Clinical Continuity Planning: Ensuring Patient Care During Vendor Disruptions
Post Summary
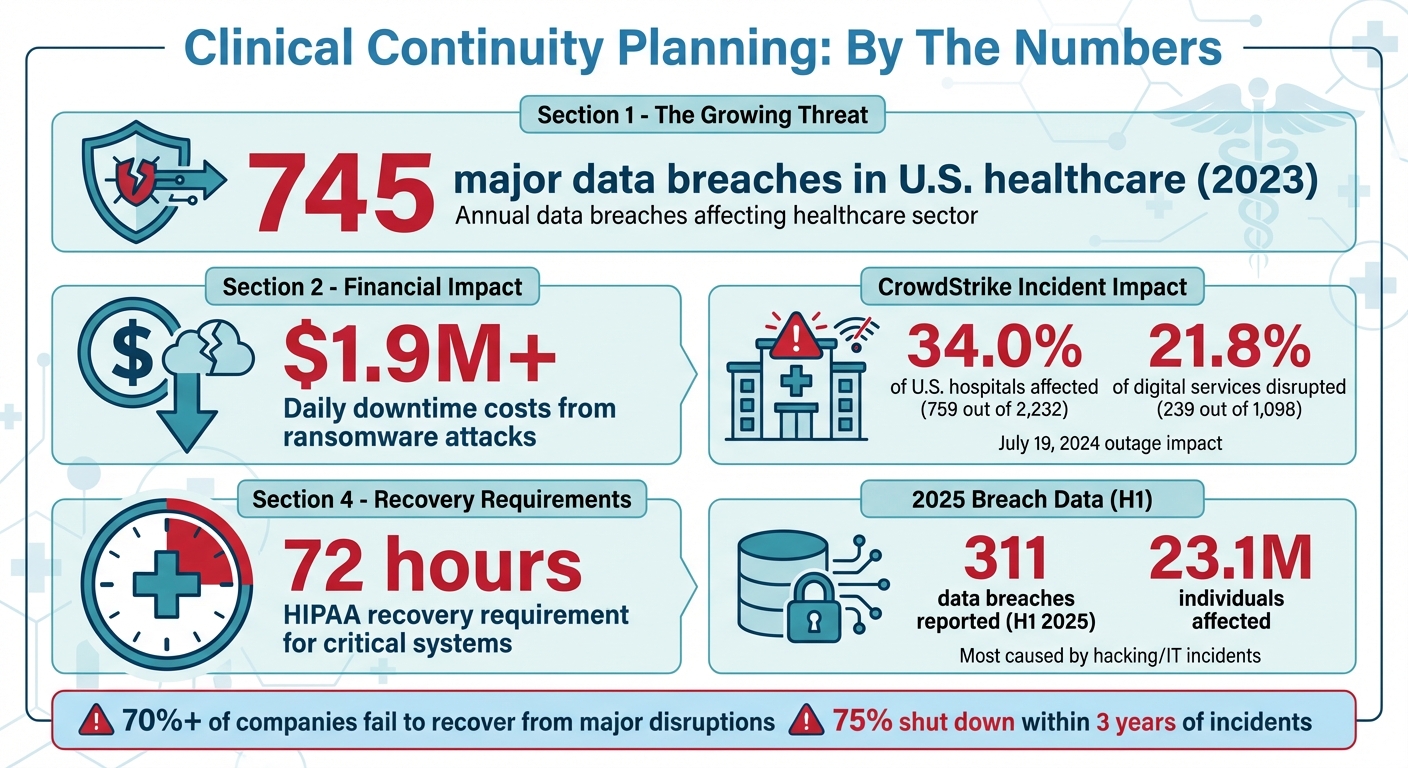
Healthcare providers depend on third-party systems like electronic health records (EHRs) and scheduling tools to deliver care. But when these systems fail - due to cyberattacks, outages, or technical issues - patient safety, clinical workflows, and operations are at risk. To counter this, clinical continuity planning is critical. It helps maintain patient care during disruptions by identifying key risks, setting up backup procedures, and ensuring quick recovery.
