Predictive Risk: Using AI to See Around Corners in Business Operations
Post Summary
Healthcare is under constant threat from cyberattacks, data breaches, and operational disruptions. Traditional methods of reacting to incidents are no longer enough. AI-powered predictive risk models now offer a way to identify and address potential risks before they escalate. Here’s how AI is transforming healthcare risk management:
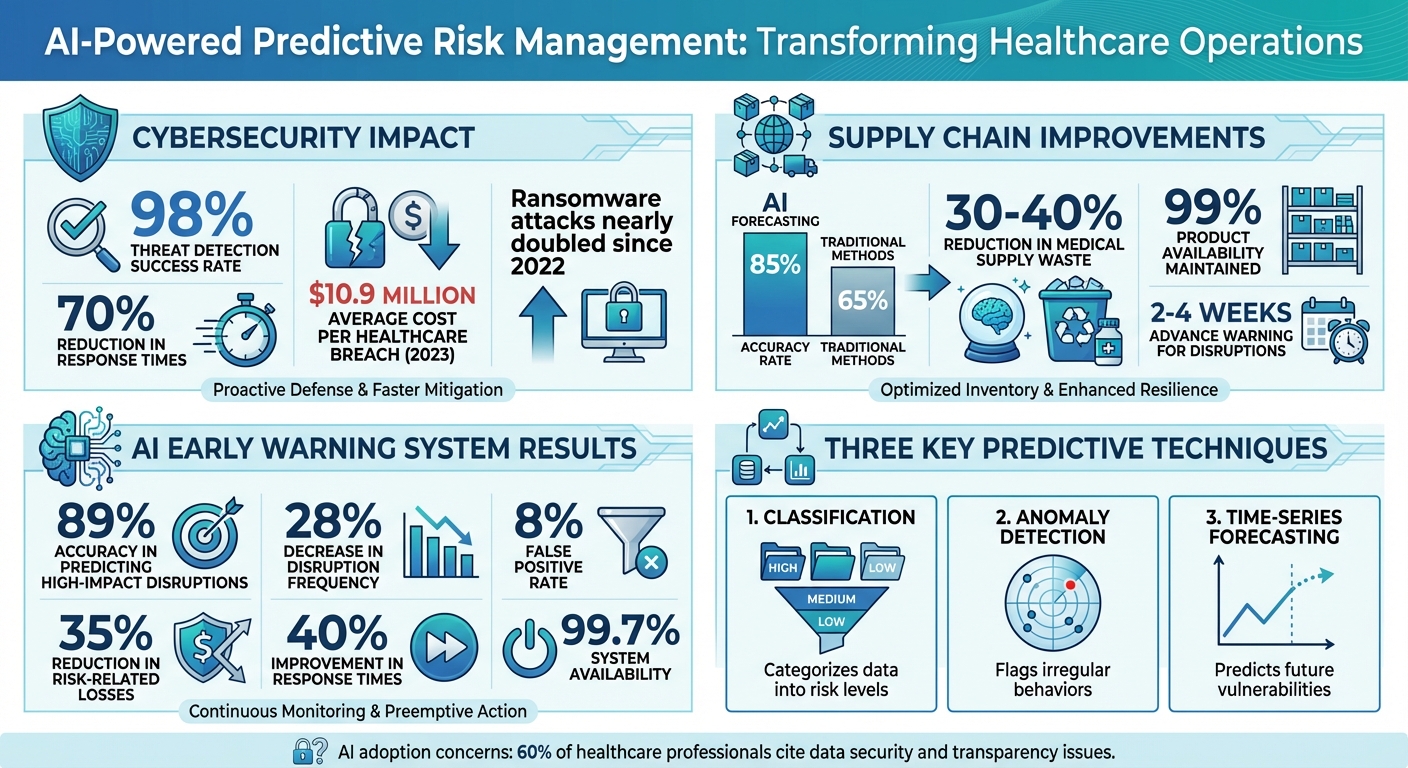
- Cybersecurity: AI detects threats with a 98% success rate and reduces response times by 70%. It identifies unusual patterns, prevents breaches, and protects patient data.
