HIPAA Compliance Audits in Risk Management Frameworks
Post Summary
HIPAA compliance audits are not just about meeting regulations - they can be a powerful part of your risk management strategy. Instead of treating these audits as a checklist, healthcare organizations can use them to identify vulnerabilities, strengthen data security, and improve operational efficiency. Here's what you need to know:
- What They Are: HIPAA audits evaluate compliance with rules to protect electronic protected health information (ePHI). Types include remote OCR desk audits, internal audits, and third-party assessments.
- Why They Matter: Integrating audits into risk management helps organizations address cybersecurity threats, reduce breaches, and streamline compliance efforts.
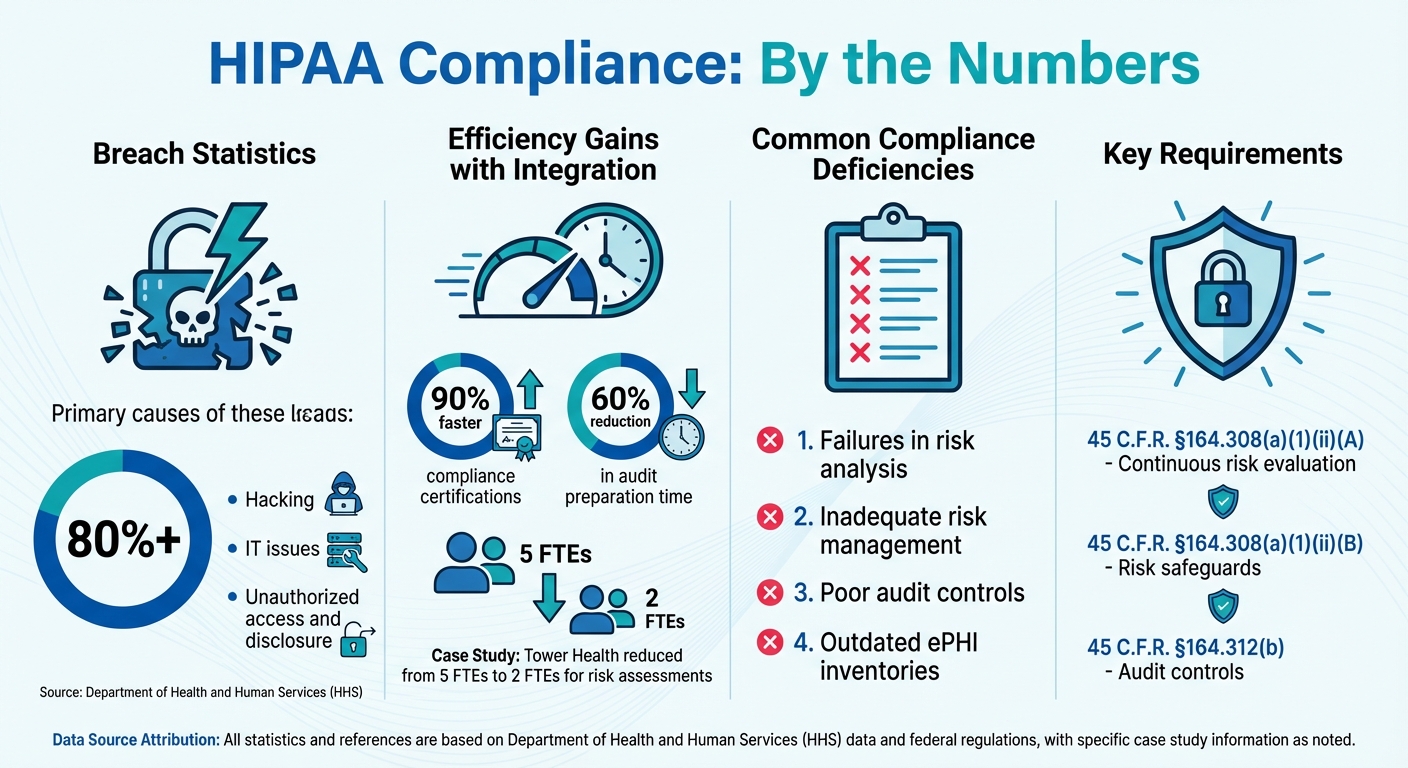
- Key Challenges: Common issues include outdated ePHI inventories, poor audit controls, and lack of coordination across departments.
- How to Succeed: Focus on clear governance, risk analysis, and continuous monitoring. Use tools designed for healthcare to simplify processes and improve outcomes.
Research Findings: HIPAA Audits and Risk Management
HIPAA Compliance Audit Statistics and Impact on Healthcare Organizations
Federal and Regulatory Requirements
The HIPAA Security Rule requires that risk analysis and management be treated as ongoing responsibilities, not just one-time compliance tasks. Specifically, under 45 C.F.R. §164.308(a)(1)(ii)(A) and (ii)(B), covered entities must continuously evaluate risks to electronic protected health information (ePHI) and implement safeguards to minimize those risks. Additionally, §164.312(b) mandates audit controls to track and review system activity involving ePHI. These rules apply to all systems handling ePHI, including mobile devices, cloud platforms, and applications beyond traditional electronic health records.
