Cross-Functional TPRM Collaboration in Healthcare: IT, Legal, and Clinical Alignment
Post Summary
Managing third-party risks in healthcare requires IT, legal, and clinical teams to work together. Why? Because vendor risks impact patient safety, data security, and compliance. Yet, silos between these departments often lead to delays, blind spots, and disjointed responses to incidents.
Here’s how healthcare organizations can improve collaboration:
- Shared Goals: Align TPRM (Third-Party Risk Management) objectives with priorities like protecting patient data and ensuring care continuity.
- Defined Roles: IT handles cybersecurity, legal manages contracts and compliance, and clinical teams focus on patient care and workflow integration.
- Integrated Workflows: Standardize processes to involve all teams from the start, avoiding redundant efforts and gaps.
- Technology: Use platforms like Censinet RiskOps™ for real-time risk tracking and communication across departments.
- Continuous Monitoring: Automate risk updates to stay ahead of emerging threats.
The result? Faster vendor assessments, reduced risks, and stronger patient trust. Collaboration isn’t just helpful - it’s essential in today’s healthcare landscape.
Defining Roles: IT, Legal, and Clinical Collaboration in TPRM
Healthcare TPRM: IT, Legal, and Clinical Department Roles and Responsibilities
Key Responsibilities of Each Department
Each department plays a distinct role in third-party risk management (TPRM), and understanding these roles is critical for seamless collaboration.
IT teams focus on identifying and mitigating cybersecurity threats. They conduct in-depth security assessments of vendors, evaluate system vulnerabilities, and continuously monitor for potential breaches to maintain the integrity of the organization's network.
Legal departments handle contracts, compliance, and liability concerns. They review vendor agreements to ensure proper data handling measures are in place, including Business Associate Agreements (BAAs) to meet HIPAA requirements.
Clinical teams prioritize patient care and operational continuity. Their responsibilities include assessing whether vendors can integrate smoothly into clinical workflows, determining the potential impact of vendor-related issues on patient outcomes, and ensuring that devices and systems align with clinical standards.
"While legal and compliance teams are typically the owners of third-party risk management, there are several others within the organization who have a stake in improving risk management and associated business outcomes." - Cherry Bekaert [4]
Clearly defining these roles sets the stage for understanding how these departments depend on one another.
Understanding Interdependencies
Vendor risks don’t exist in isolation - they can affect multiple areas simultaneously. Effective vendor reviews require input from IT, legal, and clinical teams to prevent vulnerabilities, contractual disputes, and disruptions in patient care. A single vendor failure could lead to security breaches, legal complications, and interruptions in clinical services, all at once.
"TPRM can only ever be effective if organizations have access to all available information about third-party suppliers, and the systems and processes they have in place as well as visibility into their extended supply chains and the ability to collaborate quickly across different teams when new vulnerabilities or incidents appear. No IT security team alone can shoulder all of this responsibility. That's why managing third-party risks must be a whole-organization priority." - Risk Ledger [1]
In 2025, Providence demonstrated this collaborative approach by bringing together clinicians, compliance experts, and IT leaders to tackle new artificial intelligence regulatory standards. By fostering clear communication and mapping out roles, they successfully aligned their efforts and met compliance goals on schedule [3]. This example underscores how interdependencies, when managed well, can transform into organizational strengths.
