75% Faster Credentialing, 80% Faster Audits: Real Results from Healthcare GRC AI
Post Summary
AI is transforming healthcare governance, risk, and compliance (GRC) by cutting credentialing times by 75% and audit preparation by 80%. Traditional manual processes are slow, costly, and prone to errors, delaying provider onboarding and increasing compliance risks. By automating repetitive tasks like document verification and real-time compliance monitoring, AI reduces inefficiencies, enhances accuracy, and allows professionals to focus on higher-value activities.
Key results:
- Credentialing reduced from 90–150 days to as little as 23–38 days.
- Audit workflows accelerated from weeks to minutes.
- Data entry errors decreased by 80%.
- Compliance maintenance improved by 32%.
AI tools like intelligent document processing (IDP) and predictive analytics streamline workflows, ensuring faster, more reliable outcomes while maintaining human oversight. This shift enables healthcare organizations to save time, lower costs, and improve patient care.
Main Challenges in Credentialing and Auditing
Credentialing Process Bottlenecks
Healthcare credentialing is often bogged down by mountains of paperwork and disconnected systems. Specialists can end up spending as much as 80% of their day chasing down documents and verifying information - a process that feels endless. Micah Schultz, a credentialing specialist from a large medical group in Boston, shared his experience:
"Before AI, I spent nearly 80% of my workday tracking documents - it was a relentless paperwork chase." [6]
The process of primary source verification doesn't make things any easier. Tasks like making phone calls or sending letters are time-consuming, and the hurdles only grow with differing state regulations and shifting federal standards [13][7][2]. On top of that, siloed operations between HR, credentialing, and scheduling departments create information gaps that slow everything down even further [7]. It’s not uncommon for expired licenses to be discovered at the last minute, leading to frantic rescheduling and potential staffing shortages [7].
These inefficiencies don’t just stop at credentialing - they spill over into auditing as well.
Audit and Compliance Workflow Problems
Auditing in healthcare faces its own set of challenges, with fragmented systems and outdated, reactive processes being the biggest culprits. Many organizations juggle compliance tasks across multiple platforms - billing compliance on one system, coding checks on another, and denial management through spreadsheets and emails [10]. This patchwork approach leads to duplicated work, communication breakdowns, and inconsistent data [10].
"Traditional audits tend to happen after the fact, identifying issues months after claims are submitted. In today's fast-paced regulatory climate, that reactive approach is no longer sufficient."
The administrative burden is staggering, especially for audits involving HIPAA, OCR, and the Joint Commission. External payer audits surged in 2023, further straining organizations still relying on manual processes to meet tight deadlines [10]. Without constant oversight, inaccuracies in network data can slip through, exposing organizations to regulatory penalties [9]. Manual auditing also comes with its own risks - human errors like typos or missed outliers become more common as auditors grow fatigued from repetitive tasks [10].
Time and Cost Impact
The delays caused by inefficiencies in credentialing and auditing take a heavy toll on healthcare operations and, ultimately, patient care. Credentialing alone can take anywhere from 90 to 150 days, costing roughly $7,500 per day. These delays can lead to revenue losses of more than $1.8 million for a single provider [2][9]. Clinical documentation and coding discrepancies add to the financial strain - 37% of healthcare organizations report a loss of at least $1 million, with 12% estimating losses exceeding $5 million [11].
Labor costs are another major concern. Sixty percent of healthcare administrators spend more than half their day on primary source verifications, a task prone to errors and data inconsistencies [9]. Despite this, 52% of healthcare organizations still rely on manual credentialing workflows [2]. With physician shortages expected to reach 86,000 by 2036 [2], these inefficiencies directly affect patients' access to care. Alarmingly, only 9% of healthcare leaders feel "very confident" that their organization is capturing all the revenue it should [11].
How AI Speeds Up Credentialing and Auditing
AI Technologies for GRC
AI is reshaping healthcare governance, risk, and compliance (GRC) by combining machine learning (ML), natural language processing (NLP), and automated workflows. These tools handle repetitive and time-consuming tasks that often bog down processes. For instance, NLP can process unstructured documents like licenses and certifications, automatically extracting key details. Meanwhile, machine learning identifies patterns, predicts risks, and spots irregularities that could signal compliance problems or fraud.
Predictive analytics adds another layer of efficiency by anticipating potential issues, such as flagging licenses that are about to expire weeks in advance. AI systems also integrate with real-time data sources, such as state medical boards and the National Practitioner Data Bank, allowing instant verification instead of waiting days - or even weeks - for responses.
