The boardroom has a new command center: cyber risk.
Post Summary
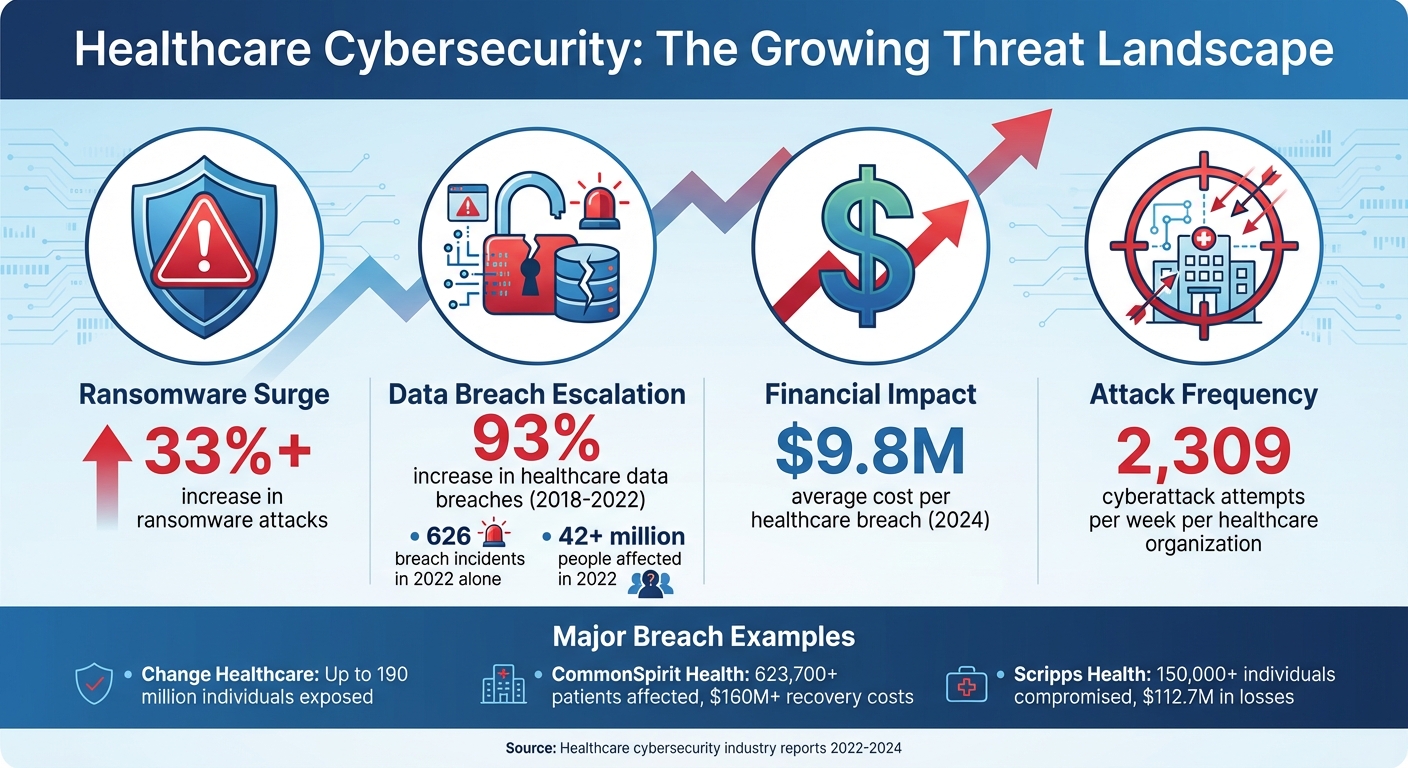
Healthcare boards must now treat cybersecurity as a top priority, on par with patient care and financial stability. Rising cyber threats - like ransomware attacks and data breaches - have exposed millions of patient records, disrupted operations, and cost healthcare organizations billions of dollars. Beyond financial losses, these incidents directly impact patient safety, making it critical for boards to take an active role in cyber risk governance.
Here’s what boards need to know:
- Cyberattacks are escalating: Ransomware incidents surged by over 33%, and healthcare data breaches affected 42M+ people in 2022.
