The Business Case for Healthcare TPRM: Cost Savings and Risk Reduction Statistics
Post Summary
TPRM programs reduce costs, mitigate risks, and ensure compliance, making them essential for safeguarding patient data and maintaining operational resilience.
TPRM minimizes breach-related expenses, reduces vendor assessment inefficiencies, and prevents operational disruptions.
TPRM mitigates risks related to data breaches, regulatory non-compliance, and vendor performance failures.
TPRM ensures adherence to regulations like HIPAA by enforcing vendor contracts, conducting risk assessments, and monitoring compliance.
TPRM programs save money by preventing costly breaches, reducing downtime, and optimizing vendor management processes.
By quantifying cost savings, demonstrating risk reduction, and aligning TPRM with organizational goals, healthcare leaders can justify TPRM investments.
Healthcare organizations manage an average of 1,300 vendors, exposing them to significant risks like data breaches and operational disruptions. A strong Third-Party Risk Management (TPRM) program not only reduces these risks but also saves money. Here's why:
- Cost Savings: Organizations using managed TPRM services can save up to $380,000 annually compared to in-house programs. Automation cuts vendor onboarding timelines and reduces staffing needs.
- Risk Reduction: Third-party breaches account for 60% of healthcare data breaches, costing $9.8 million per incident on average. Effective TPRM programs lower breach costs and improve response times.
- Efficiency Gains: Automated tools cover 90-95% of vendors, compared to manual processes that assess only 40-60 vendors annually.
Cost Savings from Healthcare TPRM
Measured Savings from TPRM Programs
A well-structured TPRM program can lead to substantial financial savings. For instance, a mid-sized company running an in-house TPRM program typically spends between $400,000 and $500,000 annually. This figure includes costs for personnel, technology, and assessments [1]. On the other hand, opting for managed TPRM services can reduce the Total Cost of Ownership (TCO) to around $120,000 per year for managing up to 50 vendors. That’s a potential savings of up to $380,000 annually [1].
The financial impact becomes even clearer when comparing breach costs. Organizations leveraging AI and automation report an average breach cost of $3.84 million, compared to $5.72 million for those without such tools - a difference of $1.88 million [3]. In the healthcare sector, the average cost of a data breach is even higher, at $9.8 million per incident [3]. Alarmingly, in 2023, 60% of these breaches were linked to third-party vendors [4], underscoring the importance of a solid TPRM program to prevent such costly incidents.
Healthcare organizations have also reported 10% to 15% reductions in vendor-related expenses by consolidating vendors, renegotiating contracts, and streamlining management processes through effective TPRM strategies [3]. These savings not only reduce costs directly but also contribute to minimizing associated risks.
Lower Operational Costs
Automation within TPRM programs offers another layer of cost efficiency by significantly reducing operational expenses. Currently, 52% of companies spend between 31 and 60 days on third-party control assessments, while 38% take between 61 and 90 days [2]. These lengthy timelines consume valuable resources and delay vendor onboarding. Automation can drastically shorten these processes, freeing up staff to focus on critical risk management efforts.
Staffing shortages add another layer of complexity. Sixty-two percent of organizations cite understaffing as their biggest challenge in protecting against third-party breaches. On average, companies would need to double their third-party security teams to meet current demands [2]. To address this, 77% of organizations use vendor management software, and 54% are exploring AI solutions that automate questionnaire responses by leveraging existing data [2]. These technological advancements reduce manual workloads and help organizations avoid the high costs of expanding their teams unnecessarily.
Risk Reduction Metrics and ROI from TPRM
Key Risk Reduction Metrics
Healthcare organizations that adopt third-party risk management (TPRM) programs often see noticeable improvements in their overall security. 87% of organizations focus on reducing risk exposure, especially since breaches involving third parties tend to cost 40% more than internal incidents [2].
Without proper oversight, organizations face significant challenges, including operational disruptions (84%), financial losses (66%), regulatory scrutiny (60%), and reputational damage (59%) [2]. These numbers make it clear: effective TPRM not only safeguards daily operations but also helps maintain trust and credibility.