Guidance from NIST Special Publications 800-30 and 800-66 provides actionable frameworks for meeting these requirements. These frameworks include tools like risk matrices, registers, and prioritization strategies to help organizations formalize their risk management processes [2][5]. Together, these regulations and guidelines emphasize the importance of integrating risk management into daily operations.
Industry Research and Data
Data from enforcement actions paints a clear picture of the risks associated with poor compliance. Over 80% of large HIPAA breaches reported to the Department of Health and Human Services (HHS) involve hacking, IT issues, or unauthorized access and disclosure [2]. Further analysis of OCR enforcement actions highlights that failures in risk analysis and management are among the most commonly cited deficiencies under the HIPAA Security Rule.
Organizations that adopt structured and repeatable HIPAA risk assessments tend to fare better. Research from security vendors and advisory firms shows that these organizations detect and contain security incidents more quickly and at lower costs. This success is often attributed to having clear asset inventories, well-defined controls, and documented response plans [4][6]. By treating risk management as a continuous process, these organizations are better equipped to minimize disruptions and financial losses.
Common Compliance Challenges
Healthcare organizations face several hurdles when it comes to HIPAA audits. One major challenge is maintaining an up-to-date inventory of PHI. Many organizations struggle to keep track of where ePHI is stored, especially as technology ecosystems grow to include third-party vendors and cloud services. Another significant issue is inadequate audit controls - many organizations fail to log access, modifications, or transmissions effectively, making it harder to detect and investigate security incidents [2][7].
Coordination across departments is another sticking point. IT, compliance, legal, and clinical teams often operate in silos, using different tools and documentation methods. This lack of integration can slow down responses and create gaps in compliance. As Matt Christensen, Sr. Director of GRC at Intermountain Health, explains:
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare" [1].
This complexity highlights the need for solutions tailored to healthcare's unique challenges. From managing patient data platforms and medical devices to navigating research systems and vendor networks, healthcare organizations require tools designed specifically for their intricate risk environments. These challenges set the stage for the next section, which focuses on practical strategies for streamlining integration.
How to Integrate HIPAA Audits into Risk Management
Setting Up Governance and Scope
Establishing clear roles and responsibilities within your organization is critical. Assign specific teams - such as IT, compliance, legal, and clinical departments - to oversee various aspects of HIPAA-related risks. Start by creating a comprehensive inventory of all assets that handle electronic protected health information (ePHI). These assets might include electronic health record systems, patient portals, medical devices, cloud platforms, research databases, and third-party vendors. This inventory serves as the backbone of your risk management strategy.
Healthcare organizations often operate in complex environments, which demand tools tailored to their unique needs. James Case, VP & CISO at Baptist Health, highlighted the value of purpose-built platforms:
"Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with" [1].
Adopting integrated systems ensures real-time, accurate tracking of ePHI assets. Once governance is in place, the focus shifts to continuous risk evaluation and mapping controls.
Analyzing Risks and Mapping Controls
A systematic approach to risk evaluation is essential. Assess each asset in your inventory, assign risk scores based on the likelihood and impact of threats, and align HIPAA controls with your enterprise risk management framework. This approach minimizes redundancy and ensures a streamlined process. Prioritize critical areas such as access management, encryption, and audit logging [8][5][9].
Terry Grogan, CISO at Tower Health, shared how automation improved efficiency:
"Censinet RiskOps allowed 3 FTEs to go back to their real jobs! Now we do a lot more risk assessments with only 2 FTEs required" [1].
AI-powered platforms can automate tasks like questionnaires and evidence validation, speeding up risk assessments. This efficiency enables your team to evaluate more vendors and systems within a shorter time frame. The next step is implementing continuous monitoring to convert audit findings into actionable security improvements.
Monitoring and Using Audit Results
Continuous monitoring is essential for identifying security incidents, compliance gaps, and unusual access patterns in real-time. Automated platforms with dashboards make it easier to visualize prioritized risks and track remediation efforts [8][5][9].
Regularly update your risk assessments - not just annually, but whenever major changes occur, such as onboarding new vendors, system upgrades, security incidents, or regulatory updates. Use audit findings to guide resource allocation and strategic planning. Brian Sterud, CIO at Faith Regional Health, emphasized the importance of benchmarking:
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters" [1].
sbb-itb-535baee
Results of Integrated HIPAA Audits
Fewer Breaches and Reduced Impact
Integrating HIPAA audits into a healthcare organization's risk management framework creates a proactive shield against data breaches. With continuous monitoring, teams can identify and address vulnerabilities before they turn into actual threats. According to HHS guidance, risk analysis remains a cornerstone of effective HIPAA compliance [2]. By keeping detailed asset inventories and routinely testing security measures, organizations can respond swiftly to incidents, minimizing their overall impact. This proactive approach not only bolsters security but also results in financial and operational efficiencies.