These technologies form the backbone of AI-driven improvements in credentialing and auditing.
AI Applications in Credentialing
Credentialing often faces delays due to manual data extraction from PDFs, faxes, emails, and scanned documents. AI-powered intelligent document processing (IDP) tackles this challenge by automating data extraction, reducing errors by up to 80% [2]. These systems also integrate with primary data sources, significantly cutting down verification times - a task that previously consumed half a business day for 60% of administrators [9].
Beyond individual tasks, AI optimizes entire credentialing workflows. It can verify licenses across multiple states, check sanctions databases, and handle multi-payer onboarding requirements - all at once. Organizations using real-time AI systems have reported a 32% improvement in staying compliant [2], and AI-driven credentialing has been shown to reduce processing times by 50% [2].
While credentialing benefits greatly, AI also brings transformative changes to auditing.
AI Applications in Auditing
AI takes the efficiency gains seen in credentialing and applies them to audit processes. Instead of scrambling to gather documentation when an audit is announced, AI enables continuous evidence collection. It automatically maps controls to regulatory requirements and tracks compliance in real time across standards like HIPAA, Joint Commission guidelines, and payer-specific rules. This proactive approach replaces the traditional reactive model, where issues might only surface months after claims are submitted - often too late to avoid penalties.
AI audit tools also analyze billing patterns and coding accuracy in real time, flagging discrepancies immediately. By reducing human error in repetitive review tasks and providing predictive risk analysis, AI allows organizations to focus on areas with the highest regulatory or financial risks. This targeted approach ensures compliance efforts are directed where they’ll have the most impact.
Measured Results: 75% Faster Credentialing, 80% Faster Audits
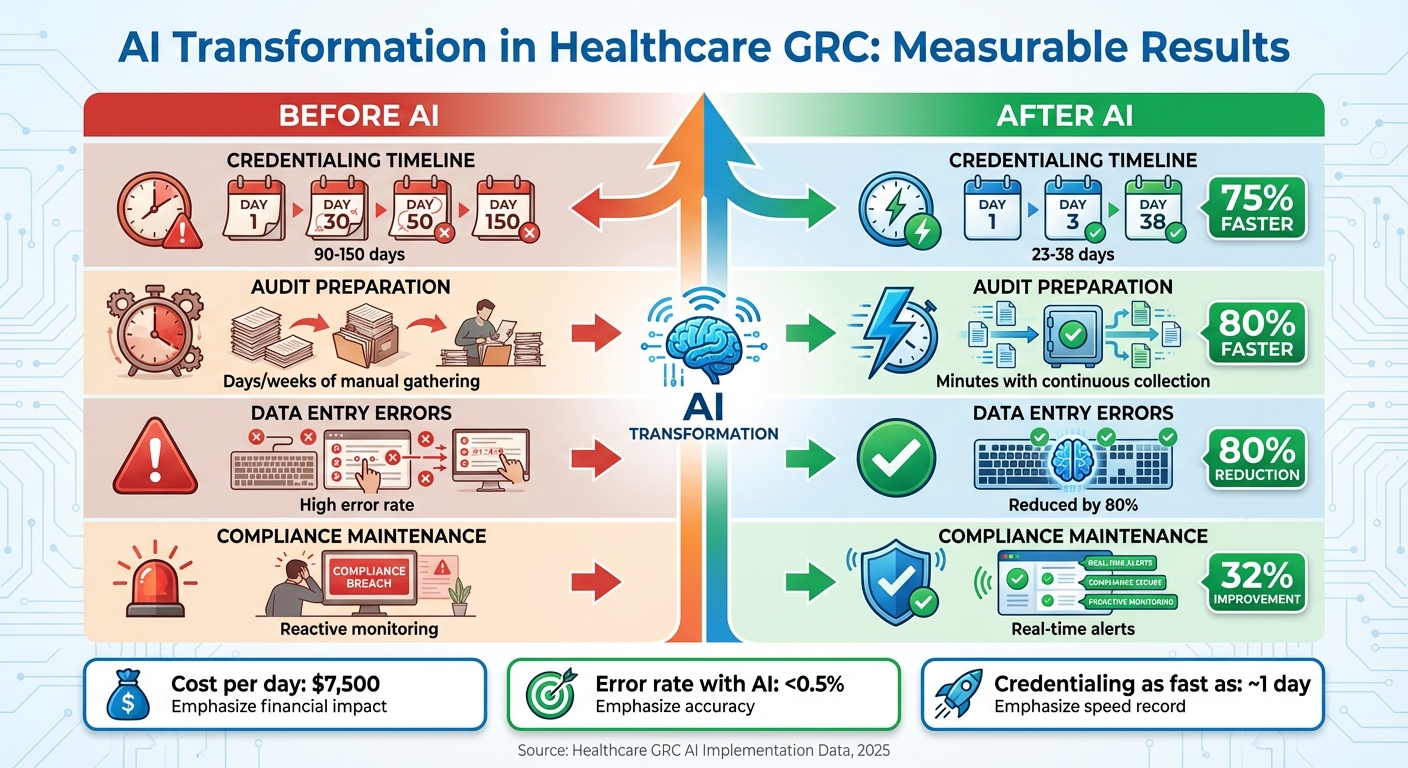
AI Impact on Healthcare Credentialing and Auditing: Before vs After Performance Metrics
Baseline Metrics Before AI Implementation
The challenges of manual processes in healthcare credentialing and auditing come with steep costs and delays. Traditionally, credentialing took an average of 90 to 150 days [2][12], costing about $7,500 per day [2]. Manual data entry across multiple systems often led to high error rates, which increased compliance risks [2][4]. On top of that, staying updated with ever-changing regulations - like those from CMS, state, and federal mandates - added significant expenses, amounting to $150 million for every $10 billion in revenue [5]. When it came to audits, organizations frequently found themselves scrambling to gather documentation only after audit announcements, making workflows reactive and inefficient.
Performance Improvements with AI
AI has dramatically changed the game, cutting credentialing time by up to 75% and slashing audit preparation time by 80%. Healthcare organizations leveraging AI have reduced credentialing timelines to as little as one day in some cases [12], a stark contrast to the months-long processes of the past. Similarly, audit workflows have seen an 80% acceleration, allowing organizations to achieve compliance readiness in record time. Verifiable's CVO services, as of September 2025, set a new standard with a ~1-day credentialing turnaround and an error rate of less than 0.5%, showcasing the impact of integrating AI with their in-house team [12].
