Vendor Risk Assessment Methods for Healthcare: Quantitative vs. Qualitative Approaches
Post Summary
These methods evaluate third-party vendors to identify, measure, and mitigate risks, ensuring compliance, operational continuity, and patient safety.
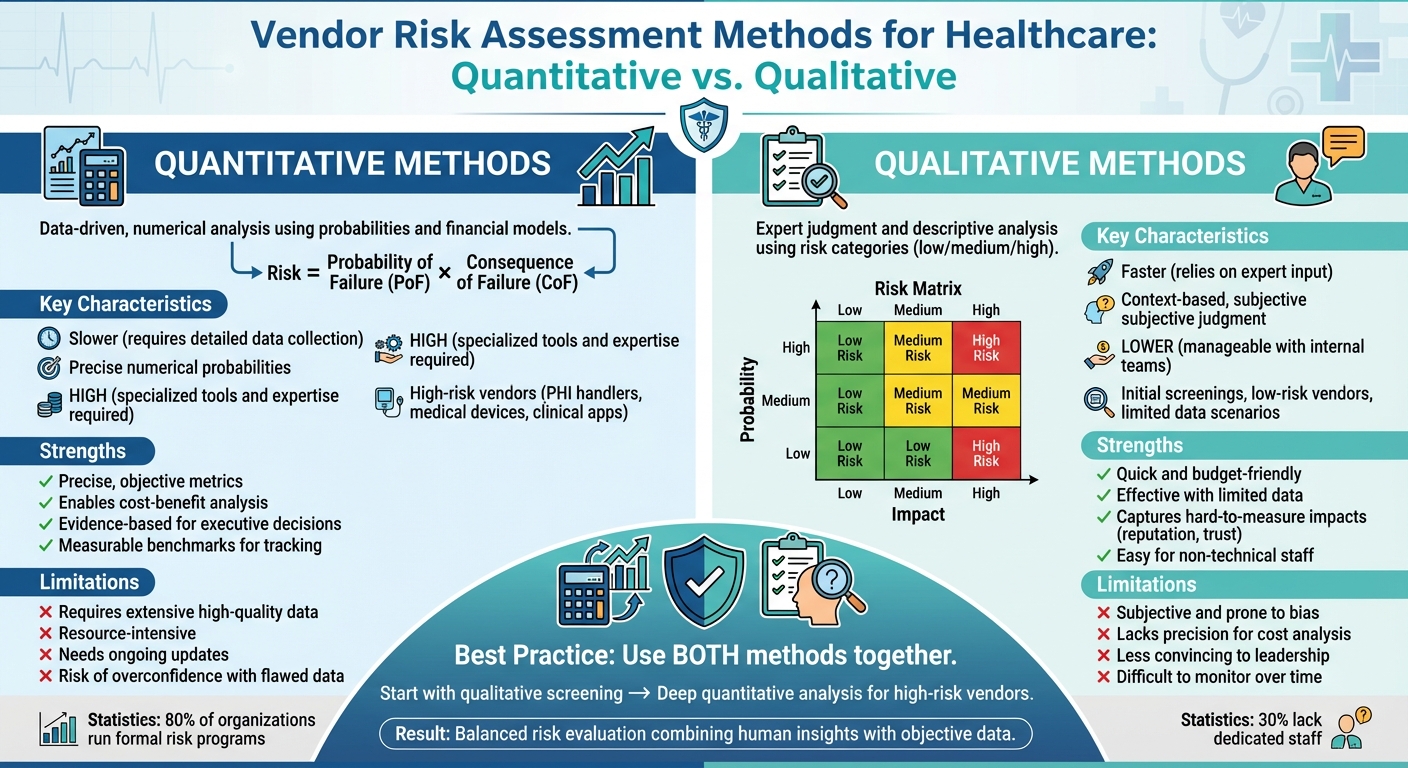
Quantitative assessments use numerical data and statistical models, while qualitative assessments rely on subjective ratings like high, medium, or low.
They provide precise, data-driven insights, enabling organizations to prioritize risks and allocate resources effectively.
They are faster, simpler, and useful when data is limited, making them ideal for initial evaluations or smaller organizations.
Use qualitative assessments for initial risk identification and quantitative methods for deeper analysis to create a balanced risk management strategy.
They protect patient data, ensure compliance with regulations like HIPAA, and mitigate risks that could disrupt critical healthcare operations.
