Process Revolution: Redesigning Workflows for the AI Era
Post Summary
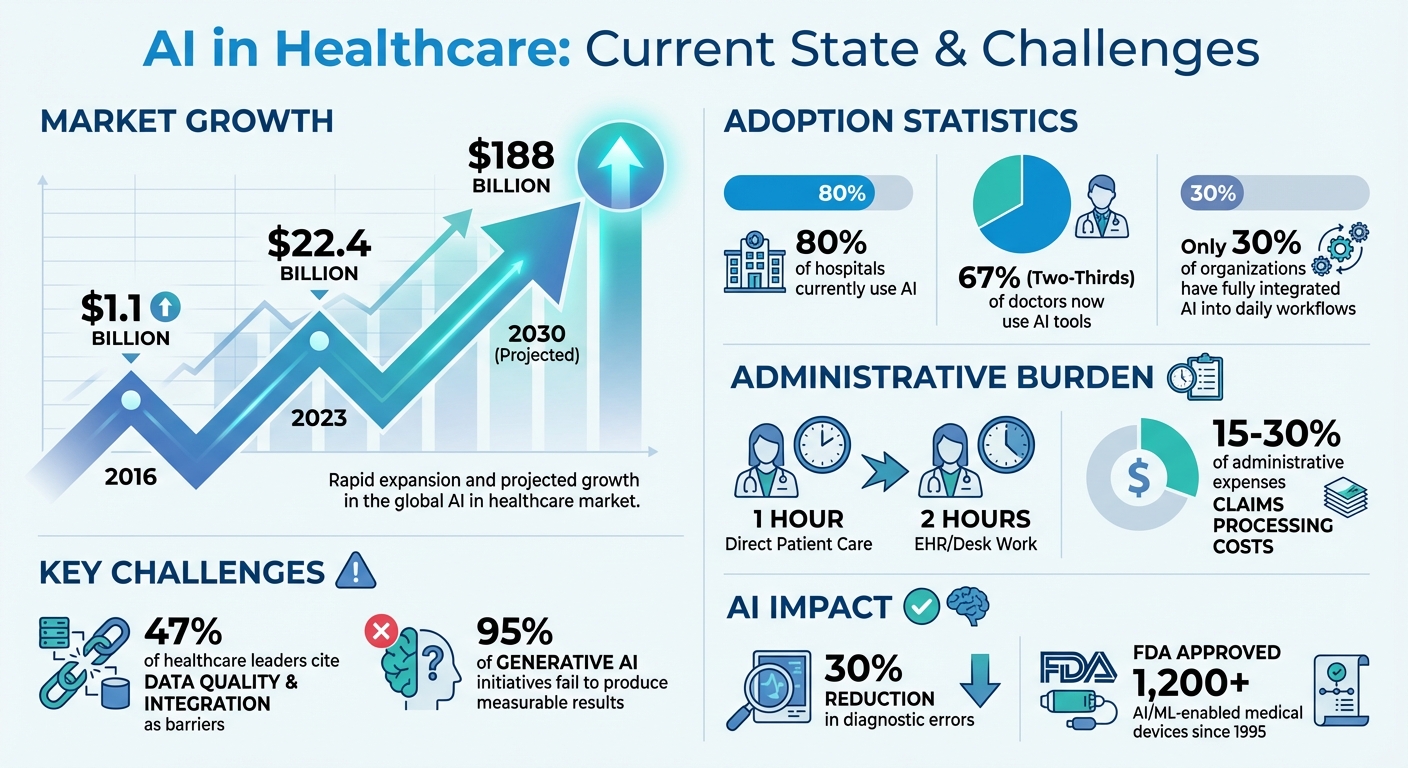
In healthcare, outdated workflows and administrative burdens are slowing progress and causing clinician burnout. AI is changing this by improving diagnostics, automating repetitive tasks, and optimizing operations. However, simply adding AI to existing systems isn’t enough. To fully benefit, healthcare organizations must redesign workflows to address inefficiencies, data silos, and cybersecurity risks.
Key takeaways:
- AI’s Role Today: AI detects diseases earlier, automates scheduling, and handles tasks like claims processing and medical coding.