| Metric | Before AI | After AI | Improvement |
|---|---|---|---|
| Credentialing Timeline | 90–150 days | 23–38 days | Up to 75% faster |
| Audit Preparation | Days/weeks of manual gathering | Minutes with continuous collection | 80% faster |
| Data Entry Errors | High (manual process) | Reduced by up to 80% | 80% reduction |
| Compliance Maintenance | Reactive monitoring | Real-time alerts | 32% improvement |
Real-time AI systems have also improved compliance maintenance by 32% [2], while intelligent document processing has reduced manual data entry by up to 80% [12]. These advancements lead to tangible operational benefits, including quicker provider onboarding, fewer staffing gaps, and better access to care for patients.
Productivity and Compliance Benefits
AI is reshaping how healthcare teams work, enabling staff to shift their focus from repetitive tasks to more strategic responsibilities. Credentialing specialists, for example, now dedicate their time to activities like analysis, exception handling, and building relationships instead of routine data entry [12]. As Janan Dave, VP of Operations at Verifiable, puts it:
"AI isn't here to replace the human element - it's here to collaborate, making our jobs more efficient and allowing us to focus on the work that truly matters" [12].
"The ROI is clear: lower labor costs, faster billing, and a significant reduction in compliance risks" [12].
Organizations with integrated IT-GRC systems report 50% fewer security incidents and achieve compliance with 30% fewer resources compared to those using fragmented methods [15]. AI-powered systems also reduce alert volumes by 61%, with a low false negative rate of 1.36% in risk management [14]. This allows teams to concentrate on real threats instead of wasting time on irrelevant alerts.
sbb-itb-535baee
Implementing AI in Healthcare GRC with Censinet
Step-by-Step AI Implementation Plan
Bringing AI into healthcare for credentialing and auditing is no small task, but a phased approach can make the process smoother and more effective. Start with Phase 1: Foundational automation and data normalization. This phase is all about automating repetitive tasks like data entry and primary source verifications (PSV). By doing this, you create a consistent and reliable data layer that serves as the backbone for more complex processes down the line. Be sure to select AI tools specifically designed for healthcare, keeping in mind the importance of meeting regulatory and payer requirements [8].
Once the foundation is in place, move on to Phase 2: Smart assistance. Here, AI takes on a more active role by analyzing data, spotting discrepancies, and even suggesting decisions based on established policies and historical trends. This lets credentialing specialists focus their expertise on areas that require human judgment and insight [8]. Finally, in Phase 3: Autonomous workflow operations, AI steps up to manage entire workflows independently. This frees up human specialists to tackle higher-level tasks like auditing outcomes, fostering relationships, and conducting in-depth analyses while the AI handles the routine work [8].