Key Points:
Why It Matters: Without preparation, vendor disruptions can delay treatments, violate regulations like HIPAA, and harm both patient trust and organizational stability. A strong continuity plan isn’t optional - it’s a necessity.
Healthcare Vendor Disruption Statistics and Impact Data 2023-2025
Identifying and Assessing Vendor Risks
To safeguard patient care from potential vendor disruptions, the first step is identifying your system's weak points. This requires a detailed evaluation of every vendor connected to your operations, data, or systems. According to BARR Advisory, vendor risk management often lacks sufficient processes to ensure data security [4]. Using structured frameworks and practical tools can help address these vulnerabilities effectively. Below are actionable steps to assess and minimize these risks.
How to Conduct Vendor Risk Assessments
Choosing the right assessment framework is key. For healthcare organizations, standards like HITRUST, along with broader frameworks such as NIST SP 800-53, PCI, SOC 1, and SOC 2, offer reliable methods to evaluate vendor security and compliance [4]. These frameworks allow you to systematically review vendor practices, including their data protection measures, operational stability, and security controls.
Vendor questionnaires are an essential tool for gathering insights into areas like internal controls, cybersecurity protocols, compliance status, financial stability, data encryption methods, incident response strategies, and business continuity plans [7]. For vendors deemed critical or high-risk - such as those managing electronic health records, medical devices, or patient scheduling systems - on-site audits provide deeper insights. These audits can uncover weaknesses in disaster recovery plans and other areas that may not be fully evident in written documentation [7].
The HHS Assistant Secretary for Technology Policy offers a Security Risk Assessment Tool that healthcare providers can adapt for evaluating vendors [5]. While NIST standards aren't mandatory for HIPAA compliance, they serve as a robust foundation for spotting vulnerabilities. Keep in mind that vendor risks are not static - they evolve as new threats arise and systems change. Continuous monitoring is therefore vital to stay ahead of potential risks and maintain compliance [4].
Ranking Risks by Impact on Patient Care
After completing assessments, it’s crucial to rank vendors based on their impact on clinical operations. Not all vendors carry the same level of risk to patient care. For example, a vendor managing your emergency department's electronic health records system poses a much higher risk than one handling non-urgent administrative scheduling. This categorization helps focus attention and resources where disruptions would most directly affect patient safety and treatment.
Align your vendor risk management strategy with broader organizational goals, such as patient safety, quality assurance, regulatory compliance, and enterprise risk management [6]. Pay particular attention to vendors involved in IT risk management, third-party risks, compliance, and AI governance [6]. For each vendor, consider the potential consequences of system downtime - whether it lasts an hour, a day, or a week. Assess which clinical functions would be disrupted, how patients would be affected, and how quickly backup systems could take over. These evaluations guide investments in redundancy, alternative workflows, and better monitoring systems. A thorough risk assessment ensures that your continuity plans are tailored to address the most critical threats to patient care.
Building a Clinical Continuity Plan
After identifying and prioritizing vendor risks, the next critical step is crafting a clinical continuity plan. This plan ensures that your organization can maintain essential operations and patient care, even during disruptions. Essentially, it’s a roadmap to minimize downtime, protect your reputation, and - most importantly - keep patients and staff safe during crises [8][1].
Start by using your risk assessments to pinpoint the clinical services that must stay operational no matter what. Conduct a Business Impact Analysis (BIA) to gauge potential financial losses, patient satisfaction issues, legal risks, and damage to your organization’s reputation. From there, establish recovery time objectives (RTOs) - the maximum acceptable time a system or service can be offline without causing severe harm [8][1][9].
An effective continuity plan combines both proactive measures to maintain operations and reactive strategies to recover after disruptions. Business continuity ensures essential functions keep running, while disaster recovery focuses on restoring IT systems and data. Together, they create a safety net for uninterrupted patient care. Industry standards like ISO 22301:2019 and frameworks such as NIST SP 800-34 provide helpful guidelines for structuring your plan [8].