- Challenges: Data silos, poor interoperability, and cybersecurity risks hinder AI adoption. Only 30% of organizations have fully integrated AI.
- Solutions: Target high-friction tasks, automate admin processes, and use AI for resource allocation and patient flow.
- Cybersecurity: Tools like Censinet RiskOps™ streamline risk assessments, ensuring compliance with regulations like HIPAA.
- Future Trends: Real-time decision-making, integrated ecosystems, and predictive risk management are shaping healthcare workflows.
AI isn’t a quick fix - it requires rethinking processes to improve efficiency, reduce clinician workload, and enhance patient outcomes.
AI in Healthcare: Key Statistics and Adoption Challenges
Challenges in Healthcare Workflow Optimization
Redesigning workflows in healthcare is no small feat, especially when it comes to integrating AI. The process is riddled with challenges that can derail even the most promising initiatives. Only 30% of organizations have fully integrated AI into their daily workflows, highlighting the uphill battle many face [3]. Key obstacles include data silos, cybersecurity vulnerabilities, and ongoing administrative burdens that hinder seamless adoption.
Disconnected Data Systems and Interoperability Issues
Healthcare data is often scattered across isolated and incompatible systems, making it difficult for AI models to access the comprehensive and consistent information they need to perform effectively. Nearly 47% of healthcare leaders cite data quality and integration as significant barriers to AI adoption [4].
Take Radiology, for example. Despite its potential to benefit from AI, the lack of standardized data sharing poses a major hurdle. Elmar Kotter from the Department of Radiology at Medical Center – University of Freiburg points out:
"Another reason why it is difficult to integrate AI algorithms into the radiology workflow is the lack of standards for data sharing between digital systems." [6]
Without proper interoperability, AI tools struggle to integrate seamlessly with Electronic Health Records (EHRs), lab databases, and imaging systems. This disconnect disrupts workflows, increases the cognitive burden on clinicians, and leads to more ignored alerts [3]. Poor integration also diminishes the clinical relevance of AI models, making it nearly impossible to scale their adoption effectively [7]. On top of these data challenges, the introduction of AI brings new cybersecurity risks.
Cybersecurity Risks from AI Systems
AI systems introduce fresh vulnerabilities that healthcare organizations must address. These models, often trained on sensitive patient health information (PHI), imaging data, EHRs, or claims records, pose a significant risk of exposing HIPAA-protected content [9]. Even during the training phase, supposedly secure datasets can become points of vulnerability [9].
Beyond data breaches, AI systems are prone to errors like "hallucinations", where the technology generates incorrect or misleading outputs. Such errors require constant monitoring [8]. Additionally, when data is pooled from multiple institutions - particularly for studying rare diseases - the risk of breaches grows, compounding the already daunting interoperability challenges [5]. These cybersecurity threats not only jeopardize patient safety but also put organizations at risk of non-compliance with regulatory standards.
Administrative Overhead and Workflow Delays
While AI promises to streamline operations, administrative burdens remain a persistent issue. Physicians spend nearly two hours on electronic health record (EHR) and desk work for every hour of direct patient care [10]. Unfortunately, AI adoption has yet to solve this imbalance due to challenges that extend beyond technology.
Outdated infrastructure and fragmented systems slow data flow, while healthcare professionals often resist new tools over concerns about job security, increased workloads, and alert fatigue. Many organizations also lack the internal expertise and clear frameworks needed to implement AI effectively. The sociotechnical effort required for adoption demands significant resources, often leading to delays that undercut AI's potential to improve efficiency. Overcoming these barriers is critical to achieving meaningful workflow optimization through AI.
Strategies for Redesigning Workflows with AI
Integrating AI into healthcare workflows isn't just about adopting the latest technology - it’s about pinpointing where AI can make the biggest impact. The process starts with a thorough needs assessment to identify bottlenecks and areas of administrative overload. By involving clinicians, staff, patients, and caregivers, and combining quantitative data (like time tracking) with qualitative insights (such as staff surveys), healthcare organizations can get a clear view of the challenges they face [11][12]. With this foundation, strategies can be crafted to tackle issues like data silos and administrative delays, focusing on AI-driven solutions that address high-priority tasks.
