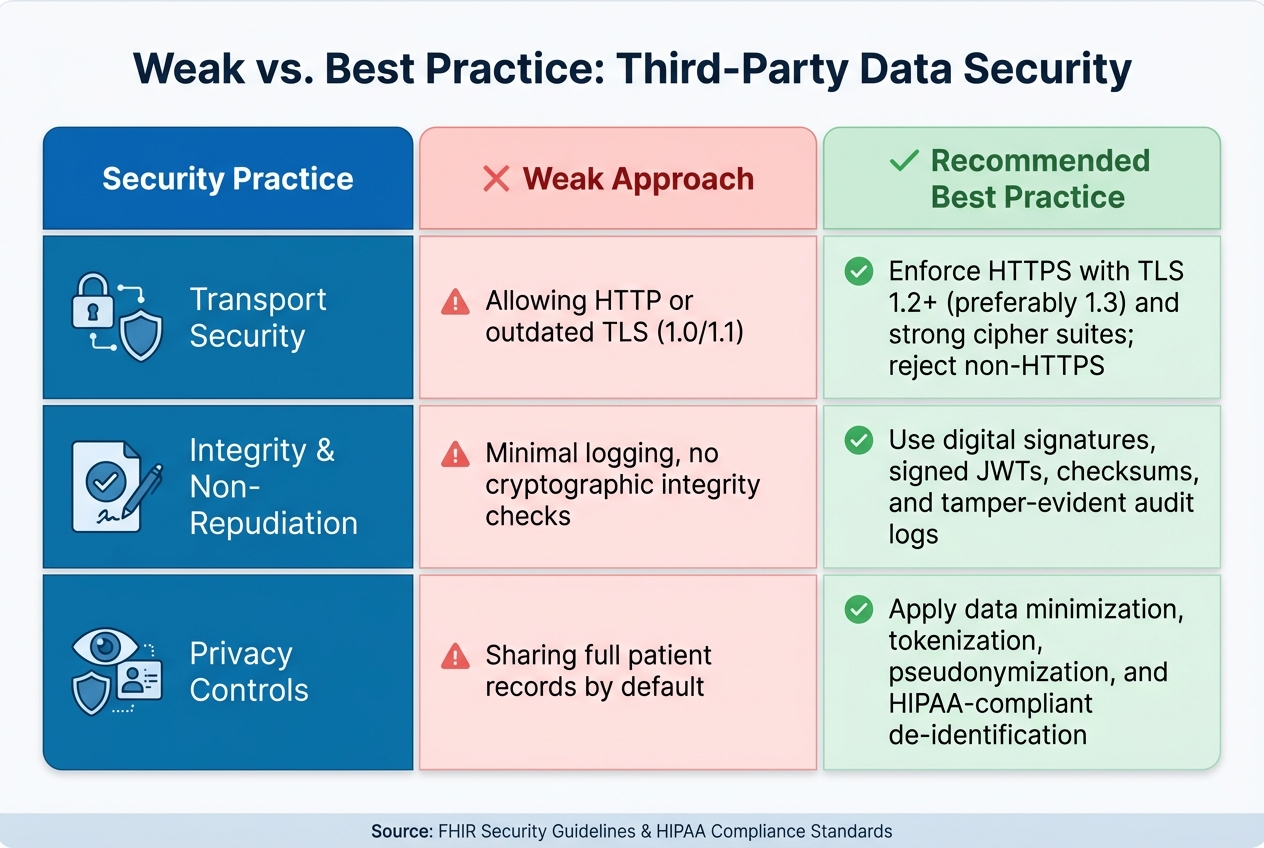
Healthcare Third-Party Data Security: Weak vs. Best Practice Approaches
Securing clinical data goes beyond authentication and session controls. It requires a multi-layered approach that includes encryption, integrity measures, and privacy-focused design principles.
