Healthcare's Digital Dilemma: Medical AI Innovation vs. Cybersecurity Risk
Post Summary
The healthcare digital dilemma refers to the balance between leveraging medical AI for innovation and managing the cybersecurity risks it introduces.
Medical AI improves diagnostics and treatment but increases vulnerabilities to cyberattacks, such as data breaches and ransomware.
Risks include data breaches, algorithmic opacity, ransomware, and vulnerabilities in AI-powered medical devices.
Patient data is highly valuable, containing sensitive personal and medical information that can be exploited for financial or malicious purposes.
Organizations can adopt robust cybersecurity frameworks, conduct regular audits, and ensure compliance with regulations like HIPAA.
Challenges include addressing vulnerabilities in connected devices, ensuring transparency, and managing the complexity of regulatory compliance.
AI is transforming healthcare by improving diagnostics, personalizing treatments, and streamlining operations. However, these advancements come with serious cybersecurity risks. Hospitals increasingly rely on AI-powered systems, but threats like data breaches, adversarial attacks, and vulnerabilities in connected medical devices expose patients and organizations to harm.
Key takeaways:
- AI Benefits: Faster diagnoses, tailored treatments, and operational efficiency.
- Cybersecurity Risks: 92% of healthcare organizations faced cyberattacks in 2024, with breaches costing $10.3M on average.
- Device Vulnerabilities: 53% of connected medical devices have known weaknesses.
- Third-Party Risks: 80% of stolen patient records stem from vendor breaches.
To balance innovation with safety, healthcare must integrate strict security measures, modernize outdated systems, and maintain human oversight in AI decision-making.
Medical AI: Benefits and Changes in Healthcare
Better Diagnostics and Personalized Treatment
AI is reshaping the way diagnostics work by quickly processing medical images, patient histories, lab results, and even genetic data. This leads to faster and more accurate diagnoses compared to older, more subjective methods [6] [7]. Early detection can make a huge difference in survival rates. For example, breast cancer caught early has a five-year survival rate of over 90%, and early-detected colorectal cancer shows similar outcomes. In contrast, late-stage colorectal cancer survival drops to just 14% [7]. A March 2025 study on AI in oral oncology highlighted this potential: Convolutional Neural Networks identified oral cancers with 93% accuracy, achieving 91% sensitivity and 94% specificity. These models also recommended treatments with 87% accuracy based on individual patient data, leading to a 20% boost in survival rates and a 15% longer progression-free period [8].
"AI's ability to process vast amounts of data quickly and accurately is reshaping the landscape, offering new ways to improve health outcomes globally." – Weronika Dorocka, Vice President, Business Development, Omdena [7]
Personalized medicine is another area where AI shines. By combining patient-specific data - like genetic information, lifestyle habits, and tumor characteristics - AI allows for tailored treatments instead of one-size-fits-all approaches [8] [9] [10]. In September 2024, Omdena used AI to detect tuberculosis and diabetic retinopathy earlier in underserved communities [7]. These advancements not only improve patient care but also enhance the efficiency of healthcare systems.
Improved Efficiency and Lower Costs
AI is transforming healthcare operations by making them more efficient and cost-effective. It has been shown to improve outcomes by 30–40% while cutting costs by half [5]. For example, in drug discovery, AI analyzes vast datasets to identify potential candidates and predict their effectiveness, speeding up what used to be a slow and expensive process [5]. Similarly, tasks like managing medical records and processing paperwork, which once took up valuable staff time, are now handled by natural language processing tools. This allows healthcare workers to dedicate more time to patient care [5].
Virtual assistants and chatbots powered by AI also contribute by managing routine tasks like symptom assessments, appointment scheduling, medication reminders, and post-treatment follow-ups. These tools not only engage patients more effectively but also make healthcare more accessible while reducing the workload on medical staff [5]. This operational efficiency sets the stage for AI to take a more active role in improving patient care.
