Emergency Department Vendor Risk: Critical Systems for Life-Saving Care
Post Summary
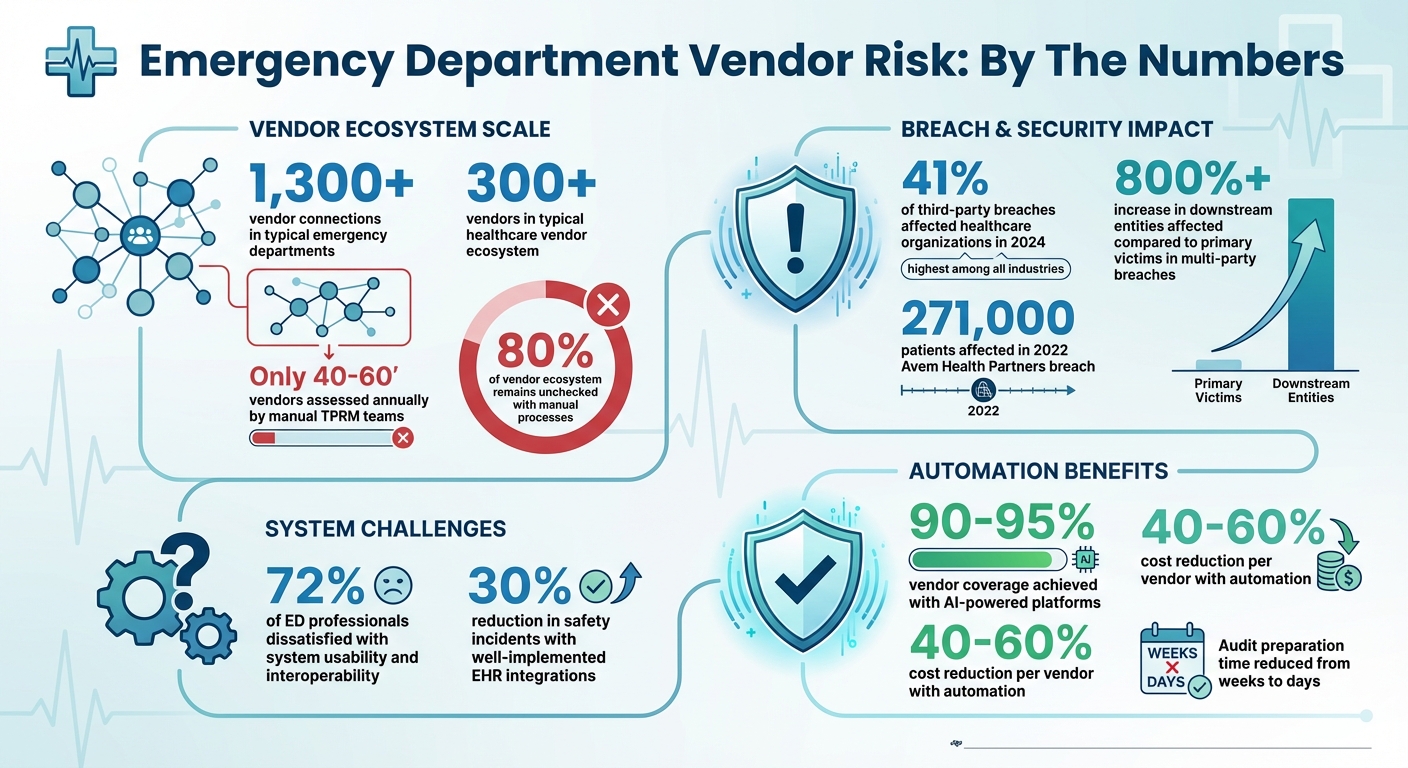
Emergency departments depend on vendor systems like EHRs, connected medical devices, and telemetry tools to deliver life-saving care. But these systems also create cybersecurity risks that can disrupt operations and compromise patient safety. Key challenges include:
- Cyberattacks on vendors: A single breach can impact entire healthcare networks, as seen in the 2022 Avem Health Partners data exposure affecting 271,000 patients.
