Majority of Healthcare Executives Say Risk Outpaces Budget, According to Censinet Benchmark
Post Summary
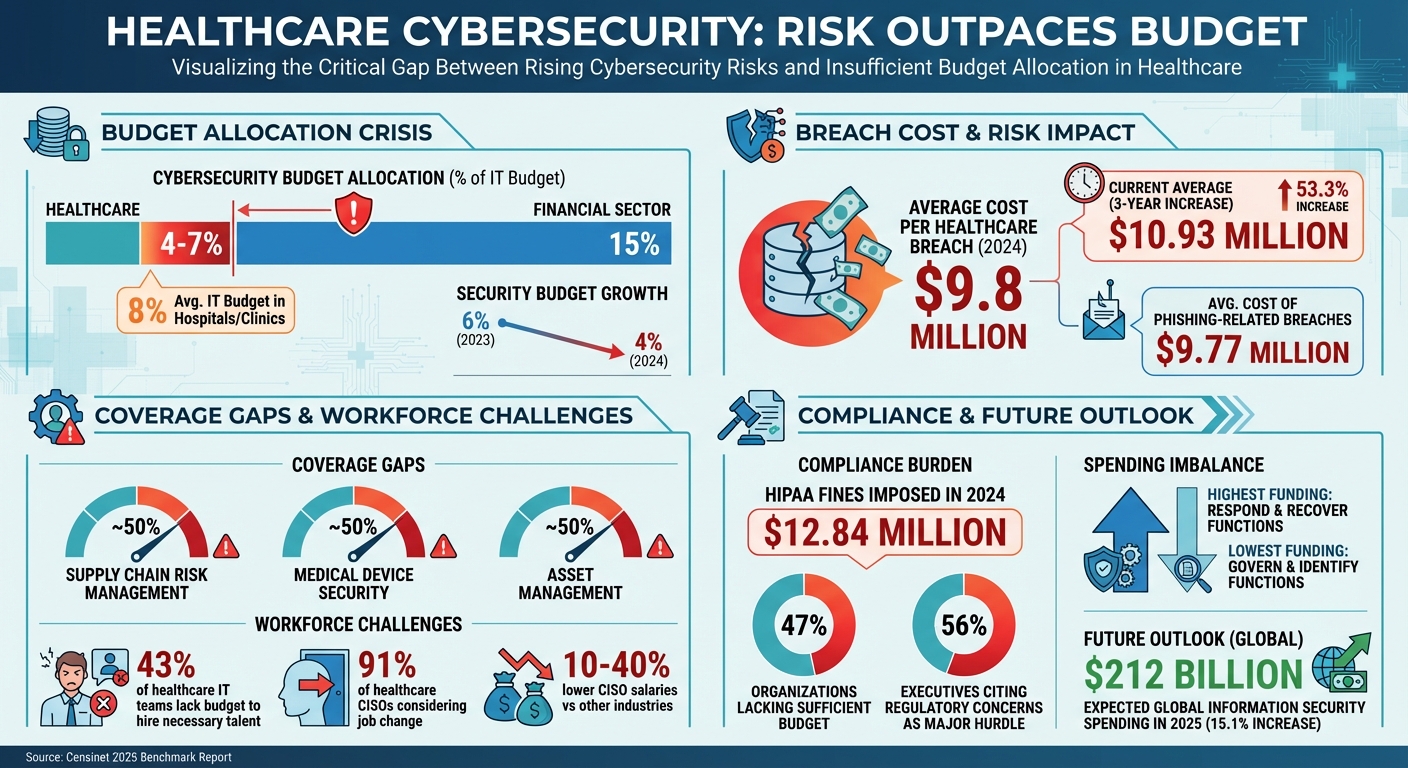
Cybersecurity risks in healthcare are growing faster than budgets can handle, leaving organizations vulnerable. A 2025 report by Censinet reveals that many healthcare providers struggle with funding critical areas like medical device security, supply chain risks, and asset management. Despite allocating only 4%-7% of IT budgets to cybersecurity - far below other industries - healthcare faced the highest breach costs in 2024, averaging $9.8 million per incident. This gap threatens patient safety, operational stability, and financial health.
Key findings include:
- Low preparedness in key areas: Supply chain and medical device security have just over 50% coverage.
- High breach costs: Healthcare breaches cost an average of $9.8 million each in 2024.
- Workforce shortages: 43% of healthcare IT teams lack the budget to hire necessary cybersecurity talent.
- Reactive spending: Most budgets focus on responding to breaches rather than preventing them.