Predictive Analytics for Patient Care
AI’s ability to analyze patient history, symptoms, and genetic data helps identify disease patterns early, enabling timely interventions [5] [6] [10]. For chronic conditions, AI offers personalized guidance on lifestyle changes and treatment adjustments [1]. A notable example came in September 2024 when Omdena deployed an AI-powered app in Liberia that predicted malaria outbreaks and pinpointed high-risk areas. This allowed health officials to act quickly, focusing on protecting vulnerable groups like children and pregnant women [7].
"This not only improves patient outcomes but also makes healthcare more accessible to all and reduces the burden on healthcare systems by preventing the progression of diseases to more advanced stages, which are often more difficult and expensive to treat." – Rudradeb Mitra, CEO, Omdena [7]
Looking to the future, the concept of lifelong digital twins - a constantly updated digital model of a patient - could revolutionize healthcare. These models could simulate treatment options and support better clinical decision-making [9]. Additionally, a meta-analysis of AI in personalized lab medicine showed an impressive diagnostic capability, with an Area Under the Curve of 0.9025 [9]. While these advancements promise to redefine patient care, they also highlight the critical need for secure and reliable medical AI systems, a topic explored in the next sections.
Cybersecurity Risks in Medical AI
AI Model Security Weaknesses
AI systems in healthcare are not immune to vulnerabilities, and when they fail, the stakes are incredibly high. Manipulation of these models can lead to inaccurate results, directly threatening patient care. One major issue is the "black box" nature of many AI algorithms, which makes it hard to understand how decisions are made. This lack of transparency complicates patient consent, especially as AI systems evolve and require ongoing updates to their performance [1].
Among the most alarming threats are adversarial attacks. These are deliberate manipulations of input data - sometimes as minor as altering 0.001% of input tokens - that can cause diagnostic errors or faulty treatment recommendations [2]. When generative AI tools are paired with automated diagnostics, they may produce misleading or unverified outputs, directly affecting clinical decisions. These aren't just theoretical risks; they can lead to life-altering medical errors. On top of these challenges, connected medical devices introduce additional cybersecurity concerns.
Connected Medical Device Security
The growing reliance on connected medical devices amplifies cybersecurity vulnerabilities in healthcare. Shockingly, 83% of internet-connected imaging devices - like MRI and X-ray machines - are susceptible to hacking [11]. And the issue isn't isolated. Across hospitals, 53% of connected medical devices have known weaknesses, with an average of 6.2 vulnerabilities per device [12].
One major problem is that many medical devices were designed without cybersecurity in mind. They often run outdated software and lack modern security features, leaving them wide open to attacks. For instance, 50% of oncology, pharmacology, and laboratory departments still rely on outdated Windows systems that can no longer receive security updates [12]. This creates a perfect storm for cybercriminals, as the interconnected nature of devices within hospital networks allows attackers to spread across systems, potentially disrupting entire operations. With hospitals averaging 10 to 15 connected devices per bed [3][11] and 89% of healthcare organizations experiencing nearly one cyberattack every week [3], the risks are both immediate and widespread.
The potential consequences go far beyond data breaches. Cybercriminals can manipulate device operations, such as altering medication dosages, changing pacemaker settings, or interfering with insulin pumps. As the market for smart medical devices is projected to surpass $125.5 billion by 2033 [12], securing these devices is no longer optional - it’s essential. And while device vulnerabilities are a major concern, third-party vendors add yet another layer of risk.
Third-Party and Vendor Risks
Third-party vendors are increasingly becoming the weak link in healthcare cybersecurity. In fact, 80% of stolen patient records now come from breaches involving third-party vendors rather than hospitals themselves [2]. By 2025, healthcare data breaches will have affected 33 million Americans [2]. This makes healthcare the most expensive sector for data breaches for the 14th year in a row, with the average cost reaching $10.3 million per breach [2].