- System vulnerabilities: Poor integration, outdated systems, and excessive access increase risks for ransomware, data breaches, and operational failures.
- Downtime risks: Failures in critical systems like pharmacy, PACS, and EMS data exchange delay care and escalate workloads.
To address these risks, emergency departments must prioritize secure vendor systems, enforce compliance with standards like HIPAA, and adopt automated tools for continuous risk monitoring and management. Without these measures, patient care and safety are at risk.
Emergency Department Vendor Risk Statistics and Impact on Healthcare
1. EHR Integrations
Real-Time Data Access Creates Critical Vulnerabilities
Electronic Health Record (EHR) integrations are the backbone of emergency department (ED) operations, giving physicians quick access to crucial patient information like medical histories, allergies, medications, and lab results. However, these connections come with risks. Every integration - whether linking ED software to hospital-wide EHR systems, lab information systems, radiology platforms, or pharmacy databases - creates an opening that cyberattacks can exploit.
The challenges are significant: 72% of ED professionals report dissatisfaction with system usability and interoperability[2]. Poorly designed integrations can lead to isolated data silos, limiting access to essential patient information. On the flip side, standalone ED systems that fail to connect with hospital EHRs, labs, and pharmacies can leave critical gaps in visibility and care coordination[2].
When done right, integrating these systems can dramatically improve patient safety. In fact, well-implemented EHR integrations have been shown to reduce safety incidents by up to 30%[4]. To achieve this, emergency departments need secure, open-standard integrations. EHR vendors that adhere to standards like HL7 and FHIR enable secure and seamless data sharing, which is vital in high-stakes environments like the ED. However, tools such as copy/paste functions, cloning, and templates - common in EHR systems - can introduce errors and increase liability risks if not managed carefully[3].
Strengthening EHR integrations isn’t just about improving workflows; it’s about protecting patients and ensuring life-saving care. By addressing these vulnerabilities and prioritizing secure, interoperable systems, emergency departments can mitigate risks and enhance outcomes.
2. Connected Medical Devices
Device Vulnerabilities Threaten Patient Safety in High-Stakes Environments
Connected medical devices like ventilators, infusion pumps, cardiac monitors, and defibrillators are indispensable in emergency care. But their reliance on connectivity introduces serious cybersecurity challenges. Research spanning three years, including findings shared by Scott Erven and Adam Brand, Associate Directors at Protiviti, at BSides San Francisco in 2015, revealed that many medical devices and healthcare systems are alarmingly vulnerable to direct cyberattacks. These vulnerabilities can jeopardize patient safety, especially in high-pressure environments like emergency departments. A single compromised device can lead to cascading failures, potentially disrupting critical care[5].
Addressing these risks requires a proactive approach throughout the device lifecycle - from design to post-production[6]. This means identifying potential hazards, assessing risks, implementing strong controls, and continuously monitoring for threats. Emergency departments should also rigorously evaluate vendors, choosing those with proven compliance with healthcare regulations, such as HIPAA, and robust audit trail capabilities[2]. These steps form the groundwork for integrating advanced technologies that bolster device security.
Looking forward, connected medical devices are becoming more cyber-resilient, offering real-time monitoring to reduce the impact of potential breaches[2]. Healthcare organizations must keep pace with evolving regulations, particularly regarding device interoperability and data privacy, to ensure their systems meet modern cybersecurity standards.
When patient safety is at stake, secure medical devices are not just a technical requirement - they are a cornerstone of effective and reliable care.
3. Telemetry and Monitoring Systems
Integration Gaps Create Critical Monitoring Gaps
Telemetry and monitoring systems play a crucial role in emergency departments, issuing life-saving alerts for cardiac arrhythmias and signs of clinical deterioration. These alerts are essential for quick diagnosis and timely intervention[9]. While these systems are designed to work alongside Electronic Health Records (EHR) integrations and connected medical devices, they also introduce challenges in vendor risk management. A striking 72% of emergency department physicians and managers express dissatisfaction with the usability and interoperability of their current IT systems[2]. When telemetry data doesn’t seamlessly integrate into EHRs via Clinical Decision Support tools, it can cost precious seconds - seconds that could make all the difference in patient outcomes[8][9]. These integration gaps expose critical weaknesses in system connectivity.