When choosing tools, look for systems that are user-friendly, include compliance tracking for standards like TJC, NCQA, and CMS, integrate effortlessly with existing healthcare systems, and scale to meet the needs of a growing organization [4]. This phased approach paves the way for solutions like Censinet RiskOps™, which we’ll explore next.
How Censinet Supports Healthcare GRC
Censinet RiskOps™ acts as a centralized hub for healthcare organizations to manage governance, risk, and compliance on a large scale. The platform simplifies critical tasks like third-party and enterprise risk assessments, cybersecurity benchmarking, and collaborative risk management. These features are essential for staying compliant while also speeding up workflows.
Censinet AITM takes things a step further by streamlining the third-party risk assessment process from start to finish. Vendors can complete security questionnaires in seconds, while the system automatically compiles evidence, tracks integration details, monitors fourth-party risks, and generates detailed risk reports. These capabilities build on the efficiency gains described earlier, offering continuous improvements powered by AI.
The platform strikes a balance between automation and human oversight. Tasks like evidence validation, policy drafting, and risk mitigation are guided by automation, but risk teams maintain control through customizable rules and review processes. Findings and related tasks are routed to the appropriate stakeholders for review and approval, ensuring that automation enhances decision-making rather than replacing it. These operational upgrades naturally evolve into stronger compliance and governance controls, which we’ll discuss below.
Healthcare Compliance and Governance Controls
For automated credentialing systems, compliance with HIPAA is non-negotiable. This includes using bank-level encryption, multi-factor authentication, and real-time monitoring. Censinet RiskOps supports these requirements by generating real-time compliance reports and alerting teams to issues like expired credentials or missing information [4].
AI also plays a key role in fraud detection. By cross-referencing credentialing data with trusted sources such as SAM.gov and the National Provider Identifier database, machine learning algorithms can uncover suspicious patterns [2]. With all this data presented in a user-friendly AI risk dashboard, Censinet RiskOps ensures that the right teams address the right issues at the right time, maintaining continuous oversight and accountability.
To make the most of these tools, ongoing training and strong IT support are essential. Staff need regular training to stay proficient with automation tools, resolve technical issues, and adapt to system updates [4]. This combination of advanced technology and skilled personnel delivers the speed and compliance improvements that healthcare organizations demand.
Tracking and Maintaining AI-Driven Results
Key Performance Indicators for Healthcare GRC
To measure AI's effectiveness in credentialing and auditing, healthcare organizations rely on key performance indicators (KPIs). These metrics help identify bottlenecks, address inefficiencies, and manage timelines more efficiently [16]. For credentialing, critical KPIs include:
- Initial cycle time: Typically 90–120 days.
- Application completeness rates: Ideally above 80% on the first submission.
- Payer enrollment success: A target of over 85%.
In auditing, useful metrics include audit readiness scores, response times to compliance inquiries, and the ratio of automated to manual reviews. These indicators provide a clear picture of how well AI tools are performing.
Delays in credentialing can be costly - a 60-day delay, for instance, can result in losses amounting to hundreds of thousands of dollars [16]. This is why many organizations closely monitor the cost per initial credentialing application, which usually ranges from $750 to $3,000. Achieving 100% regulatory compliance is also a top priority. Accurate data collection, regular reporting, and accountability are essential for keeping KPIs on track. Tools like dashboard reporting offer real-time insights, allowing organizations to address issues before they escalate [16].
Once KPIs are in place, a continuous improvement process ensures AI systems remain efficient and effective.
Continuous Improvement Process
AI systems need regular updates to stay aligned with evolving requirements. Conducting quarterly risk assessments - or assessments triggered by significant IT or regulatory changes - helps ensure AI tools remain relevant [17]. In fact, 62% of organizations report that AI has significantly boosted their compliance efficiency. Gartner forecasts that by 2025, more than half of major enterprises will rely on AI and machine learning for continuous regulatory compliance checks [1].
It’s important to choose AI solutions that can adapt and improve over time. Regular monitoring of AI GRC tools, combined with input from credentialing specialists and compliance teams, is key to refining processes. This collaborative approach ensures that technology enhances, rather than replaces, expert judgment. Frequent performance feedback and staff involvement play a vital role in maintaining the effectiveness of these systems [16].