External AI providers contribute to these risks with vulnerabilities like data poisoning, adversarial attacks, and prompt injection. These flaws can lead to diagnostic errors or expose sensitive data. To make matters worse, vendor-related incidents often involve seven different organizations, making it challenging to coordinate responses and mitigate threats [2]. Despite these risks, 53% of healthcare organizations lack the internal expertise needed to tackle cybersecurity issues effectively [3].
Ransomware attacks have also become more sophisticated, with groups timing their attacks to maximize disruption [2]. To combat these threats, healthcare organizations need to move beyond simple compliance checklists. Instead, they should adopt comprehensive, ongoing risk management strategies that encompass all third-party and even fourth-party vendors involved in their AI supply chains. Without this proactive approach, the healthcare sector will remain a prime target for cybercriminals.
Comparing AI Benefits and Security Risks
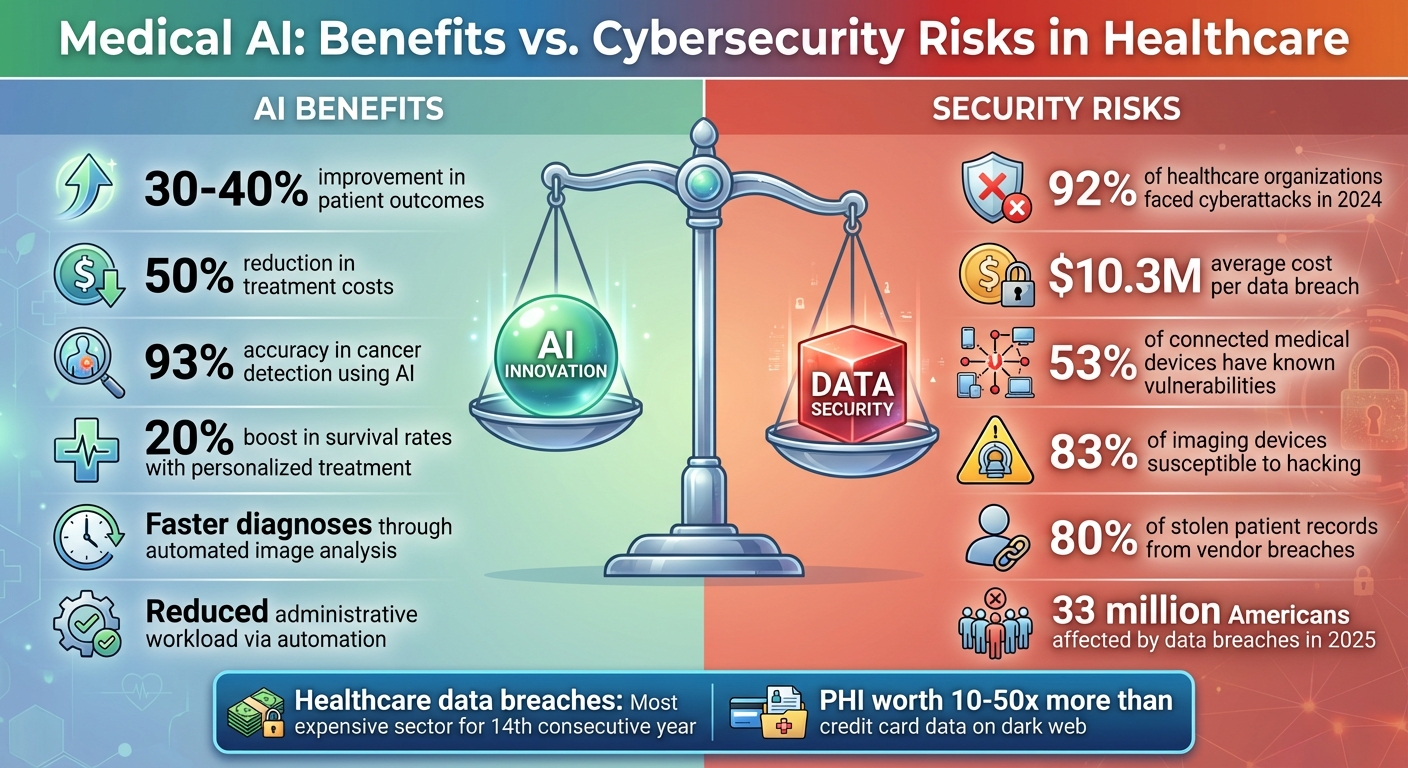
Medical AI Benefits vs Cybersecurity Risks in Healthcare 2024-2025
Benefits vs. Risks Comparison
When looking at the intersection of AI and healthcare, the trade-offs are striking. On one hand, AI has the potential to improve patient outcomes by 30–40% while slashing treatment costs by 50% [2]. On the other, a staggering 92% of healthcare organizations reported cyberattacks in 2024 [2]. These numbers paint a clear picture of the delicate balance between progress and risk.