But the risks don’t stop at connectivity. Emergency departments increasingly depend on vendor-neutral platforms to consolidate patient data from various medical devices. While this centralization improves access to information, it also creates multiple security vulnerabilities when vendors fail to meet stringent security standards[7]. Poor integration not only slows down workflows but also increases the likelihood of errors at moments when precision is non-negotiable[2]. Additionally, EHR downtime compounds these issues, adding to staff workload and causing delays that leave monitoring systems unable to relay critical patient updates[2].
In response to these challenges, many emergency departments are raising the bar for their vendors. They are prioritizing solutions built on open standards like HL7 and FHIR, which enable real-time telemetry data sharing across platforms. These standards directly address the monitoring blind spots caused by proprietary systems[2]. Departments are also opting for systems equipped with fail-safe modes, cyber-resilience features, and enhanced real-time monitoring capabilities. These features are designed to maintain patient surveillance even when primary systems experience downtime, effectively mitigating the risks tied to integration and security failures[2].
The message is clear: without secure and reliable integration of telemetry and monitoring systems, emergency departments are left with dangerous gaps in patient care. When every second counts, these blind spots can have serious consequences.
4. Diagnostic Imaging and PACS
Regulatory Compliance Gaps Expose Patient Data
Diagnostic imaging systems and Picture Archiving and Communication Systems (PACS) play a crucial role in emergency departments. These systems handle sensitive imaging data, like X-rays and CT scans, and integrate seamlessly with Electronic Health Records (EHRs) to enable quick and accurate diagnoses. However, many vendors fail to meet regulatory standards, leaving vulnerabilities that can compromise patient privacy and disrupt care. In some cases, these gaps can lead to delays in delivering critical diagnoses.
Emergency departments face two primary risks when it comes to PACS: system downtime and privacy breaches. When imaging systems go offline, access to essential diagnostic information is delayed, potentially jeopardizing patient outcomes. On the other hand, failing to comply with HIPAA regulations can lead to costly legal and financial repercussions. To mitigate these risks, PACS must include features like audit trails and adhere to stringent data privacy requirements - features that are often missing in some vendor solutions.
The flow of diagnostic imaging data involves multiple interfaces within the emergency department's ecosystem. A single weak link in the security chain can create a ripple effect, jeopardizing the entire system. Given this interconnectedness, robust vendor risk management is non-negotiable. Many leading healthcare organizations now prioritize vendors with a proven history of meeting regulatory standards, ensuring interoperability, and offering scalable solutions. These organizations demand systems designed with data protection in mind right from the start.
Additionally, emergency departments are increasingly requiring PACS solutions to include cyber-resilience features in their contracts. These features might include fail-safe modes that ensure imaging data remains accessible during outages and real-time monitoring tools to identify potential security threats. With the regulatory environment constantly evolving to address data privacy, cloud hosting, and system interoperability, ongoing vendor evaluations are critical.
Without a strong focus on vendor risk management, emergency departments risk not only regulatory compliance issues but also operational disruptions that could directly impact patient care. Protecting diagnostic imaging systems is no longer optional - it’s essential for maintaining both privacy and functionality in high-pressure healthcare settings.[2]
sbb-itb-535baee
5. Pharmacy and Supply Chain Management
Medication Systems Create Cascading Vulnerabilities
Pharmacy and supply chain management systems in emergency departments play a crucial role in handling urgent medication orders and tracking inventory - both of which directly affect patient care. However, integrating these systems with EHRs and EDIS introduces multiple access points, potentially exposing sensitive patient data. A single weak link in this chain can disrupt the entire emergency department workflow, creating a ripple effect of challenges if operational protocols fail to address these vulnerabilities.
These systems are heavily reliant on their core EHR/EDIS platforms to function smoothly. If the primary system goes offline, processes like medication ordering, dispensing, and inventory management grind to a halt. This makes it essential for emergency departments to have robust downtime protocols and contingency plans in place to ensure uninterrupted access to critical medications. Unfortunately, many facilities still lack sufficient backup measures, leaving them exposed during system outages.