Transport Encryption
To protect data during transmission, enforce HTTPS with TLS 1.2 or higher - ideally TLS 1.3 - across all clinical APIs as recommended by FHIR security guidelines. Reject non-HTTPS requests outright and disable outdated protocols like SSL, TLS 1.0, and TLS 1.1, along with weak ciphers such as RC4 and 3DES. Instead, opt for AES-GCM cipher suites with forward secrecy, such as ECDHE_RSA with AES_128_GCM [3][4].
Manage certificates through trusted authorities using 2048-bit RSA keys or equivalent elliptic curve cryptography. Automate certificate renewals to prevent service interruptions. To enhance security, implement OCSP stapling for real-time certificate validity checks and use certificate pinning for mobile and desktop applications. Additionally, web endpoints should enforce HTTP Strict Transport Security (HSTS), secure cookies, and disable insecure renegotiation [3].
Data Integrity and Non-Repudiation
Transport encryption alone isn’t enough - application-level integrity checks ensure data remains accurate and unaltered. Use methods like HMACs, digital signatures, and SHA-256 checksums to verify data integrity. For critical payloads such as lab orders or diagnostic results, adopt message-level integrity using JSON Web Signatures for FHIR APIs [3]. For larger files, like imaging studies, include SHA-256 checksums and verify them upon receipt.
This approach creates a secure chain of trust. For example, when a hospital sends lab orders to a third-party lab system, the hospital signs each order with its private key. The lab then verifies the signature before processing and signs the results upon return, ensuring the data’s integrity throughout the workflow [3].
Non-repudiation adds another layer of accountability by tying actions to verified identities. Apply digital signatures to high-risk activities like e-prescribing, consent capture, and data exports. Record details such as signer identity, timestamps, and context for each action. These records, combined with tamper-evident audit logs, provide clarity in disputes - for example, identifying who modified a medication list and when - supporting both patient safety and legal compliance [3].
Privacy-by-Design Techniques
Beyond encryption and integrity, privacy-by-design minimizes exposure of Protected Health Information (PHI) at every step. Use scoped APIs to return only the data necessary for each integration [3]. Exclude unnecessary identifiers, clinical notes, or images from payloads. For particularly sensitive data, like behavioral health records, implement separate endpoints with additional security measures.
Tokenization replaces real patient identifiers with surrogate values, ensuring third parties never access actual identifiers. Tokens can be mapped back only under strict controls, and format-preserving tokens can be used for downstream validation without revealing the original data [3].
Pseudonymization further separates identity data from clinical attributes while allowing re-linking under controlled conditions. Store re-identification keys in a secure environment with stringent access controls, and document all re-identification procedures. This method is ideal for analytics or quality improvement initiatives where tracking individual patients over time is necessary without exposing their identities [5][6].
For external data sharing, HIPAA-compliant de-identification offers two approaches:
- Safe Harbor: Removes all 18 HIPAA-defined identifiers, such as names, geographic details beyond the state level, and full-face photos. This method works well for aggregated datasets used in benchmarking [5].
- Expert Determination: Retains more granular data, like three-digit ZIP codes or limited date ranges, when a qualified expert certifies a minimal re-identification risk. This is useful for cases where geographic or temporal precision is essential [5].
When designing APIs for external integrations, include consent-aware endpoints to verify patient consent before releasing PHI. Record consent metadata in audit logs. For non-clinical workflows like billing or capacity planning, prioritize using de-identified or tokenized data feeds instead of live PHI [3]. Tools like Censinet RiskOps™ can simplify these processes by continuously monitoring vendor encryption practices, data handling, and privacy compliance across third-party ecosystems.
| Practice | Weak Approach | Recommended Best Practice |
|---|---|---|
| Transport Security | Allowing HTTP or outdated TLS (1.0/1.1) | Enforce HTTPS with TLS 1.2+ (preferably 1.3) and strong cipher suites; reject non-HTTPS [3][4][7] |
| Integrity & Non-Repudiation | Minimal logging, no cryptographic integrity checks | Use digital signatures, signed JWTs, checksums, and tamper-evident audit logs [3][4][6] |
| Privacy Controls | Sharing full patient records by default | Apply data minimization, tokenization, pseudonymization, and HIPAA-compliant de-identification [3][5][6] |
sbb-itb-535baee
Vendor Governance and Third-Party Risk Management
Technical safeguards are crucial, but they're only as strong as the vendors you work with. That's where structured vendor governance steps in, ensuring third parties meet the same high standards you set internally. Without proper vetting and oversight, even the most secure systems can be compromised. A solid governance program ensures vendors meet security requirements before they access PHI and throughout the entire relationship.