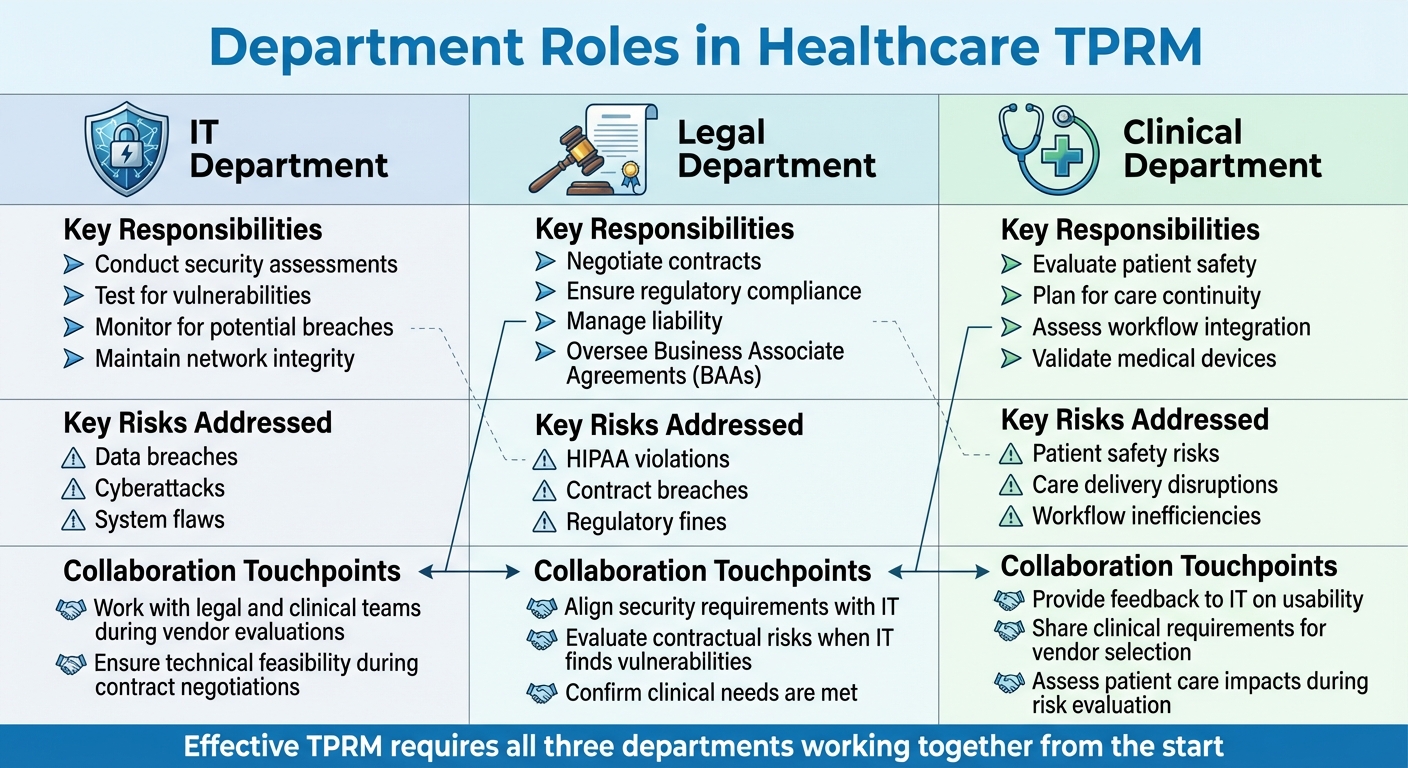
The table below further illustrates how these roles intersect and complement one another during the TPRM process.
Table: Department Roles, Risks, and Collaboration Touchpoints
| Department | Key Responsibilities in TPRM | Key Risks Addressed | Collaboration Touchpoints |
|---|---|---|---|
| IT | Conduct security assessments and test for vulnerabilities | Protect against data breaches, cyberattacks, and system flaws | Collaborate with legal and clinical teams during vendor evaluations |
| Legal | Negotiate contracts, ensure regulatory compliance, manage liability, and oversee BAAs | Address HIPAA violations, contract breaches, and regulatory fines | Align security requirements with IT and clinical needs |
| Clinical | Evaluate patient safety, plan for care continuity, assess workflows, and validate medical devices | Mitigate risks to patient safety, care delivery, and workflow efficiency | Provide feedback to IT on usability and share clinical requirements for vendor selection |
This table highlights how each department’s expertise contributes to the TPRM process. For example, if IT uncovers a vulnerability, legal teams can evaluate related contractual risks, while clinical teams assess potential impacts on patient care. Similarly, during contract negotiations, IT ensures technical feasibility, and clinical teams confirm that workflows remain unaffected. Tools like RACI charts can help clarify these roles and streamline collaboration [5].
Strategies for Breaking Down Silos Between IT, Legal, and Clinical Teams
Establishing Shared Goals and Priorities
Healthcare systems often face challenges caused by departmental silos, which can slow down innovation and delay risk management efforts. A strong starting point is to align IT, legal, and clinical teams around common Third-Party Risk Management (TPRM) goals [6].
By tying TPRM objectives to broader organizational priorities - like safeguarding patient data, enhancing satisfaction, and cutting operational costs - teams can see how their efforts contribute to the bigger picture [1]. Connecting TPRM with patient care shifts compliance from being a checkbox exercise to an actionable mission. Leaders should consistently explain the "why" behind TPRM, ensuring teams understand its importance, not just its requirements [3].