- Supply Chain: AI improves forecasting accuracy to 85%, reduces medical supply waste by 30-40%, and predicts disruptions weeks in advance.
- Vendor Risk: AI centralizes data on third-party vendors, enabling continuous monitoring and faster decision-making.
- Operational Continuity: Real-time monitoring ensures systems remain functional, protecting patient care and financial stability.
AI-driven tools like Censinet RiskOps™ simplify these processes by automating workflows, integrating data, and providing actionable insights. By using AI, healthcare organizations can prevent costly incidents, maintain compliance, and safeguard patient safety. However, ongoing monitoring, governance, and feedback loops are essential to keep these systems effective and secure.
AI-Powered Predictive Risk Management in Healthcare: Key Statistics and Impact Metrics
How AI-Powered Predictive Risk Models Work
AI-powered predictive risk models use machine learning, deep learning, and statistical algorithms to sift through data and anticipate potential threats. These models continuously evolve by learning from new data, making them adept at spotting patterns, detecting anomalies, and predicting risks in the ever-changing world of healthcare cybersecurity.
What sets these models apart is their ability to go beyond basic rule-based systems. Instead of relying on static rules, they learn from past incidents, uncover root causes, and apply this knowledge to current data. This dynamic learning process allows them to detect advanced threats that traditional systems might miss.
Predictive Techniques Used in Healthcare
AI-driven risk prediction in healthcare primarily relies on three techniques: classification, anomaly detection, and time-series forecasting.
- Classification: This method categorizes data into predefined risk levels using machine learning. For instance, systems can classify login attempts as legitimate, suspicious, or malicious by analyzing factors like location, timing, device type, and user behavior. Such algorithms have successfully identified unauthorized access to patient records, helping protect sensitive information and maintain trust [3].
- Anomaly Detection: This technique flags irregular behaviors that deviate from established norms. In healthcare, it might highlight unusual network activity, unexpected data transfers, or strange access patterns. AI systems excel at recognizing ransomware attacks in real time, reducing the risk of significant data loss or interruptions. By learning what "normal" looks like for users, devices, and networks, these systems can alert security teams to deviations that might signal a threat [3].
- Time-Series Forecasting: This approach analyzes historical data to predict future risks. For example, it can forecast when a system might become vulnerable based on patch cycles, usage trends, or seasonal cyber threats. Tools like Natural Language Processing (NLP) extract insights from unstructured data such as security logs and incident reports, while Generative AI enriches training datasets and simulates potential attack scenarios. Together, these techniques create a robust framework for predicting vulnerabilities.
Data Sources for Risk Prediction
To function effectively, AI models need diverse, high-quality data. Key data sources in healthcare include Electronic Health Records (EHRs), network telemetry, vendor assessments, medical device inventories, insurance claims, clinical trial data, and patient feedback [5][6][7][8]. These inputs provide a detailed view of potential risks.
- Network Telemetry: Offers real-time insights into traffic patterns, connection attempts, and data flows. Logs from firewalls, intrusion detection systems, and endpoints are essential for identifying anomalies.
- EHR Logs: Track who accesses patient records, when, and from where. This is critical for spotting insider threats or compromised credentials.
- Medical Device Inventories: Catalog connected devices, detailing software versions, known vulnerabilities, and patch statuses. This helps predict which devices may pose risks.
- Vendor Assessments: Collect data on third-party security postures, compliance certifications, and incident histories to gauge supply chain risks.
Additional inputs like wearable device data, genomic information, and clinical notes provide even more context. Standards like HL7 FHIR and APIs ensure seamless integration of these diverse sources, offering a comprehensive view of an organization’s risk profile [2].