Pre-Contract Due Diligence
Before signing any agreements, dive deep into the vendor's security practices. Review their recent SOC 2 Type II reports, penetration tests, and vulnerability assessments to confirm they maintain robust security controls, especially for PHI. Pay close attention to the scope of these reports, the testing period, any exceptions noted, and how management has addressed findings. System diagrams can also provide valuable insights into how PHI is protected from end to end.
Don't just take their word for it - verify HIPAA compliance with concrete evidence. Look for documentation that demonstrates adherence to both federal and state-specific privacy laws. Some states enforce stricter rules around breach notifications and data destruction, so ensure the vendor is up to speed. Check their policies on PHI handling, access control, and breach response. You’ll also want to evaluate their incident response and disaster recovery plans, including RTO/RPO targets, backup strategies, and communication protocols for situations that could impact patient care.
Business Associate Agreements (BAAs) and Contracts
Contracts go beyond formalities - they set the foundation for accountability. BAAs and other agreements should clearly outline data use restrictions, breach notification procedures, audit rights, and requirements for data return or secure destruction in line with U.S. retention standards. These agreements ensure everyone knows their responsibilities and provide a framework for ongoing oversight.
Ongoing Vendor Monitoring
Once you've completed due diligence and locked in contracts, the work doesn’t stop there. Continuous monitoring is essential to ensure vendors maintain compliance over time. Risks evolve, and vendors’ security postures can change. Use metrics like risk tier distribution, open critical issues, and remediation performance against SLAs to track their ongoing performance. Keep an eye on reported incidents, emerging vulnerabilities, certification updates, or corporate changes that could alter their risk profile.
Tools like Censinet RiskOps™ can simplify this process. By consolidating vendor inventories, integrations, and PHI data flows into one platform, these tools automate risk questionnaires, score vendor risks, and benchmark them against industry standards.
Terry Grogan, CISO at Tower Health, noted: "Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required." [1]
James Case, VP & CISO at Baptist Health, shared: "Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with." [1]
Don’t rely solely on documentation - validate technical controls periodically. Conduct targeted tests to confirm encryption, logging, and access controls. Review data flows and assess API security to ensure everything aligns with your expectations. This hands-on approach keeps your vendor relationships secure over the long haul.
Monitoring, Detection, and Incident Response
Even the most robust controls need constant monitoring to stay effective. Alongside continuous risk management, active monitoring and rapid response are critical for maintaining data security, especially in complex third-party integrations. Without these measures, threats can slip by unnoticed. When external vendors are part of the equation, visibility becomes even more crucial. You're not just keeping an eye on your own systems but also on the access points and data flows that involve external partners.