Adding to these complexities is the need for regulatory compliance. Pharmacy systems are required to maintain audit trails, adhere to HIPAA regulations, and facilitate real-time data sharing across various hospital departments. As noted by HealthCareSoftware.odoo.com [2], healthcare software must be designed from the ground up to support HIPAA compliance, maintain audit trails, and ensure patient safety. Vendors that fail to embed these safeguards into their systems risk exposing healthcare organizations to compliance violations, penalties, and potential legal issues.
These interconnected challenges highlight the importance of selecting the right vendors for pharmacy and supply chain management systems. Poor vendor choices can create vulnerabilities that extend beyond a single department, affecting the entire hospital's operations. Emergency departments must prioritize vendors that offer secure, interoperable solutions tailored to healthcare environments.
To address these needs, future vendor contracts should emphasize systems with features like fail-safe modes, cyber-resilience capabilities, and real-time threat monitoring. Integrations should support hospital-wide data flows using open standards like HL7 and FHIR. Rigorous evaluation of vendors for compliance, technical design, and operational resilience is essential to prevent disruptions that could jeopardize patient safety during critical emergencies.
6. Ambulance and EMS Data Exchange
Pre-Hospital Data Links Expand the Attack Surface
Emergency departments now depend heavily on real-time data sharing with ambulance and EMS systems to prepare for incoming patients. This connectivity undoubtedly enhances care coordination and speeds up treatment, but it also introduces vulnerabilities that extend beyond hospital walls. Every connection between pre-hospital data systems and hospital networks creates a potential weak spot. While this real-time link improves readiness, it also magnifies the risks posed by vendor-related security flaws.
A recent breach involving a third-party vendor shows just how damaging a single failure can be. Research reveals that in incidents involving multiple parties, the number of downstream entities affected can surpass the primary victims by over 800% [1]. This example underscores how a breach at one vendor can ripple through and compromise numerous healthcare organizations that rely on the same EMS data exchange provider.
The problem isn’t limited to technical vulnerabilities. System downtime adds another layer of risk. Even with strong internal defenses, vendor system weaknesses can expose sensitive data [1]. In 2024, 41% of third-party breaches impacted healthcare organizations [10], illustrating how cybercriminals increasingly target vendors as the weakest point in the healthcare supply chain. To protect these critical pre-hospital data streams, healthcare organizations must prioritize rigorous vendor risk assessments.
As emergency departments lean more on digital EMS data exchange, any disruption can lead to increased staff workloads and, more importantly, delayed patient care [2]. Without strong fail-safe measures and cyber-resilience, hospitals risk operational breakdowns. Frequent system outages or insufficient contingency plans can delay care during moments when every second is critical.
To address these challenges, healthcare organizations need to perform comprehensive vendor risk evaluations. These assessments should cover technical capabilities, compliance with industry standards, and operational resilience. Key steps include ensuring that EMS data exchange systems use secure integration protocols like HL7 and FHIR, maintain detailed audit trails, and have robust downtime contingency plans in place. Collaboration between compliance, security, IT, and legal teams is essential to thoroughly vet these systems [1].
7. Billing and Revenue Cycle Management
Financial Systems Create Hidden Vulnerabilities
Emergency departments rely heavily on billing systems to handle charges and process claims. These systems are intertwined with EHRs, patient registration platforms, and external payers, creating a broader attack surface. If a vendor's security measures are lacking, it can lead to downtime that halts revenue collection and results in financial losses. These gaps not only hit the bottom line but also bring regulatory hurdles and operational disruptions.
Healthcare software must comply with HIPAA, maintain detailed audit trails, and prioritize patient safety [2]. When billing vendors fail to meet these standards, hospitals could face regulatory violations - and the steep penalties that come with them.
Failures in billing platforms often push hospitals to rely on manual processes, which are prone to errors and delays [2]. Without strong backup plans, revenue losses during outages can become a serious threat.