Healthcare organizations rely on vendors to handle sensitive data and critical operations, but these partnerships come with risks. Assessing these risks is essential to protect patient information, ensure compliance with regulations like HIPAA, and maintain operational stability. Two primary approaches exist for vendor risk assessment:
- Qualitative Assessments: Use expert judgment, risk matrices, and descriptive analysis to evaluate risks, especially when data is limited or risks are hard to quantify (e.g., reputational harm).
- Quantitative Assessments: Rely on data, probabilities, and financial models to measure risks in numerical terms, offering precise insights for decision-making.
Each method has strengths and weaknesses. Qualitative methods are faster and less resource-intensive, while quantitative methods provide measurable, data-driven results. Combining both approaches offers a more complete risk evaluation, balancing human insights with objective data.
Quick Comparison:
| Factor | Quantitative | Qualitative |
|---|---|---|
| Speed | Slower, requires detailed data | Faster, relies on expert input |
| Accuracy | Precise, numerical probabilities | Context-based, relies on subjective judgment |
| Resource Needs | High, needs tools and expertise | Lower, manageable with internal teams |
| Best Use | High-risk vendors (e.g., PHI, medical devices) | Initial screenings, low-risk vendors |
Tools like Censinet RiskOps enable healthcare organizations to integrate both methods efficiently, ensuring a balanced and effective risk management strategy.
Quantitative vs Qualitative Vendor Risk Assessment Methods in Healthcare
Vendor Risk Assessment Basics in Healthcare
What Makes Healthcare Vendor Risk Assessment Different
Vendor risk assessment in healthcare carries unique challenges, largely driven by strict regulations and the sensitive nature of patient data. Unlike many other industries, healthcare organizations must comply with the HIPAA Security Rule, which legally requires covered entities and their business associates to perform risk assessments. This is a distinctive requirement that sets healthcare apart [3].
The primary focus is protecting protected health information (PHI). Every vendor assessment must identify potential vulnerabilities where PHI could be exposed and confirm compliance with HIPAA's administrative, physical, and technical safeguards [3]. This involves scrutinizing not just cybersecurity measures but also how vendors handle medical records, billing data, and patient communications throughout their operations.
To meet these demands, healthcare organizations use specialized tools like the ONC's and HHS OCR's Security Risk Assessment (SRA) Tool. These resources are tailored to the healthcare sector's regulatory environment, helping organizations navigate the complexities of vendor evaluations and maintain compliance.
Regulations and Standards That Guide Risk Assessment
The HIPAA Security Rule serves as the cornerstone for healthcare vendor risk assessments. It mandates organizations to evaluate risks and implement measures to protect electronic PHI (e-PHI), as outlined in 45 C.F.R. § 164.308(a)(ii)(A) [4]. This requirement extends to any vendors or consultants who create, receive, maintain, or transmit e-PHI [4]. While HIPAA doesn't prescribe specific methods for conducting assessments, it clearly defines the objectives that must be achieved [4][8].
The HITECH Act of 2009 expanded these obligations by holding business associates directly accountable for HIPAA compliance. It also introduced the Breach Notification Rule, which requires vendors to report data breaches [6][7]. The 2013 HIPAA Omnibus Rule further reinforced this, making vendors legally liable for meeting HIPAA standards [6].
Additionally, healthcare organizations often adopt NIST guidelines, such as Special Publication 800-30 and SP 800-66, as frameworks for securing e-PHI [4][5]. While these guidelines are officially required for federal agencies, they are widely used across the healthcare industry to shape compliance efforts. Another popular option is the HITRUST Common Security Framework, which offers a certifiable approach to standardizing vendor assessments across various regulatory requirements.
Data Sources Used in Vendor Risk Assessment
To meet these regulatory demands, healthcare organizations rely on a variety of data sources to assess vendor risks comprehensively. One key tool is the Vendor Risk Assessment Questionnaire (VRAQ). These structured questionnaires cover critical areas like security measures, compliance with industry standards, business continuity plans, and data protection practices [9]. They also address specific controls such as access management, encryption, incident response, and even risks posed by fourth-party vendors.
In addition to questionnaires, external audit reports play a crucial role. These reports independently verify vendor controls, providing detailed information on the scope of assessments, results, and any exceptions or remediation efforts [9][10]. Monitoring incident histories and requiring timely reporting of issues further ensures that risk assessments remain up-to-date and actionable.
