ICU and Critical Care Vendor Risk Management: Life Support System Reliability
Post Summary
Managing vendor risks in ICUs is a life-or-death matter. Cyberattacks on vendors have surged 400%, and healthcare breaches cost an average of $9.42 million. With over 1,300 vendors involved, outdated risk management methods - like annual assessments - leave systems exposed for months.
Key Takeaways:
- Manual processes assess only 20% of vendors and miss real-time risks.
- Life support systems depend on continuous, reliable vendor oversight.
- Automated platforms like Censinet RiskOps™ provide real-time monitoring, instant alerts, and faster incident response.
Manual methods are slow, inconsistent, and leave critical gaps. Automation ensures ICU systems stay secure and functional, protecting both patients and healthcare providers.
1. Censinet RiskOps™
Censinet RiskOps™ transforms how healthcare organizations manage vendor risks by providing continuous, automated monitoring. Acting as a centralized hub, it evaluates vendor risks in real time, eliminating the delays tied to traditional methods. Plus, it sends instant alerts whenever a vendor’s conditions change.
The platform speeds up evaluations with automated workflows that simplify security questionnaires and quickly summarize vendor evidence. With the help of Censinet AI™, vendors can complete questionnaires in mere seconds, while the system automatically generates risk summary reports using relevant assessment data.
Unlike annual assessments that can quickly become outdated, RiskOps keeps tabs on vendor security postures as they evolve. If a vendor encounters a security breach or fails to meet compliance standards, the system immediately notifies risk teams, ensuring no time is wasted.
RiskOps also enhances incident response through its command center, which organizes all risk data into a real-time, easy-to-read dashboard. This allows healthcare leaders to quickly spot high-risk vendors and direct critical findings to the right people for action. By coordinating efforts across Governance, Risk, and Compliance teams, RiskOps ensures that response protocols kick into gear seamlessly - avoiding the bottlenecks of manual processes.
The platform blends automation with expert oversight through a human-in-the-loop approach. Risk teams can customize rules to maintain control, ensuring decisions reflect the unique challenges of healthcare risks.
Next, we’ll dive into how these automated features stack up against the traditional, manual methods of managing vendor risk.
2. Manual Vendor Risk Management Methods
Manual vendor risk management relies on tools like spreadsheets, email, and periodic reviews to monitor vendor compliance and security for ICU life support systems. Unlike continuous monitoring, these methods fail to capture risks in real time. This delay in identifying potential issues can be especially problematic in critical care settings, where consistent and rapid oversight is essential. As a result, manual processes often lead to significant lags in risk assessment.
Risk Assessment Speed becomes a major hurdle with manual approaches. Teams are tasked with gathering documentation, verifying SOC 2 Type II reports, and ensuring HIPAA compliance - steps that can stretch out over weeks. In situations where a new ventilator system or patient monitoring platform needs to be deployed urgently, these delays can directly impact patient care. Slow assessments not only hinder timely decision-making but also risk compromising the reliability of life support systems. Adding to the challenge, relying on vendor self-attestations provides only a static view of compliance, offering little insight into ongoing security risks.
Clinical Safety Reviews face similar challenges. Without standardized evaluation criteria, manual assessments are inconsistent and prone to inefficiencies. Different team members may evaluate the same vendor in varying ways, leading to overlooked risks. Take the 2016 Banner Health breach as an example: hackers exploited vulnerabilities through a third-party payment processor in a food court, compromising 3.7 million patient records. This incident highlights how superficial, manual assessments can fail to catch critical security flaws [1].
Manual methods also weaken Incident Response capabilities. While nearly all healthcare organizations experience third-party breaches [3], manual processes lack the real-time visibility needed to pinpoint which life support systems might be impacted during an incident. This limitation becomes even more critical when managing single-source suppliers or tracking essential component inventories during emergencies.
