Healthcare Vendor Risk Management Budget Planning: ROI and Resource Allocation
Post Summary
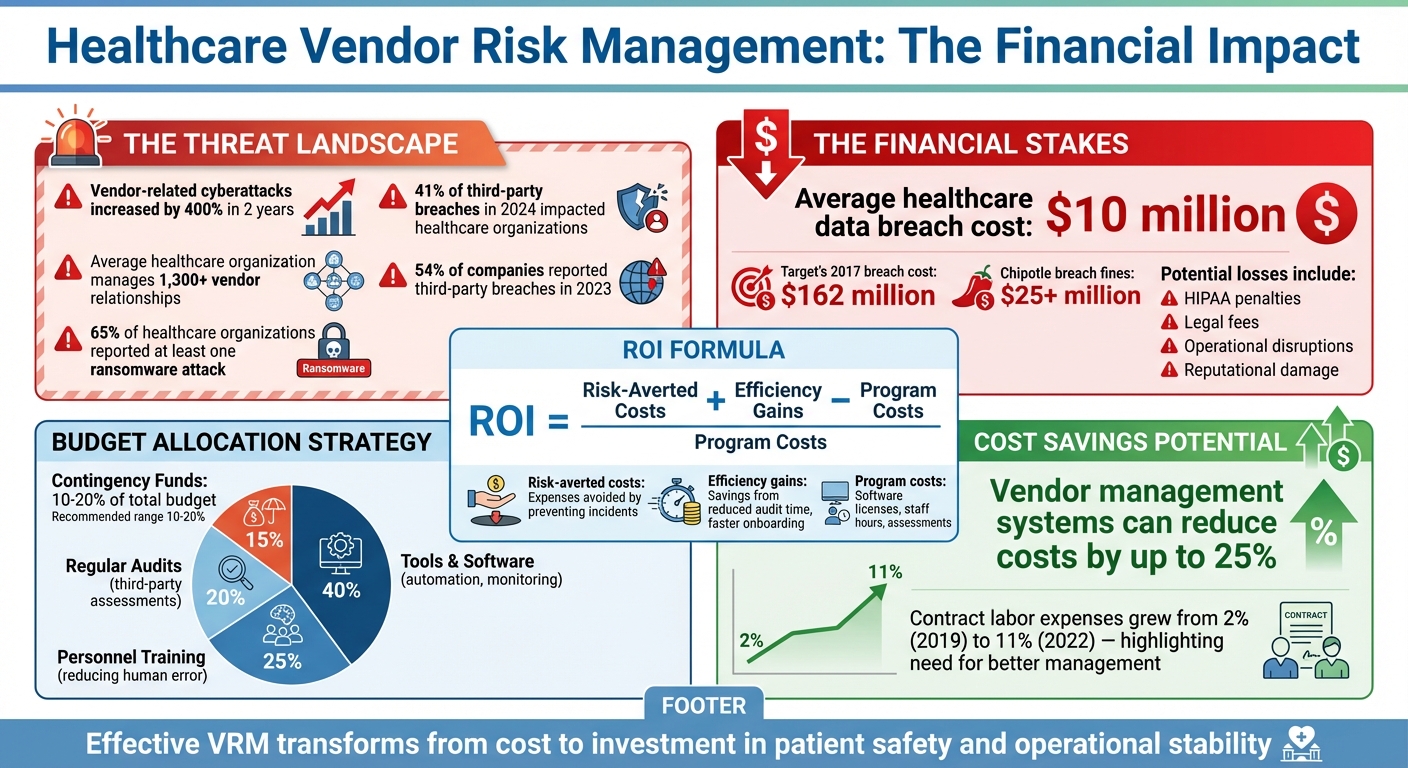
Healthcare organizations face mounting risks from vendor-related cyberattacks, with breaches in the sector increasing by over 400% in two years. Managing over 1,300 vendor relationships, each a potential vulnerability, is a critical challenge. The financial stakes are high, with the average healthcare data breach costing nearly $10 million and leading to legal penalties, service disruptions, and reputational harm. Effective vendor risk management (VRM) can mitigate these risks, but it requires careful budget planning.
