Common Cloud Security Risks in Healthcare and Solutions
Post Summary
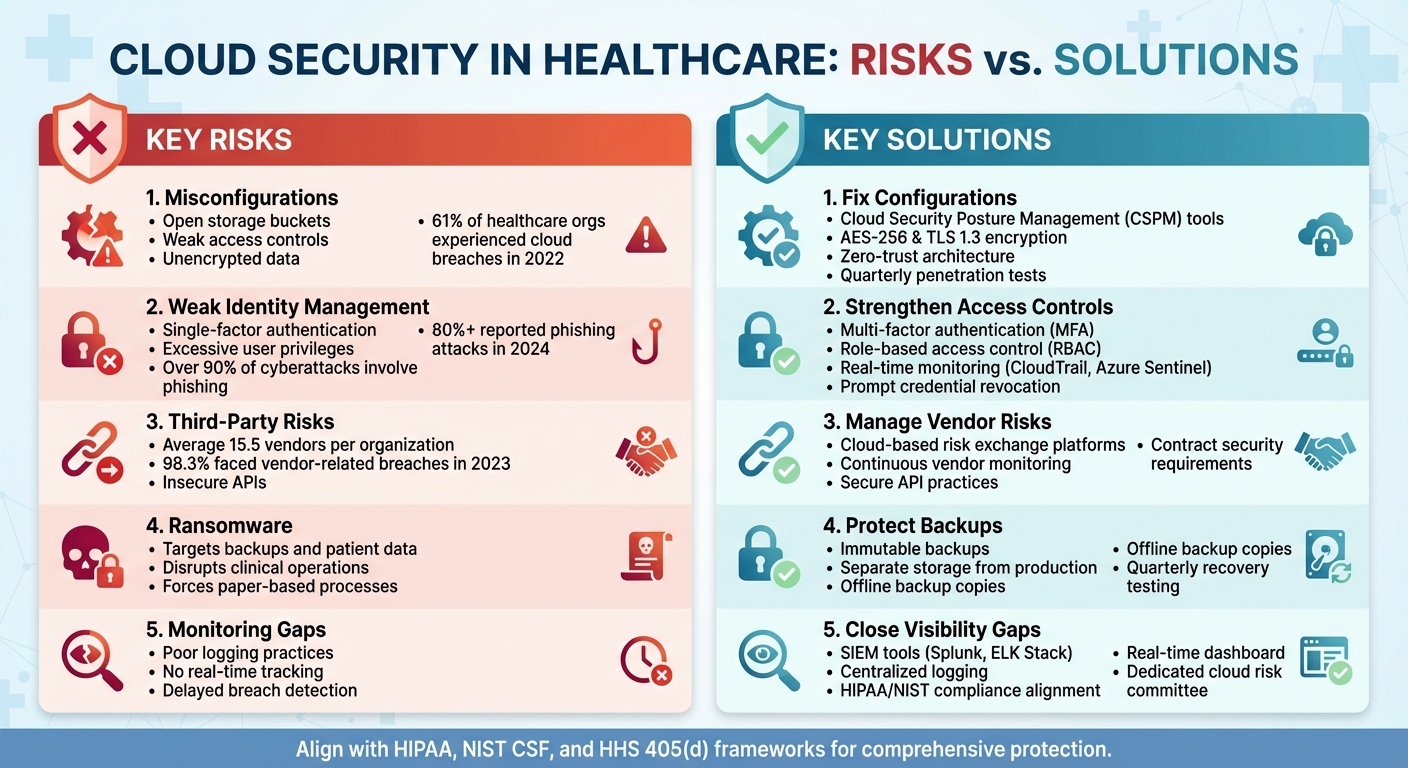
Common risks include misconfigurations, weak Identity and Access Management (IAM), ransomware attacks, vendor/API breaches, and poor encryption.
Cloud security protects sensitive patient data, ensures compliance with HIPAA, and mitigates risks like breaches, identity theft, and ransomware.
Challenges include managing misconfigurations, integrating legacy systems, addressing third-party risks, and ensuring consistent security across hybrid environments.
Best practices include implementing MFA, using CSPM tools, conducting continuous security testing, and training staff to recognize phishing attacks.
Organizations can prevent ransomware by maintaining immutable backups, using SIEM tools for threat detection, and enforcing strict access controls.
Vendors must ensure secure cloud configurations, provide encryption, and comply with healthcare regulations like HIPAA and GDPR.