One valuable tool in this process is cybersecurity ratings, which provide ongoing assessments of security performance. Lower ratings are often linked to higher chances of successful attacks [5]. By tracking these ratings over time, organizations can gain a better understanding of how well their TPRM strategies are working [5].
Ultimately, these metrics do more than just enhance security - they pave the way for financial benefits as well.
ROI from Healthcare TPRM
The financial benefits of TPRM programs are hard to ignore, especially when paired with the measurable risk reduction they provide.
A staggering 96% of organizations report a positive return on investment (ROI) from their third-party risk management efforts [2]. This confidence highlights the tangible advantages of proactively addressing vendor-related risks.
For example, integrating threat intelligence into TPRM processes allows organizations to respond to incidents 30% faster, cutting down on dwell time and reducing the impact of breaches [5]. These faster response times directly lead to lower costs and quicker recoveries.
The growing value of TPRM is also reflected in the market's rapid expansion. It's projected to grow from $7.41 billion in 2024 to $27.84 billion by 2032, with an annual growth rate of 18.2% [1]. This growth underscores how industries are increasingly recognizing the importance of managing third-party risks effectively.
Centralized vs. Hybrid TPRM Models
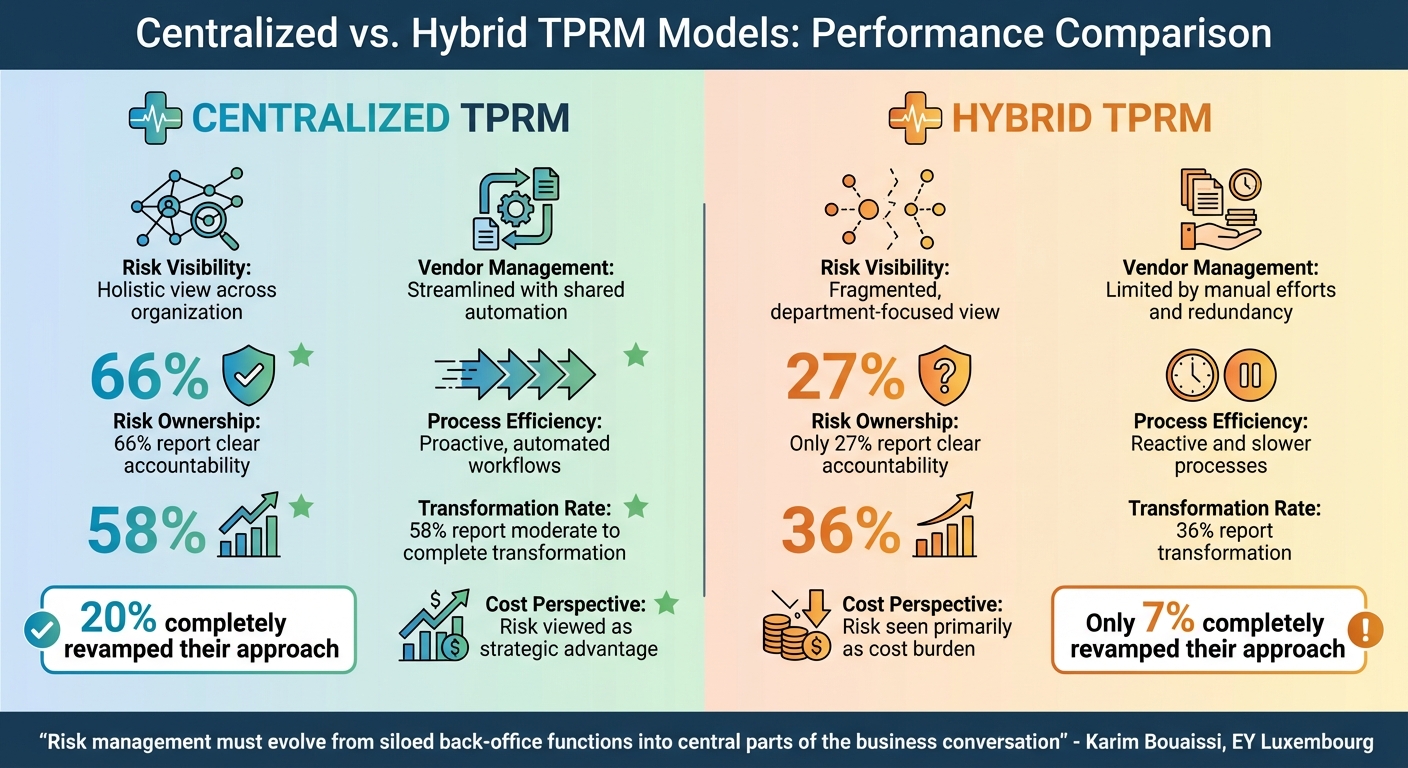
Centralized vs Hybrid TPRM Models: Key Performance Metrics Comparison
Benefits of Centralized TPRM
Organizations using a centralized Third-Party Risk Management (TPRM) model enjoy notable advantages in managing their third-party relationships. By breaking down silos, centralized models provide a holistic view of risks across the entire organization. The numbers back this up: 58% of centralized TPRM users report a moderate or complete transformation in their approach, compared to just 36% of those using siloed methods. Even more compelling, 20% of centralized users have completely revamped their approach, compared to only 7% of their counterparts [7].