What to Include in Your Continuity Plan
For a continuity plan to work effectively, it needs to cover several key areas:
Using Technology to Support Continuity Planning
Technology can simplify and strengthen your continuity planning efforts, especially as vendor networks grow and risks evolve. Managing these complexities manually can quickly become overwhelming, but technology platforms can centralize information, automate workflows, and improve the speed and accuracy of responses.
Censinet RiskOps™ is one such platform designed to centralize vendor risk assessments, BIAs, and incident response plans [8]. Its automated workflows help track recovery time objectives, monitor compliance with continuity requirements, and assign tasks to the right team members. Think of it as a control tower, ensuring critical issues are routed to the appropriate stakeholders without delay.
The platform also provides a real-time command center, offering visibility into vendor risks and continuity statuses. Risk teams can quickly identify which vendors support key clinical functions, assess the potential impact of disruptions, and prioritize recovery efforts based on patient care needs. Additionally, Censinet AITM™ enhances planning by automatically summarizing vendor documentation, capturing integration details, and identifying fourth-party risks that could affect your strategies.
When disruptions occur, having instant access to continuity information can make all the difference. Censinet RiskOps™ keeps vendor contact details, escalation procedures, and recovery plans readily available, enabling response teams to act quickly. Its collaborative tools allow real-time coordination between internal teams, vendors, and external partners, reducing response times and ensuring the plan is executed effectively - when every second matters.
Responding to and Recovering from Vendor Incidents
When vendor disruptions strike, having a solid continuity plan is just the beginning. A quick and well-coordinated response is what truly determines whether patient care proceeds smoothly or grinds to a halt. Take the CrowdStrike outage on July 19, 2024, as an example. This incident, caused by a faulty software update, disrupted Windows systems globally. In the U.S. healthcare sector alone, 759 out of 2,232 hospitals (34.0%) faced service interruptions. Of the 1,098 digital services affected, 239 (21.8%) were patient-facing systems, including critical tools like EHR access, imaging platforms, and fetal monitoring systems. While most services were restored within hours, some took over 48 hours to recover [10].
Acting immediately is non-negotiable. As soon as systems fail, activate downtime procedures and assess which patient care systems are impacted. Recovery efforts should align with your pre-established recovery time objectives (RTOs), while keeping HIPAA’s 72-hour recovery requirement for critical health systems in mind [10][12]. Your response plan should focus on identifying the root cause, preventing further risks, and restoring operations as quickly as possible [15]. This highlights the importance of having strong, well-defined incident response protocols in place.
Creating Incident Response Protocols
Strong incident response protocols hinge on clear documentation and tested procedures for detecting, reporting, and resolving issues. One key element is defining shutdown criteria to trigger manual workflows in case systems are compromised. For vendor-specific incidents, your notification strategy must comply with business associate agreements, which typically require vendors to notify you within 24 hours of activating contingency measures [12].
When designing these protocols, use frameworks like the HIPAA Security Rule and NIST Cybersecurity Framework as guides. Resources such as the HHS Cyber Security Checklist and Ransomware Guidance offer practical steps to structure your response [16]. To enhance your readiness, integrate incident response capabilities into your communication tools. These should support secure breach notifications, system lockdowns, audit logging, and backup channels [12]. With third-party involvement in data breaches nearly doubling, it’s crucial to set clear expectations for vendor incident responses and establish dedicated workflows for supply chain disruptions [13].
Working with External Partners During Incidents
Recovery is rarely a solo effort. Transparent, two-way communication between healthcare providers, manufacturers, and distributors is essential for documenting, monitoring, and forecasting product needs during disruptions. Aligning external communication with your continuity procedures strengthens your overall resilience.
"It is critical to forge new relationships with onshore and near-shore suppliers or invest in dependable companies that can fill their needs during peak surges."
This advice from the American Hospital Association underscores the importance of diversifying your supply chain and leveraging community resources, such as healthcare coalitions and regional partners, to support recovery efforts [14].