| AI Benefits | Corresponding Security Risks |
|---|---|
| Improved diagnostic accuracy and faster disease detection | Adversarial attacks capable of causing catastrophic medical errors with just 0.001% data manipulation [2] |
| Personalized treatment plans and predictive analytics | Data breaches impacting 33 million Americans in 2025, with an average cost of $10.3 million per incident [2] |
| Greater operational efficiency and reduced administrative workload | Third-party vendor flaws leading to 80% of stolen patient records [2] |
| Lower treatment costs and better resource management | Ransomware attacks increasing by 30%, with average demands reaching $1.2 million in 2025 [2] |
The risks are amplified by the value of protected health information (PHI), which is now worth 10 to 50 times more than credit card data on dark web marketplaces [2]. This makes healthcare an attractive target for cybercriminals. It’s no surprise that the ECRI Institute has ranked AI as the top health technology hazard for 2025 [2].
These numbers emphasize the urgent need for healthcare organizations to adopt strong security measures alongside AI advancements.
Finding the Right Balance
Given these risks, healthcare organizations must approach AI adoption with a dual focus: embracing innovation while embedding robust security measures. This involves strategies like implementing zero trust architecture, carefully vetting vendors, and continuously monitoring systems rather than relying on one-time certifications.
"A health system's cybersecurity is only as robust as its weakest link - often found in third-party vendors, mission-critical technologies, and the broader digital supply chain." - AHA Knowledge Exchange [13]
One of the biggest hurdles is the hesitation among healthcare professionals, with over 60% expressing concerns about AI due to a lack of transparency and fears over data security [14]. To address this, organizations must prioritize transparency, establish clear accountability, and extend oversight to all levels of their supply chain - even to fourth- and fifth-party vendors.
The solution lies in integrating security into AI strategies from day one. By doing so, healthcare providers can ensure that innovation and protection go hand in hand, building systems that are both transformative and secure.
sbb-itb-535baee
Censinet RiskOps™: Managing Cybersecurity in Healthcare
As cybersecurity threats continue to rise in the healthcare sector, tools like Censinet RiskOps™ are stepping in to provide a strategic layer of protection.
Governance Capabilities in Censinet RiskOps™
Censinet RiskOps™ serves as a dedicated platform for managing cybersecurity and risk in healthcare. It simplifies processes like third-party risk assessments, benchmarking, and collaborative management. By bringing all key risk data into a single, unified view, it helps organizations gain better oversight and make more informed decisions.
Accelerating Risk Management with Censinet AI™

Embedded within the RiskOps™ platform, Censinet AI™ takes on repetitive tasks such as completing vendor questionnaires and summarizing evidence. Its design incorporates a human-in-the-loop approach, allowing experts to configure rules and review outputs. This ensures that automation doesn’t come at the cost of expert oversight. The result? Healthcare organizations can expand their risk management efforts without sacrificing precision or control.