Centralized Logging and Observability
Effective vendor oversight starts with proactive monitoring of all integration points. This means centralizing logs from every system that handles PHI, such as EHRs, clinical applications, API gateways, identity providers, and vendor systems, into a single SIEM platform. Track API requests and responses (including scopes, resource types, and volumes), authentication and authorization events (OAuth/OIDC, MFA, role changes), administrative or configuration changes, and failed integration attempts. [3][4][9]
For those using FHIR APIs, the AuditEvent resource is a valuable tool. It standardizes logging for read, write, and search operations on PHI, providing a clear framework for security logging in API-driven clinical data exchanges. This resource helps trace who accessed what, when, and how. To stay ahead of potential issues, create dashboards that highlight error rates, spikes in authentication failures, unusual activity during off-hours, and geographic anomalies. These insights can help you identify problems before they escalate. [2][9][10]
Anomaly Detection and Alerts
Establishing a baseline for normal behavior is key to detecting anomalies. Use historical data from at least 30 to 90 days to define typical patterns for clinicians, staff, applications, and vendor integrations. This includes usual hours, locations, data volumes, patient panels, and API endpoints. Then, deploy UEBA or rule-based analytics to flag deviations from these patterns. Examples include sudden spikes in record access, bulk data exports, access from unexpected locations or devices, unusual API usage by a specific client, or calls to undocumented API endpoints. [2][9][10]
Fine-tune your alerts to minimize false positives and focus on high-risk events. For instance, prioritize alerts for access outside normal U.S. business hours by a vendor that typically operates during standard hours, or for misconfigurations that expose PHI, such as an unsecured cloud storage bucket or FHIR API. Automated alerts help your team concentrate on genuine threats rather than wasting time on noise. [3][9][10]
Collaborative Incident Response
Once monitoring and alerting are in place, a coordinated incident response plan becomes essential. Incidents involving third parties demand teamwork. Include detailed incident response and log-sharing requirements in your BAAs and contracts. These should specify maximum notification times after a security incident is detected and outline obligations for preserving and sharing relevant logs. Develop joint incident response playbooks for scenarios like compromised vendor credentials or misconfigured third-party APIs leading to data breaches.
Regular tabletop exercises with vendors are invaluable for testing and refining your response plans. Tools like Censinet RiskOps™ can support this collaborative approach by connecting healthcare organizations with their vendors in a shared risk network. This enables secure sharing of cybersecurity and risk data, strengthening overall preparedness and resilience.
Matt Christensen, Sr. Director GRC at Intermountain Health, highlighted: "Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare." [1]
Clear roles and frequent drills ensure faster containment of threats and safeguard patient care.
Conclusion
Protecting third-party data exchange in clinical settings is critical to ensuring patient safety and maintaining the quality of care. A breach in integrations or APIs can lead to delayed workflows, corrupted data, or exposed Protected Health Information (PHI) - all of which can directly impact diagnoses, treatments, and the continuity of care. By prioritizing secure and reliable third-party integrations, healthcare organizations empower clinicians with accurate, timely patient data while reducing the risk of cyber threats that could disrupt care delivery.
To achieve this, healthcare organizations need a strong, multi-layered security strategy. Implementing practices like zero trust principles, standards-based authentication, strong encryption, and strict vendor oversight creates a solid defense. However, there’s still work to be done - only 51% of healthcare organizations consistently encrypt public network transmissions and enforce least-privileged access, leaving nearly half vulnerable to potential threats [8]. By adopting these measures, organizations can significantly strengthen the security of clinical data exchanges. A unified monitoring strategy further enhances protection by enabling rapid threat detection and response.
Additionally, robust Business Associate Agreements (BAAs), thorough pre-contract evaluations, and continuous vendor monitoring are essential to ensure that external partners meet the same security standards as internal systems. Tools like Censinet RiskOps™ play a pivotal role in this process, offering healthcare organizations a way to move beyond static questionnaires toward proactive, ongoing risk management. This platform facilitates continuous monitoring and secure sharing of risk data, addressing the dynamic nature of cybersecurity challenges.
As highlighted earlier, healthcare leaders must embrace continuous risk management practices. This includes defining baseline behaviors, deploying anomaly detection systems, and conducting regular joint incident response drills to identify and address vulnerabilities. Benchmarking cybersecurity programs against industry standards is a key step in identifying gaps and securing the necessary resources to address them.
Brian Sterud, CIO at Faith Regional Health, emphasized the importance of this approach: "Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters."
FAQs
Why are Zero Trust and Least Privilege important for securing third-party data exchanges?
Zero Trust and Least Privilege are essential strategies for securing third-party data exchanges, particularly in environments where sensitive information is at stake. Zero Trust is built on the principle of never assuming trust, even for users or devices already inside the network. Instead, it requires continuous verification of identities and devices to ensure security at every access point.