Qualitative Vendor Risk Assessment Methods
What Qualitative Risk Assessment Involves
Qualitative risk assessment takes a descriptive approach, offering a way to evaluate risks when concrete data is limited. Instead of relying on hard numbers, it uses categories like "low", "medium", or "high" to rate the likelihood of a risk occurring and its potential impact. A common tool in this process is the risk matrix, which maps probability against impact on a scale (often from 1 to 5). For example, a vendor managing protected health information (PHI) might be rated as having a high likelihood of a data breach with a severe impact on patient privacy.
This approach often involves gathering insights through questionnaires, interviews, and document reviews to understand vendor security practices and identify vulnerabilities. By tapping into the expertise of security, compliance, and clinical professionals, qualitative assessments help prioritize risks in a way that aligns with the specific needs of healthcare organizations. This method is particularly effective for crafting a context-sensitive risk management strategy tailored to healthcare environments. [11]
When to Use Qualitative Methods in Healthcare
Healthcare organizations often turn to qualitative risk assessments when numerical data are hard to come by or impractical to measure. These methods are commonly used during initial vendor screenings, when onboarding new business associates, or when evaluating risks tied to emerging threats that lack historical data. They are especially helpful for assessing intangible risks, such as potential damage to patient trust, harm to an organization’s reputation, or a decline in staff confidence - factors that are difficult to quantify.
Additionally, qualitative methods can be a practical choice when resources are tight. Small security teams, limited budgets, or compressed timelines often make this approach appealing. For instance, early-stage vendor evaluations frequently rely on qualitative insights since detailed metrics or historical data may not yet be available.
Pros and Cons of Qualitative Risk Assessment
Here’s a breakdown of the advantages and challenges of using qualitative risk assessments in healthcare:
| Strengths | Limitations |
|---|---|
| Quick and budget-friendly – Delivers results without requiring extensive data collection or advanced tools | Subjective and prone to bias – Heavily influenced by individual judgment, which can vary between assessors |
| Effective with limited data – Useful for assessing new vendors or risks tied to emerging threats without historical metrics | Lacks precision – Offers general estimates rather than exact figures, complicating cost-benefit analysis |
| Captures hard-to-measure impacts – Evaluates risks like reputational harm or patient trust loss using descriptive scales | Less convincing to leadership – May not provide the numerical evidence needed to support decisions |
| Easy for non-technical staff to contribute – Welcomes input from clinical and administrative teams | Difficult to monitor over time – Changes in risk levels or improvements are harder to track without numerical benchmarks |
This balance of strengths and weaknesses makes qualitative risk assessment a flexible but imperfect tool, especially in dynamic and data-limited healthcare settings.
Quantitative Vendor Risk Assessment Methods
What Quantitative Risk Assessment Involves
Quantitative risk assessment swaps out vague, descriptive labels for hard numbers using a straightforward formula: Risk = Probability of Failure (PoF) × Consequence of Failure (CoF).
This approach leans heavily on data analytics and statistical modeling. For example, healthcare providers often pull from historical incident reports, vulnerability scans, and breach records to calculate these figures. The goal? To turn abstract threats into measurable data that can guide budgets and resource planning. By quantifying risks, healthcare organizations can zero in on priorities and allocate resources more strategically [12].
This data-driven foundation makes it possible to apply specialized tools and methods tailored to healthcare needs.
Quantitative Methods and Tools for Healthcare
To assess vendor risks, healthcare organizations often rely on structured methodologies. Risk scoring models, for instance, assign numerical weights to different risk factors, creating a composite score that allows for objective vendor comparisons.
The process is supported by tools like risk analysis software, vulnerability scanners, and incident response platforms. These technologies help refine the assessment, but they also come with their own set of complexities [12].
Pros and Cons of Quantitative Risk Assessment
Quantitative methods bring a level of precision that can be incredibly valuable, but they’re not without their hurdles. Here’s a breakdown of what works - and what doesn’t - in healthcare settings:
| Strengths | Limitations |
|---|---|
| Delivers precise, objective metrics by translating risks into monetary values and probabilities | Relies on extensive, high-quality data, which may not always be available for every vendor |
| Enables cost-benefit analysis by weighing mitigation expenses against potential losses | Requires significant resources, including specialized expertise and tools |
| Provides evidence-based insights that resonate with executive decision-makers | Demands ongoing updates and statistical analysis to remain accurate |
| Tracks risks over time with measurable benchmarks | Can lead to overconfidence if the data or assumptions are flawed |
When combined with qualitative methods, this quantitative approach offers a more rounded framework for vendor risk assessment. Together, they help healthcare organizations make better-informed decisions.