To minimize these risks, organizations need to choose vendors with a solid track record, built-in compliance tools, fail-safe features, and resilience against cyber threats [2]. It’s essential to verify interoperability, audit capabilities, and downtime protocols, while also using dashboards to track billing metrics and stay ahead of potential financial or compliance issues. A reliable billing system isn’t just about finances - it’s a cornerstone of patient care, as disruptions in revenue can indirectly affect the quality of services hospitals provide.
Conclusion
The challenges posed by vulnerabilities in vendor systems have a direct and immediate impact on emergency care. With emergency departments juggling over 1,300 vendor connections, the sheer scale of these networks makes manual monitoring impractical and leaves significant gaps in oversight [10][12]. In 2024 alone, 41% of third-party breaches affected healthcare organizations - the highest among all industries [10]. When vendor failures or breaches occur, the consequences are severe: delays in diagnoses, inability to verify patient allergies, and even ambulance diversions [11].
Currently, manual Third-Party Risk Management (TPRM) teams can only assess around 40 to 60 vendors annually, leaving roughly 80% of a typical 300+ vendor ecosystem unchecked [11]. With vendor risk profiles changing multiple times a year due to breaches, financial instability, or leadership shifts [11], annual reviews fall short in addressing the dynamic nature of these risks. This creates a critical need for a more agile and comprehensive approach to vendor risk management.
The solution lies in continuous, intelligent automation. Platforms like Censinet RiskOps™ leverage AI to achieve 90–95% vendor coverage without increasing staff workloads, while also cutting costs per vendor by 40–60% [11]. These systems monitor third-party security signals, generate actionable tasks automatically, and integrate seamlessly into HIPAA compliance workflows. For example, when a breach is detected at a business associate, the platform flags the vendor’s most recent assessment, checks BAA compliance, and initiates an exception review - all without requiring manual intervention [11].
"Manual monitoring works to about 100 vendors. Beyond that, healthcare organizations need intelligent automation that routes, correlates, and workflows findings automatically while maintaining HIPAA compliance." - Atlas Systems [11]
This underscores the urgency of transitioning from traditional, periodic assessments to automated, continuous oversight. By adopting a tiered monitoring strategy that prioritizes high-risk vendors - such as EHRs, lab systems, and remote-access devices - organizations can allocate resources more effectively [11]. Additionally, the ability to generate continuous evidence shortens audit preparation times from weeks to just days [11], ensuring that healthcare providers can maintain patient safety and strengthen their resilience in an increasingly complex vendor landscape.
FAQs
What steps can emergency departments take to reduce cybersecurity risks from vendor systems?
Emergency departments can bolster their cybersecurity defenses against risks posed by vendor systems by conducting in-depth vendor risk assessments. This process helps uncover potential weak points and ensures that vulnerabilities are addressed early. Setting clear evaluation standards and keeping a close watch on vendor compliance are essential steps in maintaining a secure environment.
Equally important is implementing strict cybersecurity policies and ensuring vendors follow all applicable regulations. Regular audits play a vital role in verifying adherence to these standards. By focusing on these proactive measures, emergency departments can safeguard their critical systems and uphold patient safety.
How do open-standard integrations like HL7 and FHIR benefit emergency departments?
Open-standard integrations like HL7 and FHIR are game-changers in emergency departments, making it easier for systems to share data seamlessly. This connectivity ensures that healthcare providers can access accurate, up-to-date patient information when time is of the essence.
These tools also enable real-time patient tracking and quicker decision-making, both of which are crucial in delivering safe, efficient, and well-coordinated care during emergencies. By improving communication and cutting down delays, they allow emergency teams to concentrate on their top priority - saving lives.
Why is ongoing risk monitoring essential for patient safety in emergency departments?
In emergency departments, keeping a close watch on risks as they emerge is crucial. It helps spot and tackle weak points in vital systems before they lead to bigger problems. This kind of vigilance ensures that life-saving tools and procedures stay dependable, reducing the chance of mistakes and keeping patients safe in high-stress situations.
With ongoing risk checks, these departments can stay steady under pressure, address problems swiftly, and uphold the standard of care, no matter how intense the circumstances get.