"Because TPRM is central to the success of any organisation, it should be possible to align TPRM objectives with broader company goals, such as protecting data, improving customer satisfaction and reducing costs." - Risk Ledger [1]
Accountability is key to making TPRM a priority. Including cross-functional TPRM objectives in individual performance reviews keeps IT, legal, and clinical teams focused on shared results [1]. Structured communication and clearly defined roles also help identify and address misaligned goals early on [3].
Once shared goals are in place, the next step is to embed them into day-to-day workflows.
Implementing Cross-Functional Workflows
Standardized workflows that involve input from all three departments - IT, legal, and clinical - can eliminate inefficiencies and prevent bottlenecks. Designing workflows that require collaboration from the outset, rather than as an afterthought, helps teams work more effectively.
Take the example of evaluating a new vendor: IT can handle security assessments, legal can review contracts, and clinical staff can assess workflow integration - all at the same time. This parallel approach not only speeds up decisions but also ensures that no critical risks slip through the cracks. Clearly defining handoff points and decision-making responsibilities further reduces confusion about who is accountable for each step.
These streamlined workflows set the stage for technology to play a bigger role in improving collaboration and risk management.
Using Technology for Better Collaboration
With unified goals and integrated workflows in place, technology can strengthen cross-functional TPRM efforts. Tools that provide real-time visibility into vendor risks and assessment progress help bridge gaps between departments. For instance, platforms like Censinet RiskOps™ allow IT, legal, and clinical teams to share data, track tasks, and communicate updates without relying on cumbersome email chains or spreadsheets.
Integrated risk registers can notify legal and clinical teams immediately when IT identifies vulnerabilities, enabling quick assessments of contractual and clinical implications [7]. Mobile access to risk data ensures that team members can stay updated and engaged wherever they are. When everyone operates with the same real-time information, collaboration becomes natural and efficient, rather than forced or fragmented.
Tools and Processes for Effective TPRM Alignment
Risk-Tiering and Vendor Inventory Management
Building a complete vendor inventory is a critical first step in managing third-party risks effectively. It's essential to know which vendors have access to patient data, clinical systems, or critical infrastructure to prioritize risks appropriately. By assigning vendors to categories like critical, high, medium, or low risk - based on factors such as data access, system integration, and regulatory requirements - organizations can focus their efforts where they're needed most. For example, IT teams can zero in on security assessments for high-risk vendors, legal teams can prioritize contract reviews for those handling protected health information (PHI), and clinical teams can concentrate on vendors that directly impact patient care processes. When all departments work from a shared, risk-tiered inventory, collaboration improves because everyone is on the same page about which vendors require immediate attention and which can follow standard review procedures.
Platforms like Censinet RiskOps™ simplify this process by maintaining centralized vendor inventories with real-time risk scores. This shared visibility eliminates the inefficiencies of juggling separate spreadsheets or databases, ensuring IT, legal, and clinical teams can work together seamlessly.
Once a clear, risk-tiered vendor inventory is established, organizations can streamline their assessments through standardized workflows.
Standardized Assessment Workflows
Standardized workflows bring consistency and clarity to vendor assessments by defining clear steps, roles, and responsibilities. This structure prevents duplication of efforts and ensures the process runs more smoothly and efficiently [2]. When team members understand their specific responsibilities and how their work fits into the overall process, assessments are completed faster and with greater accuracy [2].
A typical workflow might involve IT conducting security reviews, legal teams evaluating contract terms and liability, and clinical staff assessing how well a vendor aligns with care delivery needs. These tasks can happen simultaneously, reducing review times. Tools like RACI charts (Responsible, Accountable, Consulted, Informed) help clarify task ownership and decision-making responsibilities, ensuring everyone knows their role in the process [5][3].
Automation and standardization further enhance these workflows, saving time and improving accuracy. Documenting these processes on internal platforms allows new team members to quickly understand their roles without requiring extensive training [3].
While standardized workflows provide consistency, continuous monitoring and automation are essential for staying agile in the face of evolving risks.