Healthcare organizations rely heavily on cloud systems for managing patient data, telehealth, and medical tools. But with this shift comes serious security challenges, including data breaches, ransomware attacks, and compliance risks. Over 80% of healthcare providers reported phishing attacks in 2024, and nearly all faced vendor-related breaches in 2023. Here's a quick breakdown of the main risks and how to address them:
Key Risks:
- Misconfigurations: Open storage, weak access controls, and unencrypted data.
- Weak Identity Management: Single-factor authentication and excessive user privileges.
- Third-Party Risks: Vendor breaches and insecure APIs.
- Ransomware: Targeting backups and patient data.
- Monitoring Gaps: Poor logging and lack of real-time tracking.
Key Solutions:
- Use tools like Cloud Security Posture Management (CSPM) to fix misconfigurations.
- Enforce multi-factor authentication (MFA) and role-based access control (RBAC).
- Perform continuous vendor risk assessments and secure API integrations.
- Create immutable backups stored separately from production systems.
- Implement centralized logging and Security Information and Event Management (SIEM) tools.
By addressing these vulnerabilities with tailored strategies, healthcare providers can better protect sensitive data, ensure compliance, and maintain smooth operations.
Common Cloud Security Risks and Solutions for Healthcare Organizations
Common Cloud Security Risks in Healthcare
Healthcare organizations face a unique set of challenges when it comes to cloud security. These risks not only threaten sensitive patient data but also jeopardize regulatory compliance and clinical operations. Recognizing these vulnerabilities is crucial for creating cloud environments that safeguard both patients and providers. Below are some of the most pressing security risks in healthcare cloud systems.
Misconfigurations and Insecure Cloud Architectures
Cloud misconfigurations are a major issue for healthcare systems. According to the 2024 CSA report, they rank as one of the most frequent causes of ePHI (electronic Protected Health Information) exposure and compliance violations [2]. Common mistakes include leaving S3 buckets open with unencrypted data, allowing overly permissive access, failing to change default settings, and using weak network security groups. These errors make healthcare organizations a prime target for attackers.
In 2022, 61% of healthcare respondents reported experiencing a cloud infrastructure breach. Many of these breaches were tied to misconfigurations, especially during cloud migrations when storage solutions were improperly set up [4]. Attackers actively search for vulnerabilities like open buckets and weak access controls, exploiting them to access patient records, trigger HIPAA violations, and impose hefty fines.
Weak Identity and Access Management
Failures in Identity and Access Management (IAM) create easy opportunities for unauthorized access to sensitive healthcare data. Many healthcare organizations still rely on single-factor authentication, grant excessive user privileges, share accounts, and lack robust measures like multi-factor authentication (MFA) or timely credential revocation [2].
The numbers are alarming: over 90% of healthcare cyberattacks involve phishing schemes aimed at stealing credentials [2]. Once attackers gain access, weak IAM practices often allow them to move freely within systems, exposing electronic health records and other protected health information. These vulnerabilities also open the door to risks associated with third-party integrations and APIs.
Third-Party and API Risks
The interconnected nature of healthcare systems significantly expands the attack surface. On average, healthcare organizations work with 15.5 third-party vendors, and 98.3% reported breaches involving their partners in 2023 [2]. This reliance on external vendors handling sensitive data creates numerous entry points for attackers.
Insecure APIs and inadequate vendor assessments further complicate the situation. Third-party and supply-chain breaches are now the second most common cause of data compromises, trailing only ransomware attacks [2]. Unfortunately, traditional risk assessments - often based on lengthy questionnaires and spreadsheets - struggle to keep up with the rapidly changing cybersecurity landscape.
Ransomware and Backup Vulnerabilities
Ransomware attacks have adapted to target cloud-based workloads and backup systems in healthcare. Attackers understand that healthcare providers rely on uninterrupted access to patient data, making them more likely to pay ransoms when systems are locked down. The risk is compounded by improper backup configurations, such as storing backups in the same environment as production systems, infrequent backup schedules, or the lack of offline backup copies.
The fallout from a ransomware attack can be severe. Clinical systems may go offline, delaying patient care and forcing providers to revert to paper-based processes. These vulnerabilities are further amplified during transitions from legacy systems to cloud platforms, where inconsistent protocols and scattered data storage create additional risks [5].
Data Privacy and Monitoring Gaps
A lack of visibility into cloud environments creates exploitable blind spots for attackers. Common issues include poor logging practices, the absence of real-time monitoring, and difficulties with data residency and cross-border transfers. A systematic review identified confidentiality, data security, availability, integrity, and network security as the top challenges in healthcare cloud systems [3].