The core problem lies in the lack of ongoing vendor evaluation after onboarding. Annual reviews are insufficient in a landscape where vulnerabilities can emerge at any time. Over the course of a year, vendors can experience breaches, lose certifications, or alter their security practices. Without continuous oversight, healthcare organizations are left in the dark, exposing their most critical systems to unseen risks [1].
sbb-itb-535baee
Strengths and Weaknesses
Automated vs Manual Vendor Risk Management in Healthcare ICUs
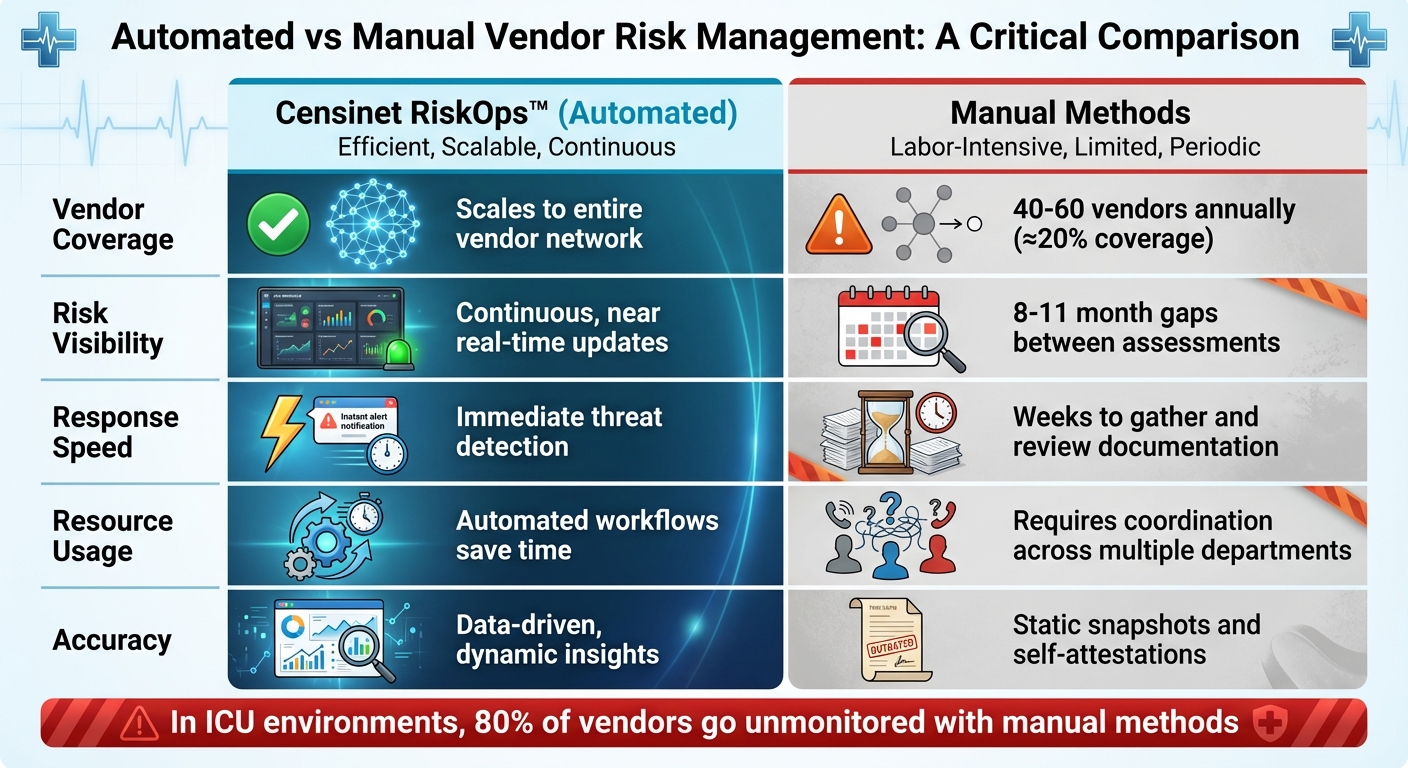
When diving deeper into the feature comparisons, it's clear that manual methods for vendor risk management fall short in several critical areas. For instance, these traditional approaches typically assess only 40 to 60 vendors annually, even though many organizations work with over 300 vendors. This leaves a staggering 80% of vendors unmonitored[2]. Such gaps are particularly risky in environments like ICUs, where life support systems rely on a web of interconnected vendors.