Targeting High-Friction Tasks
One of the best places to implement AI is in tackling high-friction tasks - those manual, time-consuming processes that often lead to errors and burn out staff. Before jumping into automation, it’s critical to evaluate the task, the available technology, the context, and the people involved. This ensures that AI solutions address real pain points without introducing new problems [11].
A phased approach is often the most effective. Start small with quick-win projects, such as automating appointment reminders or digital patient intake forms. These "sprints" can deliver immediate results and build confidence in the technology. Once the groundwork is laid, organizations can move on to more complex, transformative automation projects - the "marathons" [11][12]. For each initiative, set SMART goals (Specific, Measurable, Achievable, Relevant, and Time-bound) that directly tackle identified issues. For example, aim to "reduce patient wait times by 20%" or "improve billing accuracy to 99%" [12]. This approach ensures measurable progress while addressing operational challenges.
Automating Repetitive Administrative Tasks
AI shines when it comes to automating repetitive, data-heavy administrative tasks. By integrating systems like electronic health records, billing platforms, and scheduling tools, AI can reduce manual work and minimize errors [13]. Tasks like document management, claims processing, appointment scheduling, and routine data entry can be handled efficiently, freeing up staff to focus on patient care. Automation should prioritize improving safety, boosting efficiency, and supporting the delivery of high-quality, equitable care [11].
Optimizing Patient Flow and Resource Allocation
AI can also enhance patient flow and resource allocation by analyzing patterns in patient volume, appointment durations, no-show rates, and overall resource use. These insights allow systems to predict demand and adjust staffing levels accordingly. However, successful implementation requires a solid framework that aligns with strategic goals, ensures robust data infrastructure, complies with regulations like HIPAA, and validates solutions thoroughly [14]. Starting with pilot projects in specific departments or targeted use cases allows organizations to refine their approach and manage risks before scaling AI solutions across the board. Once routine tasks and resource allocation are optimized, advanced AI tools can further improve workflow coordination.
Leveraging Intelligent Agents for Workflow Management
Intelligent agents and AI platforms can take workflow management to the next level by coordinating complex processes across departments. These systems can handle task tracking, flag delays, and orchestrate team handoffs, helping prevent minor issues from escalating into larger problems. However, deploying these tools requires strong governance and oversight [3]. Healthcare organizations also need robust security strategies to address both the potential risks and benefits of AI. While AI can act as a threat vector, it can also serve as a powerful defensive tool [15]. Clinical Risk Management frameworks, such as Enterprise Risk Management, can guide the secure and effective implementation of these technologies [8].
Using Censinet for AI-Powered Cybersecurity Risk Management
As healthcare organizations embrace AI to enhance workflows, managing the cybersecurity risks tied to these technologies becomes a top priority. Censinet offers a platform specifically designed to address healthcare's complex risk environment. By combining automation with expert oversight, Censinet helps organizations scale their risk management efforts while maintaining safety and regulatory compliance.
Censinet RiskOps™: Streamlining Risk Assessments
Censinet RiskOps™ serves as a centralized tool for managing third-party and enterprise risks in healthcare. The platform automates traditionally manual risk assessment processes, making it easier for teams to evaluate vendors, medical devices, clinical applications, and supply chain partners. It ensures compliance with critical regulations like HIPAA while promoting collaboration among stakeholders such as IT security and clinical leadership. This collaborative approach ensures that risk management decisions align with operational priorities and legal requirements. With its automated capabilities, RiskOps™ also simplifies evidence gathering and integrates seamlessly with governance, risk, and compliance (GRC) systems.
Censinet AI™: Accelerating Risk Analysis
Censinet AI™ is designed to speed up third-party risk assessments by automating the creation of vendor questionnaires and summarizing evidence. The AI captures essential details, such as product integration specifics and fourth-party risks, and generates concise risk summary reports. While the AI handles time-consuming tasks like evidence validation and policy drafting, human oversight remains central. Configurable rules and review processes ensure that risk teams maintain control over critical decisions. This blend of automation and human judgment allows healthcare organizations to scale their cybersecurity efforts without sacrificing the nuanced decision-making required for complex risk scenarios.