Here’s what you need to focus on:
- Assess Risks and Costs: Identify high-risk vendors, calculate potential financial impacts, and review current spending on risk management.
- Calculate ROI: Use a formula to measure cost savings from risk reduction and efficiency improvements compared to program costs.
- Allocate Resources Wisely: Prioritize spending on tools, training, audits, and contingency funds for unexpected challenges.
- Choose the Right Tools: Solutions like Censinet RiskOps™ streamline assessments and monitoring, helping manage large vendor portfolios efficiently.
- Track and Optimize: Regularly monitor spending, vendor performance, and ROI to adjust your budget as risks evolve.
With the right approach, VRM transforms from a cost to an investment in protecting patient data, ensuring compliance, and maintaining operational stability.
Healthcare Vendor Risk Management: Key Statistics and Budget Allocation Guide
Assess Current Vendor Risks and Costs
Before diving into budget planning, it's crucial to identify vendor risks and understand their financial implications. Start by cataloging all vendor relationships, evaluating potential financial exposure, and reviewing your current spending on risk management. Defining risk tiers can also help you grasp each vendor's potential impact more clearly.
Create a Vendor Inventory and Risk Profile
Begin by listing all third-party relationships in a detailed inventory. In healthcare, vendor risk management covers a wide range of partnerships, including software providers, IT services, staffing agencies, and medical device suppliers [1]. Be sure to evaluate each vendor throughout their entire lifecycle [1].
Once your inventory is complete, categorize vendors into risk tiers. These tiers should reflect factors like the financial impact of a potential breach and how critical the vendor is to your operations [1]. For instance, vendors with access to sensitive data like protected health information (PHI) or those supporting essential patient care systems should fall into high or critical-risk categories. On the other hand, vendors with minimal system access might be classified as low risk.
Calculate Financial Impact of Vendor Risks
The financial fallout from vendor-related incidents often goes far beyond the immediate costs of a data breach. In healthcare, the average cost of a data breach is close to $10 million [1], which underscores the importance of a thorough risk cost assessment. Beyond breach expenses, organizations may face HIPAA penalties, operational disruptions, and long-term reputational damage [1][2].
These costs can also include class action lawsuits, government fines, and penalties under laws like the False Claims Act [1]. Poor vendor cybersecurity can lead to legal liabilities and steep operational expenses [1]. With more than 65% of healthcare organizations reporting at least one ransomware attack, these risks are anything but theoretical [1].
Review Current Risk Management Spending
Take a close look at your current risk management spending to pinpoint any gaps. Are resources being allocated effectively? For example, higher-risk vendors should receive more oversight and investment. Neglecting vendor security qualifications can lead to costly outcomes, including lawsuits, fines, and reputational harm, which can easily outweigh any initial savings [1].
Break down your spending across areas like vendor assessments, monitoring tools, audits, and incident response. This will help you establish a baseline for future investments and set the stage for calculating the return on investment (ROI) in vendor risk management. By understanding where your money is going, you can better prioritize and protect your organization.
Calculate ROI for Vendor Risk Management
Grasping the return on investment (ROI) for vendor risk management is essential when defending its place in your budget. By evaluating identified vendor risks, you can quantify the financial benefits of preventative measures. Unlike traditional ROI, which focuses on profit, vendor risk management ROI emphasizes cost savings and loss prevention. Essentially, the value lies in avoiding breaches, steering clear of fines, and ensuring smooth operations [6]. Here's how you can break down and calculate ROI using actionable steps and comparisons.
Apply the ROI Formula
The formula is straightforward:
(Risk-Averted Costs + Efficiency Gains - Program Costs) / Program Costs [6].
- Risk-averted costs refer to expenses avoided by preventing incidents.
- Efficiency gains include savings from reduced audit time, faster vendor onboarding, and fewer manual assessments.
- Program costs cover investments such as software licenses, staff hours, and third-party assessments.
Even modest reductions in the likelihood of incidents, combined with improved efficiency, can result in a strong ROI for your vendor risk management (VRM) program.