Timing is another major drawback. Annual assessments provide a static snapshot of risks, leaving an 8- to 11-month window for potential vulnerabilities to go unnoticed[2]. On the other hand, Censinet RiskOps™ offers continuous monitoring, delivering near real-time updates on vendor security. This eliminates the long delays inherent in periodic reviews and ensures risks are addressed promptly.
Resource allocation also highlights the inefficiencies of manual methods. Managing vendor risks manually often requires input from multiple departments - Compliance, Finance, Security, IT, Legal, and ESG - which is both time-consuming and cumbersome[5]. While nearly 80% of organizations have formal vendor risk programs, about 30% lack dedicated staff to oversee these efforts[5]. Censinet RiskOps™ simplifies this process by automating workflows and validating evidence, enabling organizations to manage a larger vendor network without needing additional personnel.
| Factor | Censinet RiskOps™ | Manual Methods |
|---|---|---|
| Vendor Coverage | Scales to the entire vendor network | 40–60 vendors annually (≈20% coverage)[2] |
| Risk Visibility | Continuous, near real-time updates | 8–11 month gaps between assessments[2] |
| Response Speed | Immediate threat detection | Weeks to gather and review documentation |
| Resource Usage | Automated workflows save time | Requires coordination across multiple departments[5] |
| Accuracy | Data-driven, dynamic insights | Relies on static snapshots and self-attestations |
In high-stakes environments like ICUs, delays in deploying critical systems can have serious consequences for patient care. By using automated evidence validation, Censinet RiskOps™ eliminates these delays, allowing clinical teams to implement essential technologies swiftly and securely, without sacrificing oversight.
Conclusion
Managing vendor risks manually simply doesn’t meet the demands of modern critical care. Relying on infrequent reviews leaves many vendors unchecked - an unacceptable risk in environments where patient lives depend on interconnected systems and networks. As discussed earlier, manual methods create gaps that automated solutions are designed to close.
Censinet RiskOps™ focuses on the priorities that matter most in ICU settings: fast assessments, patient safety, and the ability to scale effectively. With continuous monitoring, it delivers near real-time threat detection and enables rapid deployment of life-saving technologies, all without sacrificing security.
Healthcare risk managers know that thorough risk analysis is essential for identifying high-priority threats with the most severe consequences[6]. Censinet RiskOps™ provides the precision needed to manage these risks effectively.
Beyond speed and safety, scalability is a game-changer. With evolving threats and increasingly complex ICT supply chains[4], Censinet RiskOps™ uses automated workflows to streamline risk management, reducing the strain on resources.
For organizations tasked with protecting ICU systems, automation isn’t just helpful - it’s essential. The stakes are too high, vendor ecosystems too intricate, and the threat landscape too dynamic to rely on outdated methods. Embracing automated risk management is critical for safeguarding ICU life support systems.
FAQs
How does Censinet RiskOps™ make vendor risk management in ICUs more effective than manual processes?
Censinet RiskOps™ streamlines vendor risk management in ICUs by automating essential processes like continuous monitoring, onboarding, and compliance checks. With integration of industry standards such as HITRUST and HIPAA, it ensures that vital systems adhere to top safety and regulatory benchmarks.
By cutting down on manual tasks and enhancing precision, Censinet RiskOps™ enables healthcare organizations to identify and address risks proactively. This approach helps maintain the dependability of life support systems, protecting both patient health and safety.
Why is continuous monitoring essential for ICU life support systems?
Continuous monitoring plays a crucial role in ICU life support systems, ensuring patient safety by catching potential issues or equipment failures the moment they arise. These systems are responsible for maintaining essential functions like breathing and circulation, where even the smallest glitch can lead to serious outcomes.
With constant oversight, healthcare teams can respond immediately to problems, minimize risks, and keep life-saving equipment functioning reliably. This real-time vigilance is key to providing top-tier care in critical care settings.
What risks are associated with using manual vendor risk assessments in critical care environments?
In critical care settings, relying on manual vendor risk assessments can create several challenges. These include slower identification of vulnerabilities, an increased likelihood of human error, and lapses in continuous monitoring. Such shortcomings can result in overlooked security threats, equipment malfunctions, and potential risks to patient safety.
By automating the vendor risk assessment process, healthcare providers can achieve consistent monitoring and quicker identification of potential problems. This approach helps protect critical care systems and ensures they remain dependable when it matters most.