- Financial stakes are high: The average cost of a healthcare breach hit $9.8M, with regulatory penalties and reputational damage adding to the burden.
- Patient safety is at risk: Cyberattacks disrupt critical care, delay treatments, and compromise medical devices.
- Regulations demand accountability: SEC rules now require public companies to disclose cybersecurity practices, with board members facing personal liability for failures.
To address these challenges, boards must:
- Establish dedicated committees for cybersecurity oversight.
- Use frameworks like NIST CSF and HITRUST to guide risk management.
- Monitor actionable metrics, including financial impacts, third-party risks, and security investments.
- Engage in scenario planning and require regular cybersecurity training.
- Leverage tools like Censinet RiskOps™ for centralized risk management.
Cybersecurity isn’t just an IT issue - it’s a core enterprise risk that demands board-level attention to protect patient care, finances, and organizational trust.
The Threat Landscape: Why Boards Must Act Now
Healthcare Cybersecurity Threat Statistics 2022-2024
Cyber Threats Facing U.S. Healthcare Today
Healthcare organizations are under siege from a growing wave of cyberattacks. In just the past year, ransomware attacks surged by more than a third [6], while healthcare data breaches climbed a staggering 93% between 2018 and 2022 [8]. In 2022 alone, 626 data breach incidents - each affecting at least 500 individuals - compromised the information of over 42 million people [8]. The rapid expansion of Electronic Health Records (EHRs) and Internet of Medical Things (IoMT) devices has only widened the attack surface. On top of that, cybercriminals are increasingly exploiting vulnerabilities in third-party vendors and leveraging artificial intelligence to create attacks that are harder to detect and even tougher to defend against.
The scale of these breaches is alarming. Take the Change Healthcare ransomware attack, for example - widely regarded as the largest healthcare data breach in U.S. history. Reports suggest that data from up to 190 million individuals may have been exposed, with costs running into billions [8]. Another high-profile case involved CommonSpirit Health, where a ransomware attack disrupted clinical operations at over 100 hospitals. This not only delayed patient care but also exposed Protected Health Information (PHI) for more than 623,700 patients, with recovery costs exceeding $160 million [8]. Similarly, Scripps Health endured a cyberattack that compromised data for over 150,000 individuals, resulting in financial losses estimated at $112.7 million [8].
These examples paint a clear picture: cyber threats are evolving rapidly, and healthcare boards must act decisively to strengthen oversight and safeguard their organizations.
Financial and Regulatory Costs for Healthcare Boards
The financial toll of cyber incidents goes far beyond the immediate costs of response and recovery. By 2024, the average cost of a healthcare data breach reached $9.8 million [8]. This figure includes direct expenses like forensic investigations, legal counsel, and notification efforts, as well as indirect losses from operational downtime and damage to the organization’s reputation. For healthcare boards, the stakes are even higher, as personal liability has become a pressing concern. Recent SEC rules now require public companies to promptly disclose material cybersecurity incidents. Additionally, annual reports must include detailed information about cybersecurity risk management, strategy, governance, and board oversight [5].
The SolarWinds case in October 2023 marked a pivotal moment in regulatory enforcement. The SEC filed a complaint against SolarWinds and its Chief Information Security Officer (CISO), Timothy Brown, accusing them of making misleading statements and omitting critical information about their cybersecurity practices. This followed the SUNBURST cyberattack, which caused a significant drop in the company’s stock value. SolarWinds ultimately agreed to a $26 million settlement in a securities class action brought by shareholders [5]. As highlighted by Skadden, Arps, Slate, Meagher & Flom LLP:
"The SolarWinds case is the first time the SEC has charged a CISO with fraud and highlights the increasing importance of cybersecurity under federal securities law" [5].
This case underscores the growing accountability of CEOs, CFOs, and board members. Personal penalties are now a real possibility in cases of false reporting or major breaches [7]. With these financial and regulatory risks mounting, boards must prioritize cybersecurity oversight to protect their organizations and themselves.
Patient Safety and Clinical Disruptions
Cyberattacks in healthcare don’t just compromise data - they put lives at risk. When systems go offline, the consequences ripple through the entire care network. Ambulances are diverted, surgeries are canceled, and critical treatments are delayed. The healthcare sector’s increasing reliance on digital systems means that a single breach can disrupt care delivery on a massive scale. Even medical devices connected to hospital networks present a growing vulnerability, giving cybercriminals another entry point to exploit.