Converting Predictions into Actions
The true value of AI predictions lies in their ability to drive actionable strategies. For healthcare organizations, clear outputs like risk scores, heat maps, and real-time dashboards are essential for turning complex data into meaningful decisions.
- Risk Scores: Assign numerical values to threats, assets, or vulnerabilities, helping prioritize resources. For example, a vendor might score 85 out of 100 based on their security practices, industry breach history, and the sensitivity of the data they handle.
- Heat Maps: Visually display risk levels across departments, systems, or locations, highlighting areas of highest exposure.
- Real-Time Dashboards: Unified platforms provide immediate alerts and insights, enabling quicker decisions.
As Cambridge College of Healthcare & Technology notes:
An AI can quarantine compromised systems, stop ransomware from spreading, and disable dubious accounts automatically, mitigating the potential damage significantly [3].
These systems also automate compliance checks, reducing the burden of manual audits and ensuring regulatory adherence [3]. By shifting from reactive to proactive risk management, AI-driven tools help prevent patient harm, regulatory violations, and financial setbacks. This approach translates predictions into practical, protective measures that safeguard healthcare organizations and their patients [2].
AI Use Cases for Risk Management
AI-powered predictive tools are already reshaping healthcare operations. These systems are helping organizations prevent breaches, anticipate supply shortages, and assess vendor risks with greater accuracy. By turning insights into action, AI demonstrates its ability to provide proactive protection across critical areas in healthcare.
Preventing Data Breaches and Ransomware Attacks
Cybersecurity threats in healthcare are on the rise. Ransomware attacks have nearly doubled since 2022, and healthcare continues to bear the highest cost per breach - reaching $10.9 million in 2023 [9]. AI-driven systems are stepping up to meet these challenges, analyzing vast datasets to identify unusual log-ins or unauthorized access to electronic health records (EHRs). This allows for real-time detection of potential threats [3].
In the event of an attack, AI can quickly isolate compromised systems, stop ransomware from spreading, and deactivate suspicious accounts, minimizing the damage [3]. According to LexisNexis Risk Solutions:
AI-enabled tools can be leveraged to protect against fraud by using the same kinds of tools – GenAI and predictive analytics are AI-driven solutions used to detect emerging threats and schemes [9].
Additionally, AI-based identity verification enhances security while ensuring patient care remains uninterrupted [9].
Predicting Supply Chain Disruptions
Supply chain issues can disrupt patient care and drive up costs. AI is transforming supply chain management by analyzing data from global shipping routes, weather patterns, and health outbreaks. This enables smarter decisions and helps prevent disruptions [10].
AI-powered demand forecasting achieves an 85% accuracy rate, compared to 65% for traditional methods, and AI-driven inventory systems cut medical supply waste by 30-40% while maintaining 99% product availability [10]. During the COVID-19 pandemic, AI models accurately predicted shortages of personal protective equipment (PPE) and ventilators, allowing suppliers to adjust production and distribution ahead of time [10].
A 2025 study in the Academic Journal of Computing & Information Science introduced an AI early warning system using machine learning. When deployed across manufacturing and distribution centers, it achieved 89% accuracy in predicting high-impact disruptions 2-4 weeks in advance, resulting in a 35% reduction in risk-related losses, a 28% drop in disruption frequency, and a 40% improvement in response times. The system maintained a low 8% false positive rate and 99.7% availability [11].
Managing Vendor and Third-Party Risks
AI also strengthens oversight of external vendors, a critical area of vulnerability for healthcare organizations. Third-party vendors often represent a significant cybersecurity risk. AI platforms centralize risk data, offering real-time insights and enabling faster, more informed decisions [2]. These tools support continuous monitoring, going beyond periodic assessments to detect threats in real time by analyzing vendor data flows for unusual patterns [12].
Predictive analytics and machine learning help identify potential risks, such as compliance issues or cybersecurity threats, before they become problems [2]. Health Catalyst highlights that:
AI-driven analytics and modern technology are redefining what's possible in healthcare risk management. These tools go beyond addressing traditional pain points - they empower hospital leaders to proactively identify, mitigate, and monitor risk in real time [2].