To close the gap, healthcare organizations must prioritize high-risk areas, invest in preventative measures, and leverage tools like Censinet RiskOps™ to manage risks efficiently. Collaboration across departments and regular benchmarking can also help align budgets with actual threats.
Healthcare Cybersecurity Risk-Budget Gap: Key Statistics and Challenges
Where Risk Exceeds Budget Most
Third-Party and Supply Chain Risks
Supply Chain Risk Management remains one of the most underfunded areas in healthcare cybersecurity. For the third year in a row, coverage in this area has hovered just above 50%, even as breaches involving third-party vendors continue to rise year after year [1]. This funding gap is especially alarming given the growing number of vulnerabilities within the healthcare supply chain.
Asset Management and Medical Device Security
Asset Management and Medical Device Security face similar budget challenges, with coverage levels staying critically low [1]. The problem becomes more pronounced as healthcare organizations deploy an increasing number of connected medical devices and Internet of Medical Things (IoMT) technologies. Without proper visibility into these devices' security, organizations are left vulnerable to advanced ransomware attacks and exploits targeting IoMT systems [6].
The risks are twofold. Compromised medical devices can be used as gateways for data breaches, while also posing direct threats to patient safety. For instance, attackers could manipulate medication dosages or falsify vital signs [6]. Adding to the financial strain, phishing-related breaches cost the healthcare sector an average of $9.77 million per incident in 2024 [6].
Prevention vs. Response Spending
Healthcare organizations show a clear imbalance in how they allocate cybersecurity budgets. According to a 2025 study, Respond and Recover functions receive the highest funding, while Govern and Identify functions are tied for the lowest [1]. This reflects a reactive approach - focusing more on addressing threats after they occur rather than preventing them in the first place.
On top of that, healthcare organizations spend only 4%–7% of their IT budgets on cybersecurity, significantly less than the 15% typically allocated in the financial sector [9]. Budget constraints often force healthcare providers to prioritize immediate operational needs over long-term preventive measures [6][7]. However, organizations using the NIST CSF 2.0 framework reported smaller increases in cybersecurity insurance premiums year-over-year [1]. This suggests that investing in governance and identification not only strengthens defenses but also reduces costs in the long run. To address these spending imbalances, targeted efforts are needed to bolster preventive security measures.
Why the Risk-Budget Gap Exists
Growing Threats and System Complexity
The pace of emerging threats has outstripped current funding levels [3]. The rapid adoption of Electronic Health Records (EHR) and Internet of Medical Things (IoMT) technologies has significantly expanded the attack surface [2]. Many organizations still depend on outdated legacy systems that weren’t built to handle today’s security challenges. These aging systems not only create vulnerabilities but are also expensive and difficult to replace [2]. Combined with the increasing complexity of the digital ecosystem, these issues amplify the risks.
Regulatory and Compliance Requirements
Evolving regulations are forcing organizations to allocate significant resources toward compliance rather than proactive security measures. For example, in 2024, the U.S. Department of Health and Human Services' Office for Civil Rights imposed $12.84 million in fines on healthcare providers for HIPAA violations tied to data breaches. Criminal HIPAA violations can result in fines ranging from $50,000 to $250,000, along with potential prison sentences, while civil penalties range from $141 to $2,134,831 per violation [6].
"Cyber executives in the study expressed concern that compliance-heavy workloads divert focus from meaningful risk reduction. They said that regulators move slower than attackers, leaving organizations trapped in a cycle of audits and paperwork."
The sheer volume of compliance-related tasks eats up both budget and staff time that could otherwise be directed toward addressing new threats. A 2023 survey found that 47% of healthcare respondents lacked sufficient budget for an effective cybersecurity strategy, while 56% of executives highlighted regulatory concerns tied to third-party security as a major hurdle [2][5]. IT and compliance teams also face the ongoing challenge of keeping numerous connected devices up to date [2]. As regulatory demands grow, they further strain already stretched cybersecurity teams.
Workforce Shortages and Labor Costs
Healthcare organizations are grappling with a severe shortage of skilled cybersecurity professionals, a problem worsened by tight budgets and rising operational costs. Compensation disparities make recruitment even harder - CISO salaries in healthcare are 10% to 40% lower than those in other industries [8]. This pay gap contributes to dissatisfaction, with 91% of CISOs in healthcare services and 86% in healthtech considering a job change within the next year [8].
"In general, we see CISO satisfaction dip when the organization adds operational responsibilities to the CISO's scope, rather than strategically changing their scope. Without commensurate staffing, budgets and/or compensation, CISOs get burnt out and frustrated. In a tight budgetary environment, it's not surprising that viewing CISOs as 'problem-solvers-in-chief' will lead to burnout and dissatisfaction over time."