Without continuous monitoring, suspicious activities often go unnoticed until after a breach has occurred. Many healthcare organizations lack the tools needed to detect configuration changes, unauthorized access attempts, or data exfiltration in real time. This lack of visibility also makes it harder to reassess risks for critical components like APIs and containers, leaving systems vulnerable to evolving threats.
Solutions to Mitigate Cloud Security Risks
Healthcare organizations face a growing need to address vulnerabilities in cloud environments. Moving from reactive to proactive strategies is essential for protecting sensitive data and staying compliant with regulations. Here’s how organizations can strengthen their security measures while aligning with industry best practices.
Improving Cloud Configurations and Architecture
Using Cloud Security Posture Management (CSPM) tools is a smart way to catch misconfigurations like open S3 buckets, permissive access controls, or weak security groups before they lead to breaches. These tools conduct automated scans and provide recommendations, cutting down on manual tasks for security teams - a crucial step, as highlighted in the 2024 CSA report [2].
Encryption and network design are also critical. Employ AES-256 and TLS 1.3 for data encryption, and manage encryption keys securely with tools like AWS KMS. Adopting a zero-trust approach with features like micro-segmentation, VPCs, and security groups can help isolate sensitive data like Protected Health Information (PHI). Regular integrity checks, anti-malware scanning, and vulnerability assessments - along with quarterly penetration tests - help identify issues early. Automated monitoring tools can also flag risks tied to new APIs or containers, enabling teams to act swiftly.
Strengthening Identity and Access Controls
Tight identity management is non-negotiable. Require multi-factor authentication (MFA) for all accounts, using hardware tokens or authenticator apps for added security. Implement role-based access control (RBAC) to ensure users only have access to the data they need. For instance, clinicians might be limited to read-only access for specific patient records, ensuring sensitive information remains secure [2].
Given that over 80% of healthcare organizations reported phishing attacks in 2024, continuous monitoring of identity events is crucial [2]. Tools like AWS CloudTrail or Azure Sentinel can track login attempts, privilege escalations, and failed authentications in real time. They also alert teams to suspicious activity, such as logins from unfamiliar IP addresses or access during unusual hours. Promptly deactivating credentials for former employees further reduces risks.
Managing Third-Party and API Risks
Traditional vendor risk assessments, often reliant on spreadsheets and questionnaires, are too slow to keep up with modern threats. Instead, healthcare organizations should consider cloud-based risk exchange platforms designed for the industry's specific needs. These platforms enable faster, more secure sharing of cybersecurity data between healthcare providers and their vendors, streamlining risk assessments [1].
For example, Tower Health’s CISO, Terry Grogan, shared how adopting Censinet RiskOps significantly improved efficiency while reducing staffing needs [1]. This shift is especially important given that healthcare organizations work with an average of 15.5 third-party vendors, and nearly all (98.3%) experienced at least one vendor-related breach in 2023 [2].
Continuous vendor monitoring is key. Instead of relying solely on annual reviews, organizations can use platforms offering ongoing risk visibility. Including specific security requirements in vendor contracts and applying secure API practices - such as strong authentication, rate limiting, and frequent security testing - can further safeguard patient data.
Improving Backup and Recovery Strategies
A solid backup and recovery plan is essential for mitigating ransomware threats. Immutable backups prevent attackers from altering or deleting stored data, ensuring critical information remains safe even during an attack [2]. These backups should be stored separately from production systems, with offline copies kept for added security.
Encryption is a must for backup data, and disaster recovery procedures should be tested quarterly. Regular testing ensures systems can be restored quickly and confirms the integrity of backup data, aligning with the NIST Cybersecurity Framework [2].
Closing Monitoring and Compliance Gaps
Centralized logging through Security Information and Event Management (SIEM) tools like Splunk or the ELK Stack provides real-time insights into configuration changes, unauthorized access, and potential data breaches [2]. Aligning cloud security controls with frameworks like HIPAA, HHS 405(d), and NIST ensures compliance with regulatory requirements.
