Healthcare Vendor Risk and Medicare Advantage: CMS Star Ratings Impact
Post Summary
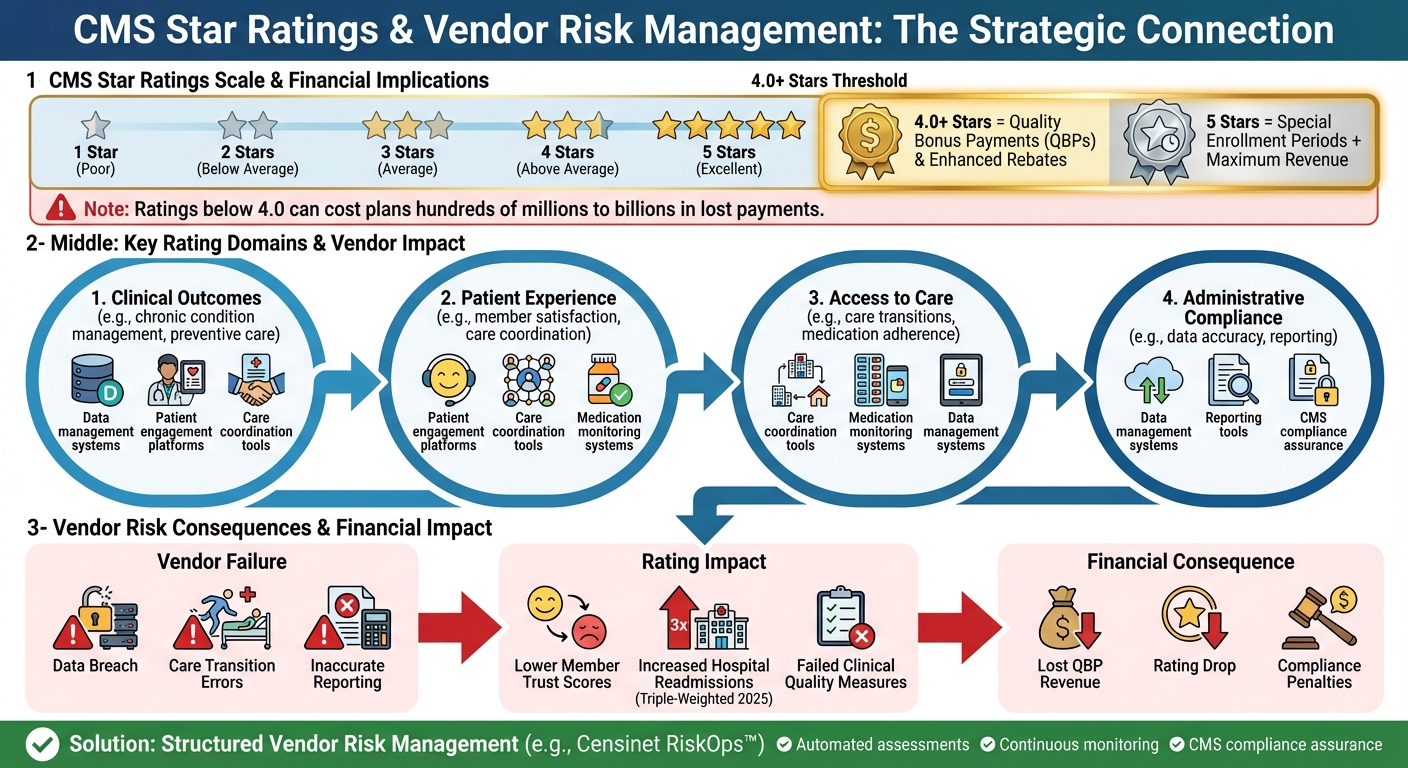
To succeed in Medicare Advantage, plans must excel in CMS Star Ratings, which directly influence revenue through Quality Bonus Payments (QBPs) and rebates. Plans achieving 4.0 stars or higher gain financial advantages and attract more members. However, changes in CMS criteria now emphasize clinical outcomes, patient experience, and health equity, while reducing focus on administrative measures. This raises the stakes for maintaining high ratings.
Third-party vendors are critical in supporting these efforts but also pose risks. Failures like data breaches or compliance errors can harm ratings and financial stability. For example, vendor underperformance in care transitions could increase hospital readmissions, now a triple-weighted measure for 2025.
To mitigate these risks, Medicare Advantage plans are turning to structured vendor risk management solutions like Censinet RiskOps™. These platforms streamline assessments, automate workflows, and ensure vendors meet CMS standards. Effective vendor oversight not only protects against setbacks but also drives improvements in Star Ratings, unlocking financial rewards and market competitiveness.