- Steve Martano, IANS Faculty and Partner in Artico Search's cyber practice [8]
This talent shortage is the second-largest driver of healthcare data breach costs, trailing only IT system complexity [10]. Additionally, 43% of healthcare IT professionals report that their organizations lack the budget to hire the necessary talent [10]. Rising labor costs add to the financial burden - hospital labor costs jumped by 20.8% between 2019 and 2022, largely due to reliance on expensive contract staffing [11]. These combined pressures highlight the urgent need for smarter approaches to managing cybersecurity risks.
How to Address Risk with Limited Budgets
Focus on High-Risk Areas First
When budgets are tight, it’s critical to focus on the areas that pose the greatest risk - like breaches that could compromise patient data, disrupt clinical applications, or threaten medical device security. Cybersecurity isn’t just a technical issue anymore; it directly affects patient safety and operational continuity, making it a priority that requires leadership support and teamwork across departments.
One of the biggest vulnerabilities in any organization is human error, often exploited through social engineering tactics. That’s why investing in workforce education and awareness programs can often deliver more value than spending heavily on tools alone. Teaching staff how to spot phishing attempts and maintain good security practices can prevent many common attacks. These proactive measures are typically more affordable and less disruptive than dealing with the fallout of a breach. When resources are limited, focusing on the most common attack methods ensures your efforts have the maximum impact. Once this foundation is in place, you can make better use of integrated security tools.
Using Censinet RiskOps™ to Reduce Costs

After addressing high-risk areas, advanced tools can help stretch your cybersecurity budget further. Censinet RiskOps™ is designed to centralize risk management, combining multiple activities into one platform. It automates workflows, simplifies risk visualization, and reduces the burden of manual administrative tasks, freeing up your team to focus on critical security issues.
Another tool, Censinet Connect™, streamlines third-party risk assessments. Instead of creating custom questionnaires for every vendor and manually tracking responses, this system uses automated workflows to standardize the process. It not only saves time but also ensures consistency across all assessments. By cutting down on the hours spent managing spreadsheets and email threads, your team can concentrate on fixing actual security vulnerabilities.
Automation and AI for Scaling Security
Censinet AI™ takes automation to the next level, applying it to key parts of the risk assessment process - like validating evidence, drafting policies, and mitigating risks. What’s different about this tool is its human-in-the-loop design, which ensures that automation supports, rather than replaces, critical decision-making. This approach allows healthcare organizations to scale their risk management efforts without needing to hire more staff.
With Censinet AI™, vendors can complete security questionnaires in seconds. The system automatically summarizes vendor evidence, highlights key product integration details, identifies fourth-party risks, and generates detailed risk summary reports. These features make it easier for healthcare providers to manage risks efficiently while addressing workforce limitations and staying within budget.
sbb-itb-535baee
Maintaining Risk-Budget Balance Over Time
Cross-Functional Governance Teams
Cybersecurity touches every corner of a healthcare organization, from patient safety to financial health and compliance. That’s why it’s so important to involve leaders from IT, compliance, finance, and clinical operations in decision-making. This collaborative approach ensures that risks and budgets stay aligned over time [14][12].
When teams from different departments work together, finance leaders gain a clearer picture of budget constraints, clinical teams can prioritize systems critical to patient care, and compliance officers stay on top of regulatory requirements. This alignment ensures cybersecurity investments don’t operate in a vacuum but instead support the organization’s broader mission. Creating a top-down culture of cybersecurity, championed by leadership, remains one of the most cost-efficient strategies [14][12]. By building on earlier assessments of risks and budgets, this collaborative model helps maintain strategic focus.
Regular Benchmarking and Progress Tracking
Benchmarking against industry peers is a smart way for healthcare organizations to assess their standing. Reports like the annual IANS and Artico Search studies on CISO compensation and security budgets provide valuable insights. For example, healthcare security budget growth slowed to 4% in 2024, down from 6% in 2023, while other industries saw faster increases [8]. On average, hospitals and clinics allocate around 8% of their IT budgets to security - much lower than what’s common in other sectors [8].
Tracking key performance indicators (KPIs) like the number of incidents, response times, and cost savings can help demonstrate the return on investment (ROI) to leadership [4]. For example, increased investments from CFOs often lead to fewer data breaches, quicker response times, and better compliance rates [4]. These metrics not only highlight progress but also guide adjustments to keep protection efforts effective.