Cost Savings and Efficiency Gains
The financial perks of integrating HIPAA audits are hard to ignore. Using pre-built mappings between frameworks like HIPAA, HITRUST, and SOC 2, healthcare organizations can streamline their compliance processes. These mappings allow control test results to be applied across multiple standards, saving significant time and effort [3]. Data shows that organizations leveraging integrated risk management platforms achieve compliance certifications up to 90% faster and cut audit preparation time by about 60% [8]. Automation further reduces manual tasks, enabling staff to focus on more strategic priorities. Beyond just saving money, these integrations strengthen the organization’s overall cybersecurity defenses.
Higher Program Maturity Levels
Integrated HIPAA audits do more than mitigate risks - they push organizations toward higher levels of program maturity. By standardizing processes based on incident records, executive certifications [4], and industry benchmarks, organizations can make measurable improvements. This data-driven strategy equips security leaders with the tools to advocate for necessary resources and clearly demonstrate progress to executives and boards. Platforms like Censinet RiskOps™ offer real-time benchmarking and insights, promoting proactive risk management and driving program growth to new heights.
Conclusion
Building a strong HIPAA audit framework requires combining the strategies and research outlined earlier into actionable steps.
Implementation Steps
Start by establishing a unified HIPAA audit and risk management program. This means setting up clear governance with defined roles across IT, compliance, clinical, and legal teams. Create a detailed inventory of all systems handling protected health information (PHI), such as electronic health records, backups, and third-party applications. Develop a repeatable audit plan that uses a likelihood-and-impact matrix to prioritize risks, ensuring critical areas get the attention they need. Incorporate continuous monitoring with real-time alerts and periodic reviews to identify and address vulnerabilities early. Invest in technology that centralizes compliance efforts - tools with features like centralized control libraries, configurable risk workflows, automated evidence collection, and vendor risk management with BAA tracking can be game-changers.
Specialized platforms can make this process even more efficient.
Technology Support for Integration
Platforms designed specifically for risk management make it easier to integrate HIPAA audits into broader compliance efforts. For example, Censinet RiskOps™ offers a centralized solution to manage risks across vendors, patient data, medical devices, and supply chains. According to industry leaders, Censinet RiskOps™ simplifies risk assessments and replaces time-consuming manual tasks, improving overall efficiency. These platforms provide dashboards that highlight residual risks, system health, and audit readiness, along with exportable reports tailored to meet OCR standards. This allows healthcare leaders to respond quickly to regulators, payers, and partners.
Main Points to Remember
Integrating HIPAA audits with risk management is a smart way to protect patient data in an increasingly complex threat landscape. This approach leads to fewer breaches, cost savings, and stronger compliance programs. As Brian Sterud, CIO at Faith Regional Health, explained:
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." [1]
Adopting proactive, data-driven strategies is essential for healthcare organizations to align security and compliance effectively.
FAQs
How do HIPAA audits strengthen risk management in healthcare organizations?
HIPAA audits are a key component of any healthcare organization's risk management approach. These audits help pinpoint weaknesses and confirm adherence to regulatory requirements, allowing organizations to tackle risks head-on and strengthen their data protection efforts.
Beyond identifying gaps, audits offer critical guidance on where to allocate resources for security improvements. This can minimize the likelihood of data breaches, hefty penalties, and harm to the organization's reputation. Regularly conducting these audits as part of a broader risk management strategy not only safeguards patient information but also bolsters the organization's ability to maintain stable and secure operations over time.
What challenges do organizations commonly face during HIPAA compliance audits?
When tackling HIPAA compliance audits, organizations often face a few recurring hurdles. One of the biggest issues is dealing with incomplete or outdated documentation. Without proper records, proving compliance becomes a daunting task.
Another challenge is insufficient staff training. If employees don’t fully understand their HIPAA responsibilities, they may unintentionally put the organization at risk.
On top of that, many organizations struggle with conducting thorough risk assessments. Keeping security measures current and effectively addressing third-party risks can also be tricky. These obstacles not only make compliance audits more challenging but can also jeopardize the security of sensitive patient data.
How can integrating HIPAA audits into risk management frameworks save costs and improve efficiency?
Integrating HIPAA audits into risk management frameworks can be a game-changer for healthcare organizations. By streamlining efforts, these audits help cut down on redundant processes and catch vulnerabilities early. This proactive approach not only helps avoid expensive data breaches or compliance fines but also ensures smoother operations.
Another major advantage is improved efficiency. Automating compliance tasks reduces the need for manual labor and provides real-time insights. This means organizations can better allocate their resources, focus on high-priority risks, and respond swiftly to potential threats - all while keeping patient data secure and protected.