To maintain focus on cloud security, organizations can establish a dedicated cloud risk committee. Quarterly reviews, clear accountability for security responsibilities, and regular reporting on risk metrics to leadership can help keep cloud security a strategic priority. Documented policies and consistent oversight ensure that no gaps go unnoticed.
sbb-itb-535baee
Using Censinet for Healthcare Cloud Security

As healthcare continues to advance, so does the need for robust cybersecurity measures. Censinet offers solutions specifically designed to tackle the unique challenges of managing cloud-based healthcare data. With its Censinet RiskOps™ platform, the company provides a cloud-based risk exchange that connects over 50,000 vendors and products within a collaborative network of healthcare organizations [1]. This modern approach replaces outdated vendor assessment methods that struggle to keep up with today’s complex cloud security threats.
Streamlining Third-Party and Enterprise Risk Management
Censinet RiskOps™ redefines how healthcare organizations manage vendor risk assessments by moving away from traditional, repetitive questionnaire-based processes. Instead, it uses pre-mapped security questionnaires aligned with standards like HIPAA, NIST CSF, HICP, HITRUST, and SOC 2. Vendors can share a single security profile across multiple organizations, eliminating redundant efforts and speeding up the contracting process for cloud solutions.
The platform also reduces the resources needed for risk management. For example, Terry Grogan, CISO of Tower Health, shared that after adopting Censinet RiskOps™, their team size for risk assessments dropped from five full-time employees to just two, freeing up three staff members for other critical tasks [1].
According to James Case, VP & CISO of Baptist Health: "Not only did we get rid of spreadsheets, but we have that larger community [of hospitals] to partner and work with" [1].
Censinet RiskOps™ also promotes collaboration by allowing security, compliance, privacy, legal, and clinical teams to work directly with vendors on remediation tasks within a unified platform. Building on this streamlined vendor management, Censinet AITM™ takes risk assessments to the next level.
Accelerating Risk Assessments with Censinet AITM™
Censinet AITM™ leverages artificial intelligence to automate evidence validation, analyze questionnaires, and coordinate remediation efforts. By doing so, it slashes assessment times from weeks to just days. This rapid turnaround is critical, especially considering that over 80% of healthcare organizations faced phishing attacks leading to cloud breaches in 2024 [2].
The AI automatically validates key artifacts like SOC 2 reports, HITRUST certifications, penetration tests, and Business Associate Agreements. It flags vulnerabilities such as missing multi-factor authentication (MFA), misconfigured cloud storage, weak logging practices, and incomplete data encryption for protected health information (PHI). Once risks are identified, the system suggests remediation tasks, tracks vendor responses, and generates detailed risk summary reports. It also evaluates fourth-party risks and integrates findings into a centralized dashboard. Importantly, risk teams maintain control throughout the process, using configurable rules and review options to ensure automation supports - not replaces - critical decisions.
Centralizing Cloud Risk Governance for Healthcare
Censinet’s platform provides a comprehensive solution for managing cloud risks tied to patient data, PHI, clinical applications, medical devices, and supply chains. It supports the entire risk lifecycle, from assessment and scoring to remediation planning, documentation of residual risks, and ongoing monitoring. This centralized approach is vital, given that healthcare organizations work with an average of 15.5 third-party vendors, and 98.3% reported at least one vendor-related breach in 2023 [2].
The platform enforces HIPAA safeguards such as unique user IDs, role-based access control, multi-factor authentication, and continuous monitoring. Automated assessments and integrity checks help address common issues like improper credential revocation and misconfigured APIs, as outlined in HIPAA Security Rule requirements. Organizations can also schedule periodic reassessments, set alerts for major security events, and use dashboards to monitor unresolved critical risks across PHI workloads. Furthermore, the platform supports incident response workflows, documenting security events and tracking remediation efforts to ensure readiness for HIPAA and HHS reporting.
Conclusion
Healthcare organizations are grappling with growing cloud security challenges that put patient data, clinical workflows, and compliance at risk. Reports reveal that ransomware attacks, system misconfigurations, and weak identity management are among the leading causes of security breaches. Additionally, third-party compromises and credential-based attacks continue to expose critical vulnerabilities across the sector [2].
To address these risks, organizations need to adopt a proactive and continuous approach to risk management. This includes implementing robust identity and access controls like multi-factor authentication (MFA) and role-based access control (RBAC), encrypting data both at rest and in transit, performing regular vulnerability assessments, and conducting thorough evaluations of third-party risks. These steps align with HIPAA's core principles of confidentiality, integrity, and availability.
On top of these foundational strategies, healthcare-specific solutions can offer additional support by simplifying risk assessments, consolidating cloud governance, and leveraging AI-driven automation - all while ensuring human oversight remains central. By employing comprehensive frameworks that tackle vendor risks, API security, data backups, and ongoing monitoring, healthcare organizations can better safeguard patient safety and maintain seamless clinical operations in today’s cloud-reliant landscape.