Continuous Monitoring and Automation
Keeping up with rapidly changing risks is nearly impossible with manual reviews. Continuous monitoring tools address this challenge by automatically tracking changes in vendor security postures, compliance statuses, and threat intelligence. These tools alert teams as soon as new risks arise, replacing outdated annual assessments with ongoing oversight. This ensures that IT, legal, and clinical teams stay aligned with the current risk landscape rather than relying on stale information.
Automation further reduces the manual workload that often slows collaboration. For instance, Censinet AITM speeds up third-party risk assessments by enabling vendors to quickly complete security questionnaires. It then automatically summarizes evidence, compiles documentation, and generates risk summary reports. This approach allows healthcare organizations to address risks more efficiently while maintaining human oversight through configurable rules and review processes.
Dynamic risk scoring keeps vendor profiles up to date in real time by pulling data from multiple sources. Integrated dashboards with real-time notifications ensure that IT, legal, and clinical teams can respond immediately to emerging risks. This streamlined system not only accelerates assessments but also strengthens collaboration across departments, ensuring no team is left in the dark. The result is faster, more coordinated risk mitigation efforts that adapt to the ever-changing threat landscape.
sbb-itb-535baee
Case Studies and Metrics for Success
Case Studies on IT-Legal-Clinical Collaboration
The University of Kansas Health System (UKHS) offers a compelling example of how technology-driven collaboration can transform third-party risk management (TPRM). By moving away from disconnected spreadsheets and manual workflows, UKHS implemented an automated, enterprise-wide vendor risk management system. This shift not only saved significant time but also allowed staff to focus on higher-priority tasks. Jennifer Blackburn, Cybersecurity Analyst at UKHS, highlighted how centralized dashboards improved visibility into workflows, boosting both efficiency and speed. The result? Stronger collaboration between IT, legal, and clinical departments. Megan Loescher, Senior Cybersecurity Analyst, noted that the platform enabled the governance, risk, and compliance (GRC) team to evolve into a more effective partner for internal teams, removing barriers and fostering stronger relationships.
Similarly, Providence demonstrated the value of structured communication and clearly defined roles, further validating the importance of collaborative approaches [3]. These examples not only showcase successful strategies but also set the stage for tracking measurable improvements in TPRM outcomes.
Key Metrics for Measuring Alignment and Outcomes
To gauge the success of cross-functional TPRM efforts, healthcare organizations should focus on metrics that reflect both operational efficiency and risk reduction. Key performance indicators include assessment completion times, vendor risk scores, and compliance progress. For example, some security teams have cut meeting durations in half by leveraging integrated collaboration tools, while compliance teams have reduced administrative workloads by 40% through better alignment and automation [7]. One hospital compliance team even managed to shrink its annual HIPAA documentation process from six weeks to just three days using automation [7].
Risk-related metrics are equally important. These include tracking the number of Tier 1 suppliers who have not completed self-attestations, monitoring credit ratings and financial scores, and assessing reputational risks through external intelligence sources. Compliance metrics, on the other hand, focus on breach incidents, regulatory findings, and audit readiness scores [8]. With 62% of healthcare organizations identifying themselves as "at risk" - a figure ten percentage points higher than the global average - and over 276 million health records exposed across 734 breaches in 2024 [7], these metrics provide essential insights into whether collaborative efforts are effectively mitigating risks.
By understanding and utilizing these key indicators, organizations can identify what works and scale those practices across their operations.
Lessons for Scaling Cross-Functional Collaboration
To scale collaboration effectively, organizations must go beyond isolated successes and embed TPRM best practices throughout their operations. This begins with education and training to ensure all teams grasp the importance of TPRM. Case studies showcasing both the rewards of success and the risks of failure can be powerful tools for this purpose. Establishing dedicated communication platforms, like Microsoft Teams or Slack, and holding regular cross-team meetings to discuss progress, challenges, and lessons learned is another critical step. Actions and outcomes from these meetings should be documented centrally.
Cross-functional goals must align with broader organizational objectives, such as safeguarding data, enhancing customer satisfaction, and reducing costs. These targets should also be reflected in individual performance reviews to reinforce accountability. Technology plays a pivotal role by enabling vendor management software to centralize information, automate processes like vendor onboarding and risk tiering, and facilitate real-time risk monitoring.
Finally, fostering a culture of collaboration is essential. Workshops, communities of expertise, and mentoring programs can help make TPRM an integrated, ongoing practice rather than a one-off compliance task [1]. By embedding these practices, organizations can create a unified TPRM framework that not only strengthens cybersecurity but also supports excellence in patient care.