sbb-itb-535baee
Quantitative vs. Qualitative: Side-by-Side Comparison
How the Two Methods Compare
When it comes to choosing risk assessment methods, healthcare organizations have to consider a range of factors. Each method - quantitative and qualitative - has its own strengths, and the right choice often depends on the type of vendor, available resources, and how quickly the assessment needs to be completed.
| Factor | Quantitative | Qualitative |
|---|---|---|
| Speed | Slower - requires detailed data collection and statistical analysis | Faster - relies on expert judgment and existing knowledge |
| Accuracy | Provides precise numerical probabilities and financial impact | Offers contextual accuracy based on operational experience |
| Resource Requirements | Needs specialized expertise, advanced tools, and high-quality data | Less demanding - can often be managed by internal teams |
| Scalability | Harder to scale without automation and robust data systems | Easier to scale quickly across multiple vendors |
| Best for Healthcare Vendor Types | Ideal for high-risk vendors managing PHI, clinical apps, or medical devices | Best for initial screenings, low-risk vendors, or when limited data is available |
| Decision-Making Support | Supplies concrete numbers for budgeting and cost-benefit analysis | Adds context and operational insights to pinpoint risks |
In practice, many healthcare organizations don’t stick to just one method. A common strategy is to start with qualitative assessments to identify vendors that might need deeper, more detailed quantitative analysis. This tiered approach is a smart way to save resources while giving high-risk vendors the attention they require [14].
By understanding the strengths of each method, organizations can set the stage for combining both to get the best of both worlds.
Using Both Methods Together
When used together, quantitative and qualitative methods provide a more complete picture of vendor risk. Quantitative analysis offers hard data to prioritize risks objectively, while qualitative assessments add context, expert opinions, and operational insights [1].
For instance, qualitative evaluations might flag risks like poor vendor security practices or concerning employee behaviors. Quantitative tools can then assess the potential financial impact of these risks, giving healthcare organizations a clearer sense of what’s at stake [14]. In fields like healthcare and life sciences, combining failure data from audits with expert reviews of processes and human factors can improve compliance, quality, and overall reliability [1].
This blend of methods encourages collaboration across departments, helping teams develop actionable strategies that align with broader business objectives [1]. The result is a well-rounded view that balances hard data with human understanding [13][2].
How Censinet RiskOps Enables a Combined Approach

Censinet RiskOps is designed to meet the healthcare industry’s high-risk management standards by integrating both quantitative and qualitative methods. Its platform combines measurable data - like vulnerability scans, audit results, and incident tracking - with qualitative insights drawn from expert reviews, root cause analyses, and process evaluations.
With tools like Censinet AI™, the platform speeds up tasks such as completing security questionnaires, summarizing evidence, and generating risk reports. Importantly, it keeps decision-making in human hands by allowing teams to set rules and review processes. This human-in-the-loop approach ensures that automation enhances, rather than replaces, oversight during risk assessment.
The platform also provides a real-time dashboard that consolidates all risk-related policies, assessments, and tasks. This centralization ensures that the right teams focus on the right issues at the right time, enabling continuous monitoring, accountability, and governance across the organization. By combining both assessment methods, Censinet RiskOps helps organizations maintain a balanced and effective approach to risk management.
Key Takeaways
Summary of Both Assessment Approaches
Healthcare organizations don't have to pick sides when it comes to quantitative and qualitative risk assessments - they can use both to their advantage. Quantitative methods provide clear, measurable data, making it easier to track trends over time, compare vendor risks, and focus on high-risk areas consistently[15].
On the other hand, qualitative methods dig deeper into areas that numbers can't fully explain. By tapping into expert judgment, they evaluate factors like internal controls, operational processes, team expertise, and even workplace culture. These insights go beyond what purely numerical data can reveal[15].
Together, these methods create a more complete picture. As one industry analysis explains:
"Monitoring feeds capture external risk signals, while questionnaires provide deeper insights into internal controls and practices that the former simply can't uncover" – Veridion[15].
This combined approach lays the groundwork for practical steps in managing risks effectively.
Next Steps for Healthcare Risk Management
With nearly 80% of organizations running formal risk programs but 30% lacking dedicated staff[16], the challenge is clear: healthcare organizations need scalable solutions that won't overwhelm their teams. A smart first step is deciding which vendors need detailed quantitative assessments and which can be managed with qualitative methods. Vendors handling sensitive areas like PHI, clinical applications, or medical devices often require more rigorous, data-driven evaluations.