Shifting from outdated, manual processes to AI-powered, collaborative tools represents a transformative step forward in healthcare cloud security. This evolution allows organizations to manage risks more effectively while meeting the high standards required for patient care and operational excellence.
FAQs
What steps can healthcare organizations take to manage third-party and API risks effectively?
Healthcare organizations can tackle third-party and API risks more efficiently by using risk management platforms tailored to the healthcare sector's specific needs. These platforms offer tools for continuous monitoring, simplify risk assessments, and make it easier to work closely with vendors to address security gaps.
With features that automate compliance tasks and enforce strict security standards, these solutions minimize manual workloads, enhance precision, and safeguard sensitive data like patient records and PHI. By adopting these technologies, organizations can take a proactive approach to risk management and uphold trust in their services.
What are the best ways to enhance identity and access management in healthcare cloud systems?
To strengthen identity and access management in healthcare cloud systems, begin by adopting multi-factor authentication (MFA) and enforcing robust password policies. These measures help minimize the risk of unauthorized access. Incorporating role-based access control (RBAC) is another essential step, as it ensures users can only access the data and systems relevant to their specific roles.
It's also important to regularly review and update access permissions to account for staffing changes. Adding continuous monitoring with audit logs can help detect potential vulnerabilities and address them promptly. Platforms like Censinet RiskOps™ are specifically designed to simplify access management, spot anomalies, and support compliance with healthcare industry standards.
Why are immutable backups essential for protecting healthcare organizations from ransomware attacks?
Immutable backups play a crucial role in healthcare organizations by ensuring that backup data remains untouched and cannot be modified or erased by ransomware attacks. This provides a secure recovery point, enabling healthcare providers to swiftly restore essential systems and patient data if an attack occurs.
By preserving the integrity and accessibility of sensitive information, immutable backups help healthcare organizations minimize downtime, maintain patient care continuity, and avoid permanent data loss during cybersecurity incidents. They are an essential part of a strong defense plan for protecting healthcare operations.
Related Blog Posts
Key Points:
What are the common cloud security risks in healthcare?
Common Risks:
- Misconfigurations: Misconfigured cloud systems expose sensitive patient data to unauthorized access.
- Weak IAM (Identity and Access Management): Poorly managed access controls increase the risk of breaches.
- Ransomware Attacks: Cybercriminals target healthcare cloud systems to encrypt data and demand ransoms.
- Vendor/API Breaches: Third-party vendors and APIs can introduce vulnerabilities if not properly secured.
- Poor Encryption: Inadequate encryption practices leave data vulnerable during storage and transmission.
Why is cloud security critical in healthcare?
Importance:
- Protects sensitive patient data, including electronic protected health information (ePHI).
- Ensures compliance with regulations like HIPAA, GDPR, and HITECH.
- Mitigates risks like identity theft, ransomware, and data breaches, which can disrupt patient care and damage reputations.
What are the challenges of securing healthcare cloud environments?
Challenges:
- Misconfigurations: Commonly overlooked errors in cloud setups can expose data.
- Legacy System Integration: Integrating cloud solutions with on-premises legacy systems creates security gaps.
- Third-Party Risks: Vendors and contractors may not adhere to the same security standards.
- Hybrid Environments: Ensuring consistent security across cloud and on-premises systems strains IT resources.
What are the best practices for mitigating cloud security risks in healthcare?
Best Practices:
- Multi-Factor Authentication (MFA): Adds an extra layer of security to prevent unauthorized access.
- Cloud Security Posture Management (CSPM): Identifies and remediates misconfigurations in real time.
- Continuous Security Testing: Simulates attack scenarios to identify vulnerabilities before they are exploited.
- Staff Training: Educates employees on recognizing phishing attacks and following security protocols.
How can healthcare organizations prevent ransomware in the cloud?
Prevention Strategies:
- Immutable Backups: Maintain backups that cannot be altered or deleted by ransomware.
- SIEM Tools: Use Security Information and Event Management (SIEM) systems to detect and respond to threats.
- Access Controls: Enforce strict access policies to limit exposure to ransomware attacks.
What role do vendors play in healthcare cloud security?
Vendor Responsibilities:
- Ensure secure cloud configurations and encryption practices.
- Comply with healthcare regulations like HIPAA and GDPR.
- Provide documentation and certifications to demonstrate adherence to security standards.