How Vendor Risk Impacts Medicare Advantage CMS Star Ratings and Revenue
CMS Star Ratings: Key Measures and Vendor Risk Connections
CMS Star Ratings Criteria Explained
The CMS Star Ratings system uses a 1–5 scale to evaluate Medicare Advantage and Part D plans, helping beneficiaries compare options on the Medicare Plan Finder website [9][10]. These ratings reflect how well plans deliver care and meet member expectations, serving as both a quality benchmark and an incentive for plans to enhance their services [9][10].
The ratings are based on several key domains, such as clinical outcomes, patient experience, access to care, and administrative compliance. These domains include measures like chronic condition management, preventive care, medication adherence, and member satisfaction. The scores from these areas combine to create an overall Star Rating, which influences plan incentives and competitive positioning in the market.
Understanding these criteria highlights the critical role of performance in maintaining high-quality outcomes.
Vendor Risk Impact Areas
Given the importance of these criteria, vendor performance plays a pivotal role in meeting CMS standards. Many third-party vendors handle essential functions like data management, patient engagement, care coordination, and medication monitoring - areas that directly affect Star Ratings calculations [9][7][1].
Failures in vendor services can lead to significant risks. For instance, if vendors managing care transitions underperform, hospital readmissions could rise. Similarly, poorly functioning patient engagement platforms can compromise clinical quality reporting. Issues with data accuracy or reliability can further lead to lower Star Ratings, reduced quality bonus payments, and a decline in enrollment [9][8].
While administrative measures were once a primary focus, CMS now places greater emphasis on clinical outcomes. This shift means vendor-related risks increasingly involve technologies for patient engagement, care coordination, and medication management - elements that are critical for achieving strong ratings [4][12].
This dynamic underscores the direct connection between vendor performance and Star Ratings success.
How Vendor Risks Affect CMS Compliance and Star Ratings
Vendors play a crucial role in helping Medicare Advantage plans meet CMS standards. Their performance impacts everything from data security to accurate reporting - both of which are key factors in calculating CMS Star Ratings. When vendors fall short, the consequences can be severe, jeopardizing a plan's competitive edge and financial health.
Data Breaches and Their Impact on Ratings
A vendor data breach doesn't just compromise sensitive information - it also undermines member trust, a vital factor in CMS evaluations. This erosion of trust can lead to lower Star Ratings, directly affecting member satisfaction scores. The financial fallout is steep: Medicare Advantage plans with reduced Star Ratings risk losing hundreds of millions - or even billions - in bonus payments when ratings dip below critical thresholds [8].
The ripple effects of these breaches extend beyond lost revenue, creating broader compliance challenges for plans.
Compliance Risks from Vendor Errors
Vendor errors can also lead to compliance failures. Many vendors handle essential tasks like clinical quality reporting, medication management, and care coordination. If their data is inaccurate, it can disrupt clinical performance measures, dragging down Star Ratings [4][11].
With CMS shifting its focus toward clinical outcomes rather than administrative metrics, dependable vendor performance is more important than ever. Plans must rely on their vendors to deliver accurate and reliable data to maintain high ratings and adapt to evolving quality benchmarks.
Vendor Risk Management Strategies Using Censinet

Unmanaged vendor risks can jeopardize CMS compliance, making effective solutions absolutely necessary. With the challenges tied to vendor performance and regulatory adherence, having a structured approach to risk management is essential - especially for Medicare Advantage plans. This is where Censinet steps in, offering a centralized platform to oversee third-party risks. Its integrated tools simplify vendor assessments and automate the often-complex workflows tied to risk management.
Using Censinet RiskOps for Vendor Assessments

Censinet RiskOps™ simplifies the vendor risk assessment process by providing a centralized platform. It includes a command center that offers clear risk visualization and automates repetitive workflows, reducing manual tasks and ensuring consistency across evaluations.
Accelerating Vendor Evaluations with Censinet AITM
Censinet AITM takes vendor evaluations to the next level by speeding up the process. It allows for instant security questionnaires and automatically summarizes supporting documents, saving time. The platform also captures critical details, such as product integration specifics and fourth-party risk exposures, improving the overall efficiency of assessments. Throughout the process, a human-guided approach ensures that critical decisions are made thoughtfully and effectively.