These real-world incidents make it clear: cybersecurity is no longer just an IT issue - it’s a patient safety issue. Boards must treat it with the same level of urgency and scrutiny as clinical quality measures. Integrating cybersecurity into core oversight responsibilities isn’t optional; it’s essential to ensuring both operational stability and patient well-being.
Building Board Oversight for Cyber Risk
How to Structure Board Cybersecurity Oversight
After outlining the current threat landscape, let's explore how healthcare boards can effectively structure their oversight and use data-driven reporting to tackle cyber risk.
Cybersecurity must be treated as a core enterprise risk by healthcare boards [3][9]. The first step is to establish clear roles and responsibilities within the organization. Dedicated risk or audit committees should be formed to focus exclusively on cybersecurity [3][9]. These committees report directly to the full board, ensuring that cyber risk remains a strategic priority.
Another key step is appointing Business Information Security Officers (BISOs). Their role is to bridge the gap between technical complexities and actionable insights, making it easier for the board to grasp and address cybersecurity challenges [12].
Cyber Risk Metrics for Board Reporting
For boards to make informed decisions, cybersecurity data must be presented in financial and operational terms that resonate with their strategic goals [11][12]. Cyber Risk Quantification (CRQ) has become an essential tool, offering clear insights into potential financial losses and the effectiveness of security investments [11].
Healthcare boards should monitor a range of metrics, including:
- The probability and financial impact of potential cyber incidents.
- The organization's overall risk posture and how it changes over time.
- Scenarios detailing costs like compliance penalties, legal fees, and reputational damage.
- Third-party cyber risk exposure, which is particularly critical since healthcare organizations face an average of 2,309 cyberattack attempts per week [13].
- Return on investment (ROI) for proposed security measures.
- Recommendations for optimizing cyber insurance.
- Benchmarking performance against industry peers [11].
Metrics should cover areas like security, financial risks, compliance, third-party vulnerabilities, cyber resilience, and employee awareness. These data points provide actionable insights that boards can use to make strategic decisions [11][12].
By focusing on these metrics, boards can lay a strong foundation for scenario planning and ongoing education.
Scenario Planning and Board Education
Accurate metrics are just the beginning. Boards also need to engage in scenario planning and improve their understanding of cybersecurity threats. A 2018 survey revealed that only 36% of IT security professionals felt senior leadership viewed cybersecurity as a strategic priority, and 68% reported that boards were not adequately informed about cyberattack risks [3]. This gap in engagement must be addressed immediately.
Regular tabletop exercises simulating ransomware attacks can help boards prepare for real-world scenarios. After-action reviews following these exercises are critical for identifying gaps and improving response strategies [15].
Quarterly training sessions should be mandatory for board members, focusing on emerging threats and best practices [15]. At least one board member should have cybersecurity expertise or access to external advisors to provide informed guidance [15]. Additionally, CISOs should deliver quarterly reports that include updates on key risk indicators, threat intelligence, regulatory changes, cybersecurity investments, and industry benchmarks [15].
Specialized training that highlights the impact of cyber incidents on patient safety and regulatory compliance is crucial. This helps boards understand that cybersecurity isn't just an IT issue - it’s a matter of protecting patient care and the organization’s reputation.
Frameworks and Tools for Cyber Risk Management
NIST Cybersecurity Framework and HITRUST

Healthcare boards require structured approaches to effectively manage cyber risks, and frameworks like the NIST Cybersecurity Framework (CSF) and HITRUST CSF offer valuable guidance. The NIST CSF is a voluntary, risk-based tool built around five core functions - Identify, Protect, Detect, Respond, and Recover. With the release of version 2.0, a sixth function, Govern, was introduced to help organizations prioritize risks based on their specific environments and risk tolerance. Within a year of its release, 30% of American organizations adopted the NIST CSF, with adopters reporting a 66% reduction in insurance premium increases, even though only 44% of healthcare organizations met its standards [17].