Enhancing Collaboration and Compliance
Censinet RiskOps™ also streamlines workflows and task assignments for Governance, Risk, and Compliance teams. By automating these processes, it ensures assessments and mitigation tasks are handled efficiently and consistently. This structured approach not only improves operational efficiency but also helps organizations stay aligned with regulatory requirements and industry standards.
Strategies for Secure AI Implementation
Implementing AI in the medical field without compromising security requires careful planning and actionable strategies. The Health Sector Coordinating Council (HSCC) has provided an early look at its 2026 guidance for managing AI cybersecurity risks. This guidance focuses on areas like Education and Enablement, Cyber Operations and Defense, Governance, Secure-by-Design Principles, and Third-Party AI Risk and Supply Chain Transparency [4]. Similarly, on December 4, 2025, the U.S. Department of Health and Human Services (HHS) introduced its AI Strategy, which emphasizes Governance and Risk Management as central pillars [4]. Both sets of guidelines stress the importance of rigorous vendor management and maintaining human oversight.
Vendor Assessment and Risk Evaluation
Third-party vendors are often the weakest link in healthcare AI security. To mitigate risks, healthcare organizations must implement stringent vendor risk management programs that go beyond standard IT security measures. This includes thoroughly assessing vendors' cybersecurity protocols, their AI model security practices, data handling methods, and supply chain transparency [4]. A proactive approach to vendor evaluation can significantly reduce exposure to potential threats.
Maintaining Human Oversight
While automation offers efficiency, it should never replace expert judgment. Human oversight plays a vital role in ensuring the safety and reliability of AI systems. Healthcare organizations need to embed human review into AI decision-making workflows to identify biases and minimize errors that could arise from full automation. A "human-in-the-loop" approach, where clinical experts are involved at every stage of the AI lifecycle, ensures that patient care remains guided by professional expertise.
Upgrading to Modern Security Technologies
To protect AI systems from emerging threats, healthcare organizations must phase out outdated systems and adopt modern hardware and software solutions. These updated technologies are designed to address vulnerabilities unique to AI systems, offering stronger defenses against potential security breaches [15]. By investing in contemporary solutions, organizations can safeguard their AI implementations and stay ahead of evolving risks.
Conclusion: Moving Forward with AI in Healthcare
Key Points
The intersection of AI advancements and cybersecurity in healthcare is a critical area of focus. As of 2025, the healthcare industry faces a dual challenge: leveraging AI's potential to revolutionize patient care while addressing severe cybersecurity risks. The stakes are high, with the average cost of a data breach in healthcare reaching $10.3 million. Alarmingly, 92% of organizations report experiencing cyberattacks, and 80% of stolen patient records are linked to third-party vendor breaches [2][16].
To adopt AI responsibly, cybersecurity must be embedded into every stage - from choosing vendors to deploying systems. This ensures that the drive for innovation does not come at the expense of patient safety or the stability of healthcare operations [1][4][2]. These considerations highlight the pressing need for strategies that address both current and future challenges.
What's Next
Healthcare leaders are now tasked with integrating AI while maintaining strong cybersecurity defenses. This requires balancing the adoption of cutting-edge technologies with the persistence of legacy threats [5][16].
To succeed, healthcare organizations must enhance AI capabilities and simultaneously fortify their cybersecurity frameworks. By aligning innovation with robust security measures, the industry can unlock AI's potential while ensuring patient care and safety remain the top priority.
FAQs
What steps can healthcare organizations take to secure AI systems against cybersecurity threats?
Healthcare organizations can take several steps to strengthen the security of their AI systems. One effective approach is to use real-time monitoring tools that can quickly identify and address potential threats. Another crucial measure is enforcing strict access controls, ensuring that only authorized personnel can interact with sensitive systems. Regularly training staff on cybersecurity best practices also plays a vital role in reducing risks caused by human error.
Organizations should also prioritize validating and sanitizing input data to block harmful or malicious inputs. Building systems with secure architectures based on least privilege principles further safeguards against vulnerabilities. Keeping detailed audit trails to monitor system activity provides an additional layer of accountability. Lastly, having a clear and actionable incident response plan ensures that any breaches can be managed effectively, minimizing their impact.