Perform Cost-Benefit Analysis
A cost-benefit analysis helps you weigh VRM expenses against potential savings. Start by documenting your current workflows and costs to establish a baseline [4]. Factor in:
- Tangible costs like breach remediation, HIPAA fines, and legal fees.
- Intangible benefits like improved compliance and enhanced security [6].
Use a full year of incident or claims data to eliminate seasonal fluctuations and account for demographic or regional changes [5]. Beyond financial metrics, consider other benefits, such as better patient satisfaction or reduced staff turnover. Evaluate ROI over both short-term (1–2 years) and long-term (3–5 years) horizons [4]. Benchmarking your results against industry standards can validate your analysis and help prioritize resources effectively.
Use Healthcare ROI Benchmarks
Healthcare organizations often compare their supply chain and vendor performance with industry peers [7]. Assigning a dollar value to potential loss events - known as financial quantification of risk - can guide monitoring strategies and assess ROI [7]. For instance, adopting frameworks like NIST CSF 2.0 as a cybersecurity standard has been linked to reduced year-over-year increases in cybersecurity insurance premiums [8], offering a clear ROI indicator.
Consider the 2024 ransomware attack on Change Healthcare, which exposed the potential for billions in emergency fund losses, revenue hits, and significant data breaches [7]. When calculating ROI, remember that your VRM program's benefits extend beyond your organization - it also supports the broader healthcare ecosystem by safeguarding critical operations and data.
Allocate Budget Across Key Categories
Allocating your vendor risk management budget wisely transforms it from a simple expense into a powerful investment in protection. By focusing your budget on clearly identified risk areas, you not only control costs but also strengthen your organization’s cybersecurity defenses. Think of it as a continuous, collaborative effort across departments to tackle key threats and maintain operational stability [9].
Distribute Resources by Category
A smart approach to budgeting involves breaking it down into key areas: upgrading tools and software, enhancing personnel skills through training, conducting regular audits, and setting aside a reserve for unexpected challenges. For example, automation tools for vendor assessments should be a top priority - they save time and improve accuracy. Similarly, investing in compliance and incident response teams and funding third-party audits are essential. With over 30% of data breaches tied to third-party incidents [11], thorough vendor evaluations are not just helpful - they’re critical.
Once resources are distributed, focus on channeling funds into areas that offer the greatest reduction in risk.
Invest in High-Impact Areas
Your resources should reflect the risk levels of your vendors. High-risk vendors - especially those with access to sensitive systems or patient data - demand more frequent reviews and robust assessments [18, 19]. Automated tools like Censinet RiskOps™ can make a big difference here, offering continuous monitoring, quicker assessments, and early detection of vulnerabilities before they become costly breaches.
Don’t overlook the human factor. Training your staff is just as critical, as human error is a major weak point in cybersecurity. High-profile incidents like Target’s 2017 breach, which cost over $162 million, or Chipotle’s crisis with fines exceeding $25 million [11], highlight the importance of proactive measures such as employee training and automated monitoring systems.
Set Aside Contingency Funds
Reserving a portion of your budget - typically 10–20% - for unforeseen risks is a smart move [10]. These contingency funds can cover unexpected expenses like rush fees, compliance penalties, legal consultations, or remediation efforts. With 54% of companies reporting third-party breaches in 2023 [11], having a financial safety net is essential for quick responses and maintaining business continuity.
The exact amount you reserve should reflect your organization’s risk profile. For instance, companies handling sensitive data or relying heavily on high-risk vendors may need to allocate toward the higher end of this range. Think of it as an insurance policy - small upfront costs that can prevent much larger expenses down the line.
sbb-itb-535baee
Choose the Right Censinet Plan
When managing budgets and aiming for a solid return on investment, picking the right risk management plan is crucial. Your choice should align with your organization's specific needs for support and control. Censinet offers three tailored options: Platform, Hybrid Mix, and Managed Services. Each plan is designed to accommodate different organizational structures, resources, and risk management priorities.