"NIST cybersecurity standards are globally recognized for their comprehensive approach to managing cybersecurity risks. They are designed to help organizations safeguard sensitive data, stay compliant with regulations, and proactively address threats." – Cynomi [16]
HITRUST CSF, on the other hand, applies prescriptive controls tailored specifically for healthcare. Over 60% of hospitals and 70% of U.S. health plans have adopted HITRUST, benefiting from tools like MyCSF, which streamline data collection, reporting, remediation, and benchmarking [18]. While NIST allows for flexibility and customization, HITRUST provides clear, detailed requirements with scalable control levels [17][18]. Together, these frameworks go beyond basic HIPAA compliance, addressing gaps that regulations might miss and reducing the likelihood of data breaches or cyberattacks [17]. They also help integrate regulatory mandates, like HIPAA, into board-level risk management strategies.
HIPAA Compliance and Risk Analysis
HIPAA compliance plays a critical role in cyber risk management, and its requirements must be integrated into board-level discussions. The HIPAA Security Rule enforces the protection of patient records, with the Office for Civil Rights overseeing compliance [3]. Boards must understand that cyber risks are not just technical concerns - they’re enterprise-level issues, comparable to patient safety and care delivery.
To make HIPAA requirements more actionable, they should be translated into straightforward, nontechnical language. Highlighting potential penalties, breach costs, and regulatory specifics can emphasize the financial and operational risks of inaction, encouraging boards to align cybersecurity investments with broader organizational goals.
Establishing a dedicated cybersecurity committee is essential. This group should regularly review risk assessments, prioritize threats, and allocate resources to mitigation efforts [3]. Additionally, the committee needs to address third-party vulnerabilities [14] and engage clinicians to ensure that security measures align with clinical workflows and address frontline concerns [2]. Boards should also receive regular updates on the organization’s cyber risk profile, including the testing of incident response plans for scenarios like ransomware attacks [3][14]. Importantly, a cyber breach doesn’t automatically mean a HIPAA compliance failure - proper documentation and response protocols remain critical [3].
Censinet RiskOps™ as Your Command Center

Building on established frameworks, advanced platforms like Censinet RiskOps™ can centralize and streamline cyber risk management. This platform acts as a unified command center, consolidating third-party and enterprise risk assessments, cybersecurity benchmarking, and collaborative risk management.
Censinet’s AITM™ feature speeds up risk assessments by enabling vendors to complete security questionnaires in seconds. It automatically compiles evidence and documentation, identifies critical integration details and fourth-party risks, and produces detailed risk summaries. This blend of automation and human oversight ensures risk teams maintain control through configurable rules and review processes.
The platform’s advanced routing and orchestration functions operate like air traffic control, directing key findings and tasks to the appropriate stakeholders, including members of an AI governance committee. Real-time dashboards provide a single view of policies, risks, and tasks, ensuring continuous oversight and accountability. Healthcare organizations can choose from platform-only, hybrid, or fully managed services depending on their internal capabilities, making it a flexible solution for organizations of varying sizes and needs.
sbb-itb-535baee
Connecting Cybersecurity to Organizational Goals
Adding Cyber Risk to Enterprise Risk Management (ERM)
Cybersecurity touches every corner of an organization - patient care, finances, compliance, operations, and even reputation [19][20]. To address this, many boards are weaving cyber risk into their Enterprise Risk Management (ERM) frameworks. By leveraging tools like standardized scoring systems and heat maps, they can assess threats such as ransomware alongside other clinical and operational risks. This approach fosters a cybersecurity-first mindset across all levels, from the C-suite to the frontlines, and naturally leads to smarter, risk-based decisions when allocating resources.
Making Risk-Based Investment Decisions
Treating cybersecurity as a fundamental business risk is key to effective security governance. This means ensuring that every dollar spent on cybersecurity delivers the most impact in reducing risks. Boards can build a strong case for these investments by quantifying the potential costs of breaches, regulatory penalties, and operational downtime [4][1]. When cyber risk data is tightly connected to the organization's broader strategy, decision-makers are better equipped to choose investments that not only strengthen security but also enhance overall business performance.