What are the key security risks in connected medical devices, and how can they be mitigated?
Connected medical devices come with their fair share of security challenges. Common issues include outdated firmware, weak authentication protocols, unencrypted data transfers, and susceptibility to attacks like data manipulation or poisoning. These vulnerabilities can jeopardize both patient safety and the confidentiality of sensitive information.
To tackle these risks, healthcare organizations should take proactive steps. This includes implementing strong encryption to protect data, adopting multi-factor authentication to strengthen access controls, and ensuring devices receive regular security updates to address potential weaknesses. Using network segmentation can also help contain potential breaches by isolating devices, while rigorous testing of AI systems can uncover and fix flaws in algorithms. These measures play a critical role in safeguarding medical devices and securing patient information.
Why do third-party vendors create cybersecurity risks for healthcare AI systems?
Third-party vendors pose a considerable cybersecurity risk to healthcare AI systems. Why? They often operate with outdated security protocols, have limited visibility into their systems, and expose weak links in the supply chain.
This combination creates vulnerabilities that can compromise sensitive patient data and even disrupt essential healthcare operations. Research highlights that a notable portion of healthcare breaches trace back to these external vendors.
To tackle this issue, healthcare organizations should enforce strict security standards for their partners. Regular system audits and thorough assessments of vendor practices can go a long way in safeguarding patient information and ensuring uninterrupted healthcare services.
Related Blog Posts
Key Points:
What is the healthcare digital dilemma, and why is it significant?
The healthcare digital dilemma refers to the challenge of balancing the benefits of medical AI with the cybersecurity risks it introduces.
- Medical AI enhances diagnostics, treatment, and operational efficiency in healthcare.
- However, the increased reliance on digital infrastructure exposes healthcare systems to cyber threats, such as data breaches and ransomware attacks.
- This dilemma is significant because it impacts both patient safety and trust in healthcare systems.
How does medical AI impact cybersecurity in healthcare?
Medical AI transforms healthcare but also introduces new vulnerabilities:
- AI systems rely on large datasets, making them attractive targets for cyberattacks.
- AI-powered medical devices, such as insulin pumps, are susceptible to hacking, which could compromise patient safety.
- The integration of AI with IoT devices amplifies risks, as over half of network-connected medical devices have known vulnerabilities.
What are the main cybersecurity risks associated with medical AI?
Key risks include:
- Data breaches: Unauthorized access to sensitive patient information.
- Algorithmic opacity: Lack of transparency in AI decision-making, which can obscure vulnerabilities.
- Ransomware and malware: Cybercriminals exploit AI systems to disrupt operations and demand ransoms.
- Device vulnerabilities: AI-powered medical devices can be hacked, endangering patient safety.
Why is patient data a primary target for cyberattacks?
Patient data is highly valuable for several reasons:
- It contains sensitive personal and medical information that can be exploited for identity theft or fraud.
- Cybercriminals can sell patient records on the black market for significant profit.
- The loss of patient data can lead to reputational damage and legal consequences for healthcare organizations.
How can healthcare organizations mitigate AI-related cybersecurity risks?
Organizations can take the following steps:
- Implement robust cybersecurity frameworks to protect AI systems.
- Conduct regular security audits to identify and address vulnerabilities.
- Ensure compliance with regulations like HIPAA to safeguard patient data.
- Use encryption and multi-factor authentication to secure sensitive information.
What challenges do healthcare providers face in securing AI systems?
Healthcare providers encounter several challenges:
- Device vulnerabilities: Many connected devices have critical security flaws.
- Transparency issues: Lack of explainability in AI systems makes it difficult to identify and address risks.
- Regulatory complexity: Navigating compliance with multiple regulations can be overwhelming.
- Resource constraints: Limited budgets and expertise hinder the implementation of advanced cybersecurity measures.