Integrating AI Risk Management with GRC Systems
Censinet further strengthens AI risk management by embedding it within robust GRC frameworks. The platform automatically routes key findings and tasks related to AI risks to the appropriate stakeholders, including members of the AI governance committee, for review and approval. A real-time AI risk dashboard provides an easy-to-navigate view of all AI-related policies, risks, and responsibilities, serving as a central hub for continuous oversight and accountability. By aligning AI risk management with existing frameworks like Clinical Risk Management and Enterprise Risk Management, healthcare organizations can ensure that AI systems are governed with the same diligence as other tools handling Protected Health Information [8].
sbb-itb-535baee
Case Studies: AI Workflow Transformations in Healthcare
Healthcare organizations in the U.S. are already seeing the benefits of AI-driven workflow changes. With the AI healthcare market growing from $1.1 billion in 2016 to $22.4 billion in 2023 - and expected to hit $188 billion by 2030 - it's clear that AI is reshaping the industry[17]. Today, approximately 80% of hospitals use AI to enhance patient care and streamline their operations[17]. Here’s how AI is making an impact in key areas like hospital logistics, claims processing, and compliance.
Automating Hospital Logistics
Hospitals using AI-powered logistics systems have transformed how they handle equipment tracking, supply chains, and resource allocation. These systems rely on predictive analytics to forecast supply needs, maintain optimal inventory levels, and ensure critical equipment is always available. By automating these processes, hospitals not only reduce manual tracking errors but also allow staff to dedicate more time to patient care.
Reducing Claims Processing Time
Claims processing represents a large chunk of healthcare’s administrative costs - ranging from 15% to 30%[18]. AI-driven systems are stepping in to automate tasks like data entry, validating payer requirements, and processing claims more quickly and accurately than traditional methods. This speeds up reimbursements, minimizes denials, and improves overall efficiency. Beyond claims, AI also strengthens regulatory compliance efforts.
Improving Compliance Monitoring
AI tools are playing a crucial role in compliance monitoring by scanning documents, logs, and workflows to spot potential issues before they escalate into violations. These systems help healthcare organizations stay aligned with HIPAA and other regulatory standards. Moreover, AI-powered decision-making tools have reduced diagnostic errors by up to 30%[17], helping clinicians make decisions that adhere to established protocols and guidelines.
Future Trends in AI Workflow Design
The future of AI in healthcare is shaping up to be transformative, building on streamlined workflows and improved risk management strategies. Instead of isolated solutions, healthcare AI is moving toward a connected framework that integrates intelligent agents with clinical data systems. This shift isn’t just about technology - it’s about delivering measurable returns, increasing efficiency, cutting costs, and easing the workload on clinicians. These advancements are laying the groundwork for trends that will further redefine how AI supports healthcare workflows.
Agentic AI for Real-Time Decision Making
Agentic AI is changing the game by enabling workflows to adjust automatically in real time, without needing constant human input. By connecting different systems through protocols like the Model Context Protocol (MCP), it ensures secure data access while simplifying operations. This approach not only improves responsiveness but also paves the way for deeper integration across healthcare ecosystems.
Integrated Ecosystems for Better Collaboration
The future of healthcare AI lies in creating interoperable ecosystems that break down data silos. By combining specialized AI models with intelligent agents that securely share data in real time, these modular systems can significantly reduce the time and resources required for implementation. This means lower administrative costs, minimized revenue losses, and the ability for healthcare organizations to incorporate new tools more seamlessly, resulting in quicker operational benefits.
Predictive Risk Management with AI Dashboards
AI dashboards are revolutionizing risk management by shifting the focus from reactive measures to proactive strategies. These tools analyze data to predict potential issues, allowing for earlier intervention. For instance, predictive sepsis detection has been shown to cut ICU stays by $1,500 to $3,000 per case, potentially saving a 100-bed hospital $1 million to $2 million annually[19]. Similarly, Viz PE integration reduced the average consultation time for pulmonary embolism from four hours to just six minutes, leading to a 74% decrease in in-hospital mortality[1]. Beyond these clinical benefits, AI dashboards also monitor system performance, detect biases, and identify areas of degradation, giving healthcare leaders the insights they need to act before problems escalate.