Meanwhile, Least Privilege ensures that users only have access to the specific data and permissions required for their role - nothing more. This approach minimizes the risk of data breaches or misuse by limiting the scope of access.
When combined, these principles form a powerful defense for protecting sensitive healthcare data, such as patient records and clinical application integrations. They work together to enforce strict access controls, reducing vulnerabilities and keeping critical information secure.
What are the best ways for healthcare organizations to continuously monitor and manage third-party risks?
Healthcare organizations can tackle third-party risks more efficiently by leveraging advanced tools like Censinet RiskOps™. These AI-powered platforms simplify risk management through real-time assessments, automated notifications, and cybersecurity benchmarking, eliminating the outdated reliance on spreadsheets.
With continuous risk monitoring and dynamic threat assessments, these tools enable organizations to address vulnerabilities proactively, stay compliant with healthcare regulations, and protect sensitive data like patient information and PHI. This method not only strengthens security but also ensures smoother operations in an ever-evolving healthcare landscape.
How does encryption protect healthcare data during third-party integrations?
Encryption is essential for protecting healthcare data, especially during third-party integrations. It ensures privacy and data integrity by converting sensitive information into unreadable code. This makes it nearly impossible for unauthorized users to access, keeping patient data secure and aligning with regulations like HIPAA in the United States.
Beyond privacy, encryption also safeguards data from unauthorized changes during transmission. This ensures the information remains accurate and reliable. By using strong encryption methods, healthcare organizations can safely exchange data while reducing risks to patient confidentiality and overall operational security.
Related Blog Posts
Key Points:
What is third-party data exchange security?
- Definition: Third-party data exchange security involves implementing strategies and practices to protect sensitive data shared between organizations and their third-party vendors.
- Purpose: It ensures that data remains secure during transfer, storage, and usage by external entities.
Why is securing third-party data exchanges critical?
- Data Breaches: Third-party vendors are often the weakest link in an organization’s security, making them prime targets for cyberattacks.
- Compliance: Regulations like HIPAA, GDPR, and SOC 2 require organizations to secure data shared with third parties.
- Reputation and Trust: A breach involving third-party data can damage an organization’s reputation and erode customer trust.
What are the key risks of third-party data exchanges?
- Data Breaches: Vendors with weak security practices can expose sensitive data to unauthorized access.
- Lack of Encryption: Data not encrypted during transfer or storage is vulnerable to interception.
- Insufficient Monitoring: Without real-time monitoring, organizations may miss vulnerabilities or breaches in vendor systems.
- Poor Vendor Practices: Vendors may lack robust security frameworks or fail to notify organizations of incidents.
What are the best practices for securing third-party data exchanges?
- Vendor Risk Assessments: Evaluate vendors’ security practices, compliance certifications, and incident response plans before onboarding.
- Data Encryption: Use protocols like HTTPS, SFTP, and IPSec to secure data during transfer.
- Continuous Monitoring: Implement tools to track vendor security posture in real time and flag vulnerabilities.
- Strong Contracts: Include security expectations, breach notification requirements, and penalties for non-compliance in vendor agreements.
- Data Anonymization: Remove or mask sensitive information before sharing data with third parties.
What role do compliance frameworks play in third-party data security?
- Standardization: Frameworks like SOC 2, ISO 27001, and HIPAA provide standardized guidelines for securing third-party data exchanges.
- Accountability: Vendors adhering to these frameworks demonstrate their commitment to data security and compliance.
- Risk Mitigation: Compliance frameworks help organizations identify and address potential risks in vendor relationships.
What tools can organizations use to secure third-party data exchanges?
- Censinet RiskOps™: Automates vendor risk assessments, monitors compliance, and provides real-time visibility into vendor security.
- Encryption Tools: Use tools that support SFTP, HTTPS, and other secure protocols to protect data in transit.
- Monitoring Platforms: Implement continuous monitoring solutions to track vendor activities and detect vulnerabilities.
- Data Anonymization Software: Tools that mask or pseudonymize sensitive data before sharing with third parties.