Automating Risk Workflows for Better Efficiency
Censinet RiskOps enhances efficiency by automating risk workflows. Assessment results and tasks are assigned directly to the appropriate teams, creating a centralized view of vendor policies, risks, and responsibilities. This streamlined system ensures continuous oversight and better coordination across all risk management activities.
sbb-itb-535baee
Measuring Vendor Risk Management ROI on Star Ratings
One way to gauge the return on investment (ROI) of vendor risk management is by tracking improvements in Star Ratings and their financial impact. Building on earlier discussions about compliance and operational risks, let’s explore how effective vendor management can lead to higher Star Ratings and better financial outcomes. Medicare Advantage plans that adopt structured vendor risk strategies often see measurable improvements in performance metrics, which significantly influence their overall ratings. This connection highlights the importance of strong vendor oversight in Centers for Medicare & Medicaid Services (CMS) evaluations.
Before and After Star Ratings Comparison
Looking at Star Ratings before and after implementing vendor oversight can reveal its impact. Enhanced vendor management improves key CMS metrics like member experience, care coordination, and medication adherence. When vendors are effectively monitored and managed, their performance directly boosts these measures [7][4].
Plans can evaluate progress by comparing specific performance metrics before and after adopting comprehensive vendor assessments. For instance, better vendor oversight often leads to reduced hospital readmissions and higher member satisfaction survey scores. These gains contribute to higher Star Ratings, especially when multiple metrics show consistent improvement across rating periods.
Financial Benefits of Higher Star Ratings
Achieving a 4-star rating or higher unlocks major financial benefits, including Quality Bonus Payments (QBPs) and enhanced rebates. Plans with 4 or more stars qualify for these incentives, which directly boost revenue and improve their competitive position. On the other hand, a drop in Star Ratings can result in losses amounting to hundreds of millions of dollars [1][6].
Plans with 5-star ratings gain an additional edge: access to special enrollment periods, which helps them attract more members. Vendor risk management plays a key role in these outcomes by ensuring that third-party services consistently support the clinical outcomes, patient experience, and care coordination measures CMS evaluates. Reliable vendor performance and compliance help plans avoid the disruptions and penalties that can lower ratings and jeopardize financial stability.
Conclusion
Vendor risk management plays a critical role in achieving higher CMS Star Ratings and improving financial outcomes. For Medicare Advantage plans that depend on third-party vendors - whether for clinical resources, analytics platforms, or medication therapy management programs - it's essential to ensure these vendors deliver on key CMS quality measures. When vendors fall short, it directly impacts quality measures that are vital for CMS ratings.
Minimizing vendor-related failures is a key step toward securing high Star Ratings, which come with substantial financial rewards [1]. As CMS continues to emphasize clinical care, health outcomes, and patient experience - while simplifying administrative requirements - the reliability and performance of your vendor network become increasingly important [2][3][4][5]. Strong vendor management is essential to mitigating risks that could negatively affect the quality measures tied to Star Ratings.
Censinet RiskOps and Censinet AI streamline third-party risk assessments by automating processes like security questionnaires, evidence summaries, and detailed risk reporting. This approach combines automation with human oversight, enabling risk teams to reduce vulnerabilities effectively while maintaining control and decision-making authority.
FAQs
How do CMS Star Ratings affect the revenue of Medicare Advantage plans?
CMS Star Ratings significantly influence the financial outcomes of Medicare Advantage plans. Plans that achieve 4 stars or higher become eligible for quality bonus payments and rebates, potentially boosting revenue by as much as 5%. Conversely, plans with lower ratings may face reduced payments, which could lead to cost-cutting measures like scaling back benefits or increasing premiums for members.
Focusing on vendor risk management and compliance can help healthcare organizations enhance their Star Ratings. This not only supports stronger financial performance but also ensures beneficiaries receive higher-quality care.
How do third-party vendors impact CMS Star Ratings for Medicare Advantage plans?
Third-party vendors play a key role in shaping CMS Star Ratings by assisting Medicare Advantage plans in meeting compliance standards, bolstering cybersecurity measures, and enhancing quality metrics. These partners ensure precise data reporting and provide support for clinical and operational processes that align with CMS guidelines.
When healthcare organizations manage vendor risks effectively, they can reduce compliance and security challenges, which ultimately leads to improved outcomes and higher Star Ratings. Collaborating with dependable vendors is crucial for maintaining smooth operations and delivering high-quality care to members.
What steps can Medicare Advantage plans take to effectively manage vendor risks?
Medicare Advantage plans can tackle vendor risks effectively by taking a thoughtful and proactive approach. Start with detailed risk assessments during the onboarding process to pinpoint potential issues and confirm that vendors meet compliance standards.
Set up clear policies and procedures to manage vendor relationships and schedule regular audits to ensure ongoing compliance. Leveraging data analytics for tasks like coding and documentation can also highlight weak spots and improve precision. By maintaining consistent oversight and staying ahead of potential problems, organizations can safeguard sensitive data, minimize risks, and even boost their CMS Star Ratings.