Short-Term and Long-Term Performance Comparison
Tracking metrics over time provides measurable insights into AI's impact. Here’s how performance can improve:
| Metric | 90-Day Results | One-Year Outcomes | Target Benchmarks |
|---|---|---|---|
| Credentialing Cycle Time | 120–150 days | 90–105 days (approx. 30% reduction) | 75–90 days (further acceleration) |
| Application Completeness Rate | 65–70% | 85–90% | Above 90% |
| Payer Enrollment Success | 70–75% | 88–92% | Above 90% |
| Audit Response Time | 5–7 business days | 1–2 business days (70% reduction) | Same-day response (up to 80% faster) |
| Compliance Committee Approval Rate | 85–88% | 93–96% | 95%+ |
| Cost Per Credentialing Application | $2,500–$3,000 | $1,200–$2,000 | $750–$1,500 |
Conclusion: Achieving Better Efficiency and Compliance with AI
AI-powered GRC solutions are transforming how healthcare handles credentialing and auditing. The results are hard to ignore - credentialing speeds up by 75%, and audits are completed 80% faster. These improvements not only cut costs but also reduce compliance risks and help ensure patient safety.
Relying on manual processes introduces risks to both compliance and patient care. AI shifts this outdated, reactive approach to a proactive system. It continuously monitors credentials, flags expiring licenses in real time, and cross-checks multiple databases to catch issues before they escalate [4][3].
Censinet RiskOps™ is a prime example of how AI can scale risk management without sidelining human expertise. With Censinet AI™, vendors can complete security questionnaires in seconds instead of weeks. Risk teams maintain control through customizable rules and manual review processes, blending automation with human oversight. This approach empowers healthcare leaders to manage risks faster and with greater precision.
Healthcare organizations face a maze of regulations, from HIPAA to state-specific requirements. AI-driven GRC solutions take the burden off staff by automating compliance checks, tracking regulatory updates, and identifying obligations. This not only protects patient data and clinical operations but also allows staff to focus on more impactful tasks.
For those still using spreadsheets and manual workflows, the next step is clear. AI-driven GRC solutions aren't just about speeding up processes - they provide a sustainable way to maintain compliance, reduce risks, and improve patient care. By adopting this forward-thinking approach, healthcare organizations can stay agile and compliant in a constantly evolving regulatory environment.
FAQs
How does AI help reduce credentialing time by 75% in healthcare?
AI has transformed credentialing by automating tedious tasks like data extraction and document handling. It allows for real-time verification of credentials, quickly identifies discrepancies, and simplifies workflows. As a result, onboarding timelines shrink from weeks to just days - or even hours.
By cutting down on manual work and improving accuracy, AI not only speeds up the process but also boosts compliance and lowers the chances of human error. This shift is reshaping how healthcare organizations manage credentialing.
How does AI enhance healthcare audit processes?
AI is transforming healthcare audits by simplifying intricate processes and boosting precision. Some standout technologies include real-time monitoring, which flags compliance issues as they occur, and predictive analytics, which helps foresee potential risks. Pattern recognition plays a key role in sifting through massive datasets to spot anomalies. On top of that, automated data extraction and verification accelerates document reviews, while AI-powered compliance analysis ensures regulatory standards are met with higher accuracy. These tools collectively enable healthcare organizations to work more efficiently and minimize mistakes in their audit processes.
What obstacles do healthcare organizations face when adopting AI for Governance, Risk, and Compliance (GRC)?
Healthcare organizations face a variety of hurdles when integrating AI into governance, risk, and compliance (GRC) efforts. These challenges include navigating intricate regulations like HIPAA, safeguarding sensitive information through robust cybersecurity measures, and dealing with fragmented or disconnected risk management systems. On top of that, ensuring high-quality, accurate data remains essential for AI to perform as intended.
To tackle these issues, organizations should focus on building effective data governance frameworks, offering thorough training for staff, and setting up oversight mechanisms to address potential biases and maintain compliance. By addressing these pain points head-on, healthcare providers can harness AI to streamline credentialing, audits, and broader risk management tasks with greater efficiency.
Related Blog Posts
- AI-Powered GRC: How Leading Organizations Are Automating Compliance in the Age of Increasing Regulation
- How Leading Health Systems Reclaimed 3,000 Staff Hours Monthly with GRC Automation
- Why 92% of Healthcare Organizations Are Failing at GRC Integration - And How AI Changes Everything
- How AI Agents Reduce Provider Credentialing from 120 Days to 30 - Without Compromising Quality