Review Censinet Plans and Features
To make an informed decision, it’s important to understand what each plan provides. Here’s a breakdown:
- The Platform plan gives your team complete access to the Censinet RiskOps™ software, equipping them to independently manage risk assessments and monitoring. This option is ideal if you already have a skilled internal team in place.
- The Hybrid Mix combines in-house tools with expert support, offering flexibility for organizations that need targeted assistance while retaining overall control.
- Managed Services takes care of everything for you. From assessments to reporting and ongoing monitoring, this fully outsourced option is perfect for teams with limited resources or those seeking a hands-off approach.
| Plan | Best For | Key Features | Management Style |
|---|---|---|---|
| Platform | Teams with strong internal resources | Full Censinet RiskOps™ access, risk assessments, cybersecurity tools, Censinet AI™ | Self-managed |
| Hybrid Mix | Teams needing partial support | Combination of software and managed services, including Censinet AI™ | Shared responsibility |
| Managed Services | Teams with limited resources | End-to-end risk management, including assessments, reporting, and monitoring | Fully outsourced |
All plans come with Censinet AI™, which speeds up assessments, summarizes documentation automatically, and generates risk summary reports.
By comparing these features, you can determine which plan aligns best with your organization’s needs and capabilities.
Select a Plan Based on Your Needs
Once you’ve reviewed the options, match the plan to your team’s strengths and your risk management goals. For organizations with experienced cybersecurity teams, the Platform plan offers the tools needed to maximize productivity and efficiency. On the other hand, if your resources are limited, Managed Services provides a complete solution, allowing your team to focus on broader strategies while Censinet handles the heavy lifting.
The Hybrid Mix is a great middle ground for organizations in transition. If you’re building internal expertise but still need occasional expert assistance - perhaps during busy assessment periods or when handling high-risk vendors - this plan offers the perfect blend of control and support.
As highlighted by the Ponemon Research Report, "current approaches to assessing and managing vendor risks are failing", leading to increased fines and investigations by HHS and OCR [12]. This underscores the importance of choosing a plan that strengthens your risk management processes.
When deciding, consider factors like the size of your vendor portfolio, your team’s capacity, and compliance requirements. Organizations with smaller teams often see better returns with Managed Services, while those with established internal expertise can benefit from the cost-effectiveness and autonomy of the Platform plan.
Track and Optimize Your Budget
Once you've chosen a plan and allocated resources, the next step is keeping a close eye on your budget. Regular monitoring ensures that every dollar works as hard as it can, preventing unnecessary spending and uncovering opportunities for improvement. This ongoing attention builds on your initial efforts, helping you achieve lasting results.
Monitor Spending and Performance
Keeping tabs on spending and performance in real-time is essential for effective vendor risk management. Real-time dashboards are a powerful tool for this, offering a clear view of spending trends, vendor performance, and risk outcomes. They allow you to spot issues immediately and address them before they escalate.
Your dashboard should include not just financial data but also key metrics like vendor compliance rates, assessment completion times, and trends in security incidents. For instance, if a vendor repeatedly misses compliance deadlines, you can intervene promptly to avoid costly surprises during audits.
Consider this: hospitals that use vendor management systems can cut management costs by up to 25% [13]. To achieve similar results, implement a vendor scoring system tied to performance metrics outlined in your Service Level Agreements (SLAs). Track indicators like system uptime for SaaS vendors, response times for IT services, and HIPAA compliance rates from regular audits. These metrics provide a clear picture of whether your vendors are delivering on their promises.
Review Budget Performance Regularly
Make it a habit to review your budget on a regular basis. Schedule quarterly check-ins and a detailed annual review. These reviews should compare actual spending with your projections and evaluate whether your current resource allocation aligns with the shifting risk landscape.
Vendor portfolios evolve over time as new vendors come on board and risk profiles change. If you find unused contingency funds, think about reallocating them to areas that could have a bigger impact, such as advanced AI tools that speed up assessment processes.
Here's a striking example: contract labor expenses for healthcare organizations jumped from 2% of total labor costs in 2019 to 11% in 2022 [13]. This kind of shift highlights why routine budget reviews are so important. They ensure your resources are being used effectively and are aligned with both current needs and potential risks. These reviews also help you fine-tune your overall vendor risk management strategy.