Conclusion: Building a Resilient Healthcare Future with AI
Healthcare organizations are at a crossroads: they can either redesign workflows to effectively integrate AI or risk perpetuating inefficiencies that hold them back. A recent MIT study revealed that 95% of generative AI initiatives fail to produce measurable results, largely because they're layered onto flawed systems without addressing the need for adaptability, accountability, and trust [21]. With U.S. physician adoption of AI nearly doubling and two-thirds of doctors now using AI tools [21], the stakes for getting this right have never been higher.
Successfully integrating AI into healthcare demands strong governance frameworks. These frameworks should emphasize transparency, human oversight, and ongoing monitoring throughout the AI lifecycle. Physicians, ultimately responsible for patient care decisions, must remain at the center of this process [20]. Research by Yu et al. at Mayo Clinic and Zyter|TruCare highlights how this can work: when AI confidence levels were properly calibrated and explanations were made transparent, trust among physicians soared, reducing override rates from 87% to 33% [21]. Such frameworks also need to address the cybersecurity risks that come with AI.
Cybersecurity is a pressing issue. Since the FDA approved over 1,200 AI/ML-enabled medical devices starting in 1995 [21], every new integration has introduced potential vulnerabilities. To combat these risks, healthcare leaders must adopt comprehensive data governance policies that cover secure storage, access, aggregation, and deidentification [16][2].
Meanwhile, the evolving standard of care adds another layer of complexity. In some cases, not using available AI tools could be considered negligence [20]. This makes workflow redesign not just a matter of efficiency but a critical step for ensuring patient safety. Organizations that focus on transforming their processes - rather than merely adopting technology - will be better equipped to achieve meaningful clinical outcomes while staying compliant and safeguarding patients.
The path to a resilient healthcare future lies in treating AI as a driver for system-wide workflow transformation, not as a quick fix. Organizations that prioritize adaptability, establish clear lines of accountability, and embed trust into every aspect of their AI operations will lead the way in delivering better outcomes and safer care. These principles are the foundation of the broader movement toward reshaping healthcare workflows with AI.
FAQs
How can healthcare organizations redesign workflows to successfully adopt AI technologies?
Healthcare organizations looking to integrate AI into their workflows should begin by thoroughly analyzing their current processes. This helps pinpoint where AI can make the biggest impact. Involving clinicians and other stakeholders from the start is crucial to ensure the technology addresses practical needs and gains wider acceptance.
Key areas to enhance include automating repetitive tasks - like documentation using ambient listening tools - and improving clinical decisions with AI-powered support systems. A robust data infrastructure and comprehensive staff training are critical to a seamless rollout. Emphasizing transparency, accountability, and continuous monitoring not only fosters trust but also ensures adherence to healthcare regulations and effective risk management.
What challenges do healthcare organizations face when adopting AI into their workflows?
Adopting AI in healthcare workflows isn't without its hurdles. Organizations face challenges like limited staff training, resistance to change from healthcare providers, and concerns surrounding the accuracy and explainability of AI systems. On top of that, data quality issues, bias in algorithms, and cybersecurity risks add layers of complexity to implementation efforts.
Other obstacles include infrastructure constraints, steep implementation costs, and the necessity of aligning AI tools with regulatory and ethical standards. Tackling these issues requires a proactive approach: invest in comprehensive training programs, foster open communication about the advantages of AI, and ensure these tools are tailored to fit seamlessly into specific healthcare workflows.
What cybersecurity challenges does AI bring to healthcare, and how can they be addressed?
AI has brought significant advancements to healthcare, but it also opens the door to new cybersecurity risks. These include sophisticated threats like data breaches, tampering with AI systems, and weaknesses tied to outdated infrastructure or third-party integrations. Together, these vulnerabilities broaden the potential attack surface, underscoring the need for strong security practices.
To combat these risks, healthcare organizations should prioritize securing AI systems through measures like strict access controls, routine security evaluations, and continuous system monitoring. Adhering to healthcare compliance standards and introducing protections for AI models are also critical steps to safeguard patient data and reduce potential threats.