Centralized models encourage collaboration across departments, ensuring that everyone operates from the same framework rather than conducting separate, disconnected evaluations. This unified approach leverages shared automation practices, minimizes inefficiencies from manual processes, and enhances accountability by enabling quicker identification and resolution of incidents [6][7]. Beyond improving risk management, these models also contribute to cost savings and better return on investment, as previously discussed.
"Risk management can't just be about compliance checklists or static risk registers. It must be about keeping the business resilient when everything hits at once. Our research shows that companies are facing nonlinear, fast-moving, interconnected risks, from supply chain shocks to cyberattacks. These events don't wait their turn. They hit simultaneously and create ripple effects across the organization. This is why enterprise risk management (ERM), and third-party risk management (TPRM) must evolve from siloed back-office functions into central parts of the business conversation."
- Karim Bouaissi, EY Luxembourg Consulting Partner – Cyber & Digital Risk [7]
While centralized models offer a clear edge in oversight and efficiency, some organizations choose hybrid models to strike a balance between centralized coordination and localized autonomy.
Hybrid TPRM Models: Pros and Cons
Hybrid models aim to blend centralized oversight with decentralized control, giving individual departments more independence while maintaining some level of coordination. This approach is particularly appealing for organizations with diverse operations or complex regulatory landscapes.
However, this flexibility comes with challenges. Only 27% of hybrid model users report clear risk ownership, compared to 66% in centralized systems. Additionally, just 25% of hybrid users indicate that their Chief Risk Officer holds equal standing with other C-suite executives, a stark contrast to the 76% in centralized models [7]. Hybrid setups often lead to duplicated efforts, reactive assessments of vendors, and fragmented information flow [6][7]. While they may allow for localized cost management, they frequently fall short in delivering the unified risk oversight needed for robust cybersecurity management. Organizations focusing solely on controlling immediate costs may overlook the broader benefits and resilience that a centralized strategy can provide [7].