Using Censinet RiskOps™ for Organizational Alignment
Censinet RiskOps™ bridges the gap between cyber risk management and organizational strategy. Its real-time dashboards and automated task routing enable seamless collaboration across clinical, operational, and security teams. This ensures everyone is aligned toward shared goals. The platform is designed to scale, offering flexibility for healthcare organizations of all sizes - whether they need a platform-only solution, a hybrid model, or fully managed services. By integrating cyber risk management into the wider organizational framework, boards can make well-informed decisions that enhance both security and operational outcomes.
Conclusion
Cybersecurity is no longer a back-office issue - it’s a boardroom priority. Healthcare boards must recognize that cyber risk is a strategic challenge with direct implications for patient safety, financial health, and organizational reputation [10][3][21][14]. With threats evolving rapidly - think AI-driven attacks or deepfakes - boards need to stay actively engaged in addressing these emerging vulnerabilities [10][6].
Reducing cyber risk starts with thoughtful planning and fostering a culture that prioritizes patient safety. Boards that integrate cybersecurity into their governance frameworks - using tools like the NIST Cybersecurity Framework or HITRUST - can establish clear accountability and reporting structures [22]. This approach ensures risks are managed effectively, keeping both patients and the organization protected.
Frameworks lay the groundwork, but tools drive action. Platforms like Censinet RiskOps™ offer boards a centralized hub for managing cyber risks. With real-time dashboards, automated workflows, and streamlined collaboration across teams, it provides the actionable insights needed to align cybersecurity efforts with organizational goals.
At its core, addressing cyber risk isn’t just about deploying technology - it’s about leadership, accountability, and fostering a proactive culture. By making cybersecurity a priority alongside patient care, healthcare organizations can better navigate today’s complex threat landscape. Strong governance ensures that data is secure, trust is maintained, and the ability to deliver quality care remains uncompromised [3][4].
FAQs
Why is cybersecurity a critical focus for healthcare boards today?
Healthcare boards are increasingly zeroing in on cybersecurity as a top priority, and it's easy to see why. The surge in cyberattacks - ransomware and data breaches, in particular - poses serious risks. These incidents can grind operations to a halt, expose sensitive patient data, and even threaten patient safety. It's no longer just an IT issue; it's a governance challenge that demands attention at the highest level.
On top of that, regulatory requirements and industry standards are tightening the screws, calling for stronger oversight of cybersecurity practices. Compliance isn't optional, and falling short can damage both the organization’s reputation and its operational stability.
By making cybersecurity a core focus, healthcare boards can not only protect patient information but also reinforce trust, ensure the organization stays resilient, and align security efforts with broader strategic goals. It’s about more than just defense - it’s about leadership in a digital age.
What steps can healthcare boards take to manage cyber risk effectively?
Healthcare boards play a crucial role in managing cyber risks by integrating cybersecurity into their governance strategies. This means making it a consistent part of their discussions and decisions. To do this effectively, boards should implement regular, in-depth risk reporting, establish committees that include members with cybersecurity expertise, and treat cybersecurity as a strategic priority.
It's also essential for boards to align cybersecurity initiatives with the organization's broader goals. Protecting sensitive patient information and ensuring compliance with regulations should be at the forefront. Key actions include routinely reviewing incident response plans, keeping a close eye on the organization's cyber resilience, and encouraging open communication between leadership and IT teams. These steps are vital to staying prepared for potential threats.
What are the best frameworks and tools for managing cybersecurity risks in healthcare?
To tackle cybersecurity risks in healthcare, organizations can rely on established frameworks like the NIST Cybersecurity Framework (CSF) and HITRUST CSF. These frameworks offer clear guidance for identifying, evaluating, and addressing cyber risks while staying in line with regulatory standards.
Another valuable option is ISO/IEC 27001, a globally recognized standard that helps healthcare organizations build strong information security management systems. By adopting these tools, healthcare providers can strengthen data protection, meet regulatory requirements, protect sensitive patient information, and maintain operational stability.
Related Blog Posts
- From Undervalued to Indispensable: How to Elevate ERM in Board-Level Discussions
- “From Downtime to Disaster: Why Clinical Resilience Demands New Thinking”
- “The Tools, Skills, and Mindsets That Will Define Risk Teams in the Next 5 Years”
- Benchmarking Study Finds Cyber Risk Governance Emerging as Board-Level Priority