When working with affected vendors, rely on data-driven approaches to avoid overreacting to supply chain disruptions [11]. If necessary, collaborate with external cybersecurity experts to bolster your incident response capabilities [15]. During the recovery phase, document lessons learned and refine your protocols based on how they performed in practice. In the first half of 2025, U.S. healthcare organizations reported 311 data breaches affecting approximately 23.1 million individuals, with most caused by hacking and IT-related incidents. This underscores the ongoing need to improve incident response strategies [12]. By combining internal efforts with external partnerships, you can create a cohesive and effective recovery plan.
sbb-itb-535baee
Testing and Updating Your Continuity Plans
A continuity plan is only as good as its testing. Without regular evaluation, it’s just a document gathering dust. Consider this: more than 70% of companies fail to recover from major disruptions, and 75% shut down within three years of such incidents [19]. These numbers underscore why testing your continuity plan is absolutely critical.
To start, schedule quarterly tabletop exercises. These discussion-based reviews help you examine potential scenarios and identify weak spots in your plan [18][19]. However, keep in mind that while these exercises are useful, they often lack the depth to uncover all vulnerabilities, especially if the focus is limited to IT systems.
For a more thorough evaluation, conduct annual full-scale simulations. These stress tests go beyond discussions, putting your production processes, networks, personnel, and facilities to the test [18]. Make sure your disaster recovery systems are designed to handle 100% capacity, not just partial loads, since real-world demands often exceed expectations [18].
Running Vendor Disruption Drills
Vendor disruptions can have ripple effects on your operations, so it’s essential to test how your organization handles these situations. Run drills that simulate downtime, vendor communication breakdowns, and their impact on critical services like patient care. Align these exercises with your overall business continuity goals, starting with a gap analysis to define the drill's purpose [19].
Don’t stop at testing a single failure point. For example, simulate a scenario where your EHR system goes down while access to imaging platforms or laboratory systems is also interrupted. This multi-layered approach ensures your team is prepared for complex challenges. Verify that all communication channels, including backup tools for breach notifications and system lockdowns, are functioning before starting the drill [19].
Budgeting is another key element. Allocate sufficient resources, define the roles of participants, and provide any necessary training to ensure the drill runs smoothly [19]. Afterward, document everything in post-exercise reports. These reports should include outcomes, recommendations, and specific action points for improvement [19][2]. Regularly engaging your recovery team in these simulations helps identify gaps and improve your overall readiness [20]. Use the results to update your continuity plan and strengthen weak areas.
Learning from Incidents to Improve Plans
Every disruption is an opportunity to refine your continuity plan. Review and update your plan annually - or sooner if significant operational, technological, or facility changes occur, or after learning key lessons from an incident [2][17][19]. This ongoing process ensures your plan stays effective and ready for future challenges [3].
When analyzing incidents, focus on four critical areas: people, processes, premises, and providers [3]. Use these insights to revise training programs, improve communication strategies, and update your Business Impact Analysis [3]. Evaluate vendor performance during disruptions, and if necessary, diversify your supplier base or renegotiate contracts with critical vendors [3].
Take concrete steps to address vulnerabilities. Update supporting documentation, including contact lists, critical functions, supplies, vendors, equipment, and alternate site details. Regular practice runs are essential - they reveal weaknesses and give you the chance to make quick adjustments, ultimately strengthening your organization’s resilience [20].
The feedback from these tests plays a vital role in refining your strategies. By continuously evolving your continuity plans to address emerging risks and challenges, you’ll be better prepared for whatever comes next [20].
Conclusion
Vendor disruptions are bound to happen, but with proper preparation, healthcare organizations can avoid severe consequences that jeopardize patient care. The difference between a minor inconvenience and a full-blown crisis often comes down to how well-prepared an organization is. By focusing on detailed risk assessments, strong continuity plans, and consistent testing, healthcare providers can ensure critical operations remain intact during disruptions. These efforts build on existing strategies, creating a seamless safety net for patient care.
Prolonged downtime puts both revenue and patient safety at risk, making swift recovery a top priority. In healthcare, the stakes are exceptionally high since disruptions impact not only business operations but also the ability to provide safe and timely care. This is why continuity planning should be seen as a continuous commitment, not a one-and-done task.