Comparison Table: Centralized vs. Hybrid TPRM Models
| Factor | Centralized TPRM | Hybrid TPRM |
|---|---|---|
| Risk Visibility | Holistic view across the organization [6][7] | Fragmented, department-focused view [6][7] |
| Vendor Management | Streamlined with shared automation [6] | Limited by manual efforts and redundancy [6][7] |
| Risk Ownership | 66% report clear accountability [7] | Only 27% report clear accountability [7] |
| Process Efficiency | Proactive, automated workflows [6][7] | Reactive and slower processes [6][7] |
| Transformation Rate | 58% report moderate to complete transformation [7] | 36% report transformation [7] |
| Cost Perspective | Risk viewed as a strategic advantage [7] | Risk seen primarily as a cost burden [7] |
sbb-itb-535baee
How Censinet RiskOps™ Improves TPRM Efficiency
Overview of Censinet RiskOps™
Censinet RiskOps™ serves as a centralized platform tailored for healthcare organizations to manage third-party and enterprise risks. It acts as a unified hub where organizations can conduct risk assessments, benchmark cybersecurity practices, and collaborate on risk management efforts. The platform addresses a wide array of risks, including those tied to patient data, protected health information (PHI), clinical applications, medical devices, and supply chains - all from a single, easy-to-navigate command center that provides clear risk visualization.
Whether deployed internally, fully managed, or in a hybrid model, the platform adapts to healthcare organizations of all sizes. This flexibility lays the groundwork for AI-driven automation, which further simplifies and speeds up the risk assessment process.
AI-Driven Risk Assessment Automation
Censinet AI™ takes over tedious tasks, allowing vendors to complete security questionnaires in just seconds. The tool goes beyond simple automation by summarizing evidence, integrating product details, identifying fourth-party exposures, and producing detailed risk reports.
This system doesn’t eliminate human oversight - it enhances it. Risk teams retain control through customizable rules and review processes, ensuring that automation supports decision-making rather than replacing it. By managing tasks like evidence validation and policy drafting, the platform allows healthcare organizations to scale their risk management efforts without sacrificing quality. The result? Faster risk mitigation, reduced operational costs, and improved ROI, all while maintaining the level of precision required to safeguard patient care and safety.
Real-Time Dashboards and Risk Insights
RiskOps™ builds on its automated features by offering real-time dashboards that provide instant visibility into risks. Acting as a centralized hub, it aggregates real-time data into clear, actionable insights across all third-party relationships. Advanced routing and orchestration features ensure that critical findings and tasks are automatically directed to the appropriate stakeholders for swift review and action.
This streamlined approach ensures nothing falls through the cracks, maintaining continuous oversight and accountability. With all AI-related policies, risks, and tasks displayed in one unified dashboard, healthcare leaders have a reliable source of truth. This empowers them to make faster, more informed decisions regarding vendor relationships and risk mitigation. By consolidating data and simplifying workflows, RiskOps™ strengthens the case for adopting efficient third-party risk management strategies.
Conclusion
Healthcare organizations can no longer afford to treat third-party risk management (TPRM) as a mere formality. The numbers tell a concerning story: manual TPRM teams typically evaluate only 40 to 60 vendors each year, despite managing ecosystems with more than 300 vendors. This leaves around 80% of vendors unchecked, creating a significant gap in oversight. To make matters worse, annual assessments leave an eight- to 11-month window where critical risks could go unnoticed [8].
The advantages of automated TPRM are hard to ignore. Organizations that adopt modern monitoring solutions can achieve 90% to 95% vendor coverage - without needing to expand their teams [8]. This represents a major leap forward in protecting patient data and managing costs effectively.
Censinet RiskOps™ offers a powerful solution by combining AI-driven automation with real-time risk visibility. It eliminates the inefficiencies of manual processes, allowing healthcare organizations to scale their risk management efforts without adding staff or inflating budgets. By automating evidence validation, directing critical findings to the right stakeholders, and centralizing decision-making through intuitive dashboards, RiskOps™ turns TPRM into a strategic advantage rather than a resource drain. This shift aligns perfectly with the broader trends discussed throughout this analysis.
The message is clear: healthcare organizations need to modernize their TPRM processes now. With proven cost savings, enhanced risk management, and operational efficiency, tools like Censinet RiskOps™ are essential for those committed to protecting patient safety while ensuring financial stability. The time to act is now.
FAQs
How does automating TPRM help cut costs and reduce risks?
Automating Third-Party Risk Management (TPRM) takes the hassle out of key tasks like vendor onboarding, conducting assessments, and tracking risks. By cutting down on manual work, it not only saves time but also trims labor costs.