Maintain Long-Term ROI
To ensure a strong return on investment (ROI) over the long term, consider automating repetitive tasks like contract management, ongoing monitoring, and tracking critical dates. Automation not only saves time but also reduces the chances of missing important deadlines [14]. This frees your team to focus on more strategic aspects of risk management.
Automation tools like Censinet AI™ can significantly enhance efficiency. By speeding up vendor questionnaires, summarizing documentation, and generating risk summary reports, these tools let you evaluate more vendors in less time. This means you can expand your risk coverage without a corresponding increase in costs.
To measure the impact of these improvements, track metrics like time saved through automation, the financial benefits of avoiding data breaches (the average cost of a healthcare data breach is nearly $10 million [1]), and productivity gains from streamlined processes. These numbers not only help justify your budget to senior leadership but also highlight the ongoing value of your vendor risk management efforts.
Conclusion
Creating a vendor risk management budget isn’t just about allocating funds - it’s about protecting patient safety and shielding your organization from ever-changing threats. With vendor-related attacks in healthcare skyrocketing by over 400% in just two years [1] and 41% of third-party breaches in 2024 impacting healthcare organizations [3], a proactive stance is no longer optional - it’s critical.
The process is simple yet powerful: evaluate your current vendor risks and associated costs, calculate ROI using actual financial data, and focus investments on areas with the greatest impact. Considering the nearly $10 million average cost of a breach [1], the math is clear. Every dollar spent on prevention can save exponentially more by avoiding breach-related expenses, regulatory fines, and damage to your reputation. To achieve this, the right tools make all the difference.
Solutions like Censinet RiskOps™ and AI™ simplify risk management, helping you efficiently oversee more than 1,300 vendor relationships while cutting down on administrative burdens.
Sustained success, however, depends on constant vigilance. Regularly monitoring metrics, automating repetitive tasks, and revisiting your budget as your vendor landscape evolves will help you stay ahead of emerging threats. By integrating these practices into your larger cybersecurity strategy, you’ll not only protect your operations but also ensure the safety of the patients who rely on you.
FAQs
What’s the best way for healthcare organizations to identify and manage high-risk vendors?
Healthcare organizations can stay on top of managing high-risk vendors by starting with a clear identification process. Pinpoint vendors who handle sensitive information, like Protected Health Information (PHI), or those whose services are critical to daily operations. Once identified, conduct thorough risk assessments to dig into their cybersecurity measures and identify any weak spots.
It’s smart to channel resources toward vendors that pose the biggest risks to patient safety or the organization’s core functions. Set up continuous monitoring systems to ensure these vendors stick to security standards, and make sure specific cybersecurity requirements are spelled out in all vendor contracts to hold them accountable. Also, don’t let your risk management approach get stale - regularly review and adjust strategies to stay ahead of emerging threats and make the best use of available resources.
What factors should healthcare organizations consider when calculating ROI for vendor risk management?
When you're working out the ROI for vendor risk management, it's essential to weigh both costs and benefits. On the cost side, think about expenses like conducting vendor assessments, responding to breaches, the financial hit from downtime, compliance-related efforts, and the labor or resources needed for each assessment.
On the flip side, the benefits often come in the form of risk reduction. This includes avoiding cybersecurity incidents, boosting operational efficiency, and staying on top of regulatory requirements. By carefully balancing these expenses against the potential gains, healthcare organizations can make smarter choices about where to allocate resources and show the true value of their vendor risk management programs.
How can contingency funds be effectively allocated within a vendor risk management budget?
Allocating 10–15% of your total vendor risk management budget as contingency funds is a practical way to handle unexpected costs. These funds can be a safety net for unforeseen expenses, such as integration hiccups, data migration challenges, or sudden compliance updates.
By planning ahead and setting aside these funds, healthcare organizations can reduce the risk of financial strain and keep their vendor risk management strategies on track. This proactive step adds flexibility to your budget, helping to manage surprises effectively and ensuring a smoother overall process.