Leveraging technology like Censinet RiskOps™ can simplify vendor risk assessments and automate key workflows, ensuring uninterrupted oversight of essential operations. These tools, combined with proactive planning, help shield your organization from vendor-related challenges.
Key Takeaways
FAQs
What are the essential steps for healthcare providers to assess vendor risks effectively?
To carry out a thorough vendor risk assessment, begin by sorting your vendors into categories based on the level of risk they pose. Carefully examine their security and compliance documentation to confirm they align with your required standards. From there, create action plans to manage any risks you uncover, and set up continuous monitoring to catch potential problems early. Additionally, make sure you have a well-defined incident response plan in place and establish clear steps for vendor offboarding when the relationship ends.
How can healthcare organizations maintain clear communication during vendor disruptions?
Healthcare organizations can navigate vendor disruptions more effectively by adopting a few practical strategies. Conducting regular performance reviews helps pinpoint potential problems before they escalate. Leveraging digital communication tools promotes open and transparent dialogue, ensuring all parties stay on the same page. To address changes swiftly, real-time alerts can be used to notify vendors immediately about disruptions. Moreover, incorporating vendors into incident response plans creates a unified and streamlined approach to tackling challenges as they arise.
How does technology help maintain patient care during disruptions?
Technology is essential for keeping patient care on track during unexpected disruptions like cyberattacks or system outages. It ensures rapid response mechanisms, reliable data backup and recovery, and smooth communication across healthcare teams.
Some of the most important tools include well-structured incident response plans, tiered recovery systems to prioritize critical applications, and strong digital security protocols. These solutions work together to safeguard patient information, keep operations running, and support clinical workflows even in tough situations.
Related Blog Posts
- Top 7 Cloud Disaster Recovery Tools for Healthcare
- Clinical Continuity Planning: Ensuring Patient Care During Vendor Disruptions
- Patient Care Can't Wait for Cloud Recovery: Healthcare's Business Continuity Crisis Exposed
- The AWS Outage Exposed Cloud Vulnerabilities - What It Means for Healthcare Business Continuity
{"@context":"https://schema.org","@type":"FAQPage","mainEntity":[{"@type":"Question","name":"What are the essential steps for healthcare providers to assess vendor risks effectively?","acceptedAnswer":{"@type":"Answer","text":"<p>To carry out a thorough <a href=\"https://censinet.com/vendor-solutions\">vendor risk assessment</a>, begin by sorting your vendors into categories based on the level of risk they pose. Carefully examine their <strong>security and compliance documentation</strong> to confirm they align with your required standards. From there, create action plans to manage any risks you uncover, and set up <strong>continuous monitoring</strong> to catch potential problems early. Additionally, make sure you have a well-defined <strong>incident response plan</strong> in place and establish clear steps for vendor offboarding when the relationship ends.</p>"}},{"@type":"Question","name":"How can healthcare organizations maintain clear communication during vendor disruptions?","acceptedAnswer":{"@type":"Answer","text":"<p>Healthcare organizations can navigate vendor disruptions more effectively by adopting a few practical strategies. Conducting <strong>regular performance reviews</strong> helps pinpoint potential problems before they escalate. Leveraging <strong>digital communication tools</strong> promotes open and transparent dialogue, ensuring all parties stay on the same page. To address changes swiftly, <strong>real-time alerts</strong> can be used to notify vendors immediately about disruptions. Moreover, incorporating vendors into <strong>incident response plans</strong> creates a unified and streamlined approach to tackling challenges as they arise.</p>"}},{"@type":"Question","name":"How does technology help maintain patient care during disruptions?","acceptedAnswer":{"@type":"Answer","text":"<p>Technology is essential for keeping patient care on track during unexpected disruptions like cyberattacks or system outages. It ensures <strong>rapid response mechanisms</strong>, reliable data backup and recovery, and smooth communication across healthcare teams.</p> <p>Some of the most important tools include well-structured <strong>incident response plans</strong>, <strong>tiered recovery systems</strong> to prioritize critical applications, and strong <strong>digital security protocols</strong>. These solutions work together to safeguard patient information, keep operations running, and support clinical workflows even in tough situations.</p>"}}]}