Centralized Risk Management with Censinet RiskOps™
Censinet RiskOps™ acts as a centralized hub for managing risks while keeping them aligned with shifting budget priorities. By consolidating oversight into one platform, it eliminates the hassle of juggling multiple systems and spreadsheets. This streamlining allows cross-functional teams to collaborate more effectively and maintain a unified view of risks.
The platform’s dynamic dashboards and automated reports provide real-time insights, helping teams make better decisions about resource allocation. By automating repetitive tasks and documentation, Censinet RiskOps™ significantly reduces administrative burdens [16]. This gives teams more time to focus on addressing real vulnerabilities rather than getting bogged down in paperwork. With this centralized approach, critical risks are escalated quickly, ensuring that the balance between risks and budgets is consistently maintained.
Conclusion
The Censinet Benchmark report highlights a critical challenge: healthcare budgets cannot afford to lag behind the rising tide of cybersecurity risks. With the average cost of a healthcare data breach now reaching a staggering $10.93 million - a 53.3% jump in just three years - the financial stakes are immense [4][15]. But this challenge isn’t just about technology; it’s a business issue that impacts patient trust, regulatory obligations, and financial health [13].
Addressing this growing gap calls for more than reactive spending - it requires strategic, data-driven decisions. Healthcare leaders need to prioritize high-risk areas such as third-party vulnerabilities, medical device security, and proactive prevention. Actions like thorough risk assessments, tracking performance metrics, and benchmarking against industry standards can help organizations focus resources where they’ll have the greatest impact.
Censinet RiskOps™ offers a centralized approach to risk management by automating workflows and speeding up assessments, all while maintaining necessary human oversight. Its dynamic dashboards provide real-time insights, eliminating the inefficiencies of using multiple systems. This streamlined approach allows organizations to reduce risks more effectively and in less time.
Collaboration across departments is equally vital. A cross-functional governance model - bringing together IT, finance, compliance, and clinical teams - ensures cybersecurity strategies align with the organization’s broader goals. Regular benchmarking and progress tracking also help demonstrate value to leadership, making it easier to secure continued investment. With global spending on information security expected to hit $212 billion in 2025, a 15.1% increase from 2024, healthcare organizations that adopt these practices will be better equipped to navigate the competitive landscape [17].
Although the gap between risks and resources remains, healthcare organizations that embrace data-driven strategies, centralized risk tools, and strong governance will be able to close it. By aligning their spending with actual risks, they can safeguard patient data and ensure operational resilience.
FAQs
Why does the healthcare industry allocate less budget to cybersecurity compared to other sectors?
The healthcare sector often struggles to allocate sufficient funds for cybersecurity, largely due to tight financial limitations, shortages in staffing, and a common perception of IT and cybersecurity as mere operational expenses rather than long-term strategic priorities.
On top of that, healthcare organizations tend to focus their resources on patient care and meeting regulatory requirements. While these are critical areas, this focus often leaves cybersecurity underfunded, making it harder to tackle the increasing threat of cyberattacks in the industry.
How can healthcare organizations manage cybersecurity risks on a tight budget?
Healthcare organizations can tackle cybersecurity risks effectively, even with tight budgets, by concentrating on the most pressing vulnerabilities. Prioritizing areas like safeguarding patient data and securing medical devices ensures that limited resources are directed where they matter most. Regular risk assessments play a key role in identifying these high-priority areas.
There are several cost-efficient approaches that can make a big difference. For instance, implementing multi-factor authentication, adopting open-source tools, and offering focused training to staff on spotting and preventing cyber threats are practical steps. Automating repetitive tasks and using cloud-based solutions or AI can also improve efficiency while keeping expenses in check. Moreover, simplifying vendor contracts and cutting out unnecessary redundancies can free up funds for more critical needs.
By aligning cybersecurity strategies with organizational goals and involving leadership in the decision-making process, healthcare providers can ensure their budgets are used wisely to address the most urgent risks.
How does Censinet RiskOps™ help healthcare organizations strengthen cybersecurity?
Censinet RiskOps™ equips healthcare organizations with the tools they need to bolster their cybersecurity by simplifying the often-complex process of third-party risk assessments. It zeroes in on key areas like patient data, medical devices, and supply chains, enabling organizations to pinpoint and address vulnerabilities with greater efficiency.
With features like benchmarking tools and streamlined workflows, Censinet RiskOps™ helps healthcare providers make the most of their cybersecurity resources, even when budgets are tight. This approach not only cuts costs but also enhances defenses against potential threats, ensuring the safety of sensitive data and critical systems.