Censinet RiskOps makes managing both types of assessments easier. It combines automation with human oversight to streamline the process. Features like Censinet AI™ automate tasks such as filling out questionnaires, summarizing evidence, and generating reports, all while ensuring that critical human judgment is still part of the equation. The platform's real-time dashboard also helps teams quickly address risks, enabling them to assess more vendors efficiently without cutting corners. This approach ensures patient safety and supports better care delivery by scaling risk management operations to meet growing demands.
FAQs
What’s the best way for healthcare organizations to combine quantitative and qualitative risk assessments?
Healthcare organizations can make the most of quantitative and qualitative risk assessments by blending their unique advantages. Begin with qualitative techniques like expert opinions, interviews, and risk matrices to uncover detailed insights and pinpoint potential challenges. Follow this with quantitative methods - such as scoring systems, probability models, and financial impact analyses - to deliver clear, data-backed evaluations.
To maintain effective risk management, it’s crucial to regularly monitor and validate both approaches. This balanced strategy helps organizations combine a deeper understanding of risks with actionable, measurable outcomes, leading to better decision-making and stronger overall security.
What challenges do healthcare organizations face when assessing vendor risk under HIPAA regulations?
Healthcare organizations encounter numerous hurdles when it comes to evaluating vendor risks under HIPAA regulations. One major challenge is ensuring that third-party vendors adhere to HIPAA's Privacy and Security Rules. This often involves establishing solid Business Associate Agreements (BAAs) that clearly define each party's compliance responsibilities.
Another pressing concern is keeping a close eye on vendor security practices to safeguard against data breaches. On top of that, organizations must also tackle the problem of shadow IT - unauthorized tools or software that bypass security protocols. These hidden risks can lead to compliance violations and put sensitive patient information at risk.
Why would a healthcare organization opt for a qualitative approach instead of a quantitative one when assessing vendor risk?
Healthcare organizations often turn to a qualitative approach when dealing with risks that are tricky to quantify with numbers. This method shines in situations involving complex or nuanced issues, like evaluating new vendors, meeting compliance requirements, or tackling operational hurdles.
By leaning on expert insights and descriptive analysis, qualitative assessments offer a richer perspective on risks that numbers alone might miss. This approach is especially helpful when precise data is hard to pin down, or when the specific context surrounding a risk is a key factor in decision-making.
Related Blog Posts
Key Points:
What are vendor risk assessment methods in healthcare?
- Vendor risk assessment methods evaluate third-party vendors to identify, measure, and mitigate risks.
- These methods ensure compliance with regulations like HIPAA, protect patient data, and safeguard critical healthcare operations.
- They are essential for managing risks in vendor ecosystems, where 62% of breaches are linked to vendor vulnerabilities.
What is the difference between quantitative and qualitative risk assessments?
- Quantitative Risk Assessments:
- Use numerical data, scoring systems, and statistical models to measure risks.
- Provide precise, data-driven insights for prioritizing risks and allocating resources effectively.
- Qualitative Risk Assessments:
- Rely on subjective ratings like high, medium, or low to evaluate risks.
- Focus on expert opinions, descriptive evaluations, and tools like risk matrices and interviews.
- Both methods have strengths and limitations, and combining them often provides a more comprehensive risk management strategy.
What are the strengths of quantitative risk assessments?
- Data-driven insights: Provide objective, measurable evaluations of vendor risks.
- Predictive modeling: Use historical data to estimate the likelihood of risk events.
- Financial impact analysis: Convert risks into cost estimates, helping organizations plan for potential disruptions.
- Ideal for large vendor networks: Enable consistent monitoring and regulatory reporting.
What are the strengths of qualitative risk assessments?
- Faster and simpler: Useful for initial evaluations or when data is limited.
- Expert-driven insights: Leverage professional judgment to assess nuanced risks.
- Scenario-based evaluations: Simulate potential threats to evaluate vendor readiness.
- Best for smaller organizations or new vendor relationships: Helps identify red flags without requiring extensive data.
How can healthcare organizations combine these methods?
- Initial screening: Use qualitative methods to identify potential risks quickly.
- Deeper analysis: Apply quantitative methods for high-risk vendors or critical operations.
- Balanced strategy: Combining both approaches ensures comprehensive risk management, balancing speed with precision.
Why are vendor risk assessments critical in healthcare?
- Protect patient data: Vendors often handle sensitive Protected Health Information (PHI), making them a target for cyberattacks.
- Ensure compliance: Regulations like HIPAA and HITECH mandate thorough vendor assessments.
- Mitigate operational risks: Proactively addressing vendor vulnerabilities reduces the likelihood of disruptions.