What’s more, automation reduces assessment fatigue by streamlining workflows, making the entire process smoother. It also ensures round-the-clock monitoring to spot potential risks as they arise. This proactive approach can help you avoid expensive data breaches and operational hiccups, safeguarding both your finances and your reputation.
What are the advantages of using a centralized TPRM model instead of a hybrid approach?
A centralized TPRM (Third-Party Risk Management) model offers consistent oversight, uniform risk assessments, and reliable data, which can translate into cost savings and minimized risks. By cutting out redundancies, this model simplifies processes, boosts efficiency, and ensures a unified method for handling third-party risks.
In contrast to hybrid models, which can lead to disjointed workflows and oversight gaps, a centralized approach allows for continuous monitoring and provides clearer, actionable insights. This helps organizations build a more cohesive and effective risk management strategy.
How does TPRM help healthcare organizations respond to risks more quickly?
Third-Party Risk Management (TPRM) plays a critical role in helping healthcare organizations address risks efficiently. By automating essential processes such as vendor onboarding, risk assessments, and ongoing monitoring, TPRM simplifies workflows and ensures potential vendor risks are identified and managed without delay.
This automation minimizes manual effort and enhances visibility into possible issues, allowing healthcare providers to make faster, more informed decisions. The result? Stronger compliance measures and better protection of sensitive patient information.
Related Blog Posts
- Third-Party Risk Management ROI Calculator: Prove Your Program's Value to Healthcare Executives
- The Business Case for Healthcare TPRM: Cost Savings and Risk Reduction Statistics
- Third-Party Risk Management ROI Calculator: Prove Your Program's Value to Healthcare Executives
- TPRM Technology Stack for Healthcare: Tools, Platforms, and Integration Strategies
Key Points:
What is the business case for TPRM in healthcare?
- Third-Party Risk Management (TPRM) is essential for healthcare organizations to manage vendor risks, reduce costs, and ensure compliance.
- It safeguards sensitive patient data, prevents operational disruptions, and strengthens resilience against cybersecurity threats.
- TPRM transforms risk management from a compliance checkbox into a strategic capability that supports organizational goals.
How does TPRM reduce costs in healthcare?
- Minimizes breach-related expenses: Data breaches in healthcare cost an average of $10.93 million, making TPRM a critical cost-saving measure.
- Reduces inefficiencies in vendor assessments: Automated TPRM tools streamline vendor evaluations, saving time and resources.
- Prevents operational disruptions: Effective TPRM ensures vendors meet performance standards, avoiding costly downtime.
What risks does TPRM address in healthcare?
- Data breaches: TPRM mitigates risks associated with third-party vendors handling Protected Health Information (PHI).
- Regulatory non-compliance: TPRM ensures adherence to HIPAA, HITECH, and other healthcare regulations.
- Vendor performance failures: Continuous monitoring identifies and addresses vendor issues before they impact operations.
How does TPRM improve compliance in healthcare?
- Enforces vendor contracts: TPRM ensures vendors comply with contractual obligations, including breach notification and data protection requirements.
- Conducts risk assessments: Periodic assessments verify vendor compliance with security standards and regulations.
- Monitors compliance: Continuous monitoring ensures vendors maintain compliance throughout the contract lifecycle.
What are the financial benefits of TPRM?
- Prevents costly breaches: By addressing vulnerabilities proactively, TPRM reduces the likelihood of expensive data breaches.
- Reduces downtime: Ensures vendors meet performance standards, minimizing disruptions to patient care.
- Optimizes vendor management: Automated tools save time and resources, allowing organizations to focus on high-risk vendors.
How can healthcare organizations secure executive buy-in for TPRM?
- Quantify cost savings: Demonstrate how TPRM reduces breach-related expenses and operational inefficiencies.
- Showcase risk reduction: Highlight how TPRM mitigates risks to patient data and compliance.
- Align with organizational goals: Position TPRM as a strategic investment that supports patient safety and operational resilience.