Conclusion: Building a Unified TPRM Framework in Healthcare
Creating a unified Third-Party Risk Management (TPRM) framework is crucial for safeguarding patient data and maintaining operational stability. The numbers paint a stark picture: while 80% of healthcare organizations are working toward technological transformation, only 23% report successful implementation across departments [9]. This gap highlights the pressing need for strong leadership, clear accountability, and effective technology solutions.
The foundation for addressing these challenges lies in three key areas: leadership commitment, shared accountability, and the right technology. Executive involvement plays a pivotal role, significantly increasing the chances of success [9]. Organizations that bring together cross-functional teams achieve technology adoption rates 34% higher than those using isolated approaches [9]. These aren't just incremental gains - they define the line between effective risk management and potential vulnerabilities.
To start, secure executive support and establish clear, cross-departmental accountability. For example, one hospital system cut implementation delays by 40% simply by creating a dedicated Slack channel for cross-functional teams [9]. Set shared goals that align with broader priorities like patient safety and data security, and use a unified dashboard to monitor progress. Include frontline users, technical experts, and administrative staff in implementation teams to ensure diverse perspectives shape your risk management strategy.
Technology is the backbone of effective TPRM. Centralized platforms can automate repetitive tasks, standardize vendor assessments, and provide real-time insights into risks across departments. Healthcare organizations using pilot projects for technology rollouts see adoption rates improve by 30% and implementation costs drop by 25% [9]. This phased approach allows teams to test workflows, gather feedback, and fine-tune processes before scaling up.
The most successful organizations weave TPRM into their daily operations through ongoing education, regular cross-team meetings, and clearly defined responsibilities. Breaking down silos between IT, legal, and clinical teams is essential - not just for meeting compliance standards but also for achieving operational excellence. By fostering collaboration, healthcare organizations can turn TPRM into a strategic tool that protects patients, builds strong vendor relationships, and enhances resilience against emerging risks.
FAQs
How can IT, legal, and clinical teams work together effectively in third-party risk management (TPRM)?
Effective collaboration between IT, legal, and clinical teams in Third-Party Risk Management (TPRM) hinges on clear communication and well-established roles. Regular cross-departmental meetings are essential for aligning priorities, exchanging insights, and ensuring that everyone is moving toward shared goals. Teams should work together to define objectives centered on cybersecurity, compliance, and patient safety, as these priorities form the backbone of successful teamwork.
Adopting standardized tools - such as risk assessment templates, dashboards, and reporting platforms - can help simplify processes and improve visibility across departments. Fostering an environment of mutual respect and ongoing learning ensures that every team appreciates the unique challenges and expertise each group brings to the table. By collaborating effectively, these teams can identify potential risks, craft mitigation strategies, and maintain a steady flow of information to safeguard both the organization and its patients.
How does Censinet RiskOps™ improve third-party risk management in healthcare?
Censinet RiskOps™ takes the hassle out of third-party risk management by automating vendor assessments, speeding up onboarding, and providing continuous risk monitoring. It brings IT, legal, and clinical teams together, promoting a unified strategy for tackling cybersecurity, compliance, and operational issues.
With these features combined, healthcare organizations can cut down on inefficiencies, strengthen data security, and stay on top of regulatory requirements - all while boosting their ability to handle risks effectively.
Why is it essential to align third-party risk management (TPRM) with overall organizational goals in healthcare?
Aligning Third-Party Risk Management (TPRM) with an organization’s overarching goals is essential for creating a cohesive approach to managing risks. It ensures the protection of patient data, supports compliance with regulations like HIPAA, and bolsters the organization’s ability to operate smoothly under various challenges.
Collaboration is key here. When IT, legal, and clinical teams work together, it eliminates silos, simplifies processes, and allows risks to be addressed more efficiently. This unified effort doesn’t just improve cybersecurity - it also fosters trust among patients and stakeholders alike.
Related Blog Posts
- Third-Party Risk Management vs. Vendor Management: What Healthcare Leaders Need to Know
- Healthcare Third-Party Risk Management Trends 2025: What's Changing and Why It Matters
- Third-Party Risk Management vs. Vendor Management: What Healthcare Leaders Need to Know
- Healthcare TPRM Governance: Essential Board Reporting and Executive Oversight Strategies