Platforms like Censinet RiskOps™ simplify vendor assessments with automation. Using Censinet AI™, vendors can complete security questionnaires in seconds. The platform then compiles vendor documentation, highlights key integration details, identifies fourth-party risks, and generates risk summaries. This approach not only reduces the time required for assessments but also ensures accuracy, enabling healthcare organizations to manage vendor risks at scale without compromising thoroughness.
How to Implement Predictive Risk Models
Putting AI-driven predictive risk models into action requires a well-thought-out plan. Healthcare organizations need to assess their current capabilities, establish a strong data infrastructure, and seamlessly integrate AI tools into their workflows. The aim is to create a system that not only delivers actionable insights but also adheres to compliance and security standards. By focusing on proactive risk predictions, organizations can turn strategic goals into real-time, impactful actions.
Assess Readiness and Set Goals
Start by evaluating your organization's current risk management capabilities and identifying areas that need improvement. This includes reviewing your cybersecurity measures, data management processes, and team expertise [2].
Pinpoint key risk areas where predictive models could have the most positive impact. For instance, if vendor breaches are a recurring issue, prioritize vendor risk management. If ransomware is the primary concern, focus on models designed to prevent breaches. Setting clear, focused goals helps improve predictive accuracy and ensures that resources are allocated to address the most pressing vulnerabilities [2].
Form an AI governance committee that includes representatives from legal, compliance, IT, clinical operations, and risk management [4]. This team will oversee AI-related activities, address potential biases, and ensure compliance with both federal and state regulations. They should also develop policies for AI procurement, deployment, and monitoring that align with industry standards. Transparency is crucial - over 60% of healthcare professionals have expressed concerns about adopting AI due to fears of data insecurity and lack of clarity [14]. A strong governance framework can help build trust and encourage adoption.
Design Data and AI Workflows
Implement a centralized risk data platform that integrates information from clinical, operational, financial, and workforce systems [2]. This requires robust interoperability through APIs to ensure data consistency across sources like electronic health records (EHRs) and incident reporting systems.
Ensure data is clean, organized, and properly labeled for training and deploying predictive models [2]. Real-time data pipelines are crucial for monitoring and forecasting, allowing AI systems to identify emerging threats as they arise. Additionally, review your compliance and security measures to confirm they include HIPAA-compliant cloud environments, encryption, audit trails, role-based access controls, and tools for managing regulatory updates and documentation [2].
Classify AI systems by their level of autonomy to match the degree of human oversight required for each system's risk level [13]. For high-risk applications, apply stricter governance controls to ensure compliance with regulations like HIPAA and FDA standards [13].
Using Censinet RiskOps™ for Integration
Once your data workflows are in place, the next step is to integrate insights into a unified platform. Censinet RiskOps™ offers a centralized solution that automates AI risk workflows. By consolidating data from various sources, it provides a single source of truth for risk information across the organization [2]. This eliminates data silos and fosters collaboration among clinical, financial, and operational teams [2].
Censinet AI™ takes collaboration further by enabling advanced routing and orchestration across Governance, Risk, and Compliance (GRC) teams. It directs key findings and tasks to the appropriate stakeholders, including members of the AI governance committee, for review and approval. With real-time data displayed in an intuitive AI risk dashboard, the platform ensures that the right teams address the right issues at the right time, promoting continuous oversight and governance.
The platform’s human-in-the-loop approach strikes a balance between automation and human decision-making. Risk teams maintain control through customizable rules and review processes, ensuring that automation supports rather than replaces critical decisions. This approach allows organizations to manage complex risks with greater speed and accuracy while prioritizing patient safety and care quality. By blending automation with human insight, healthcare leaders can scale their risk management efforts without compromising oversight.
sbb-itb-535baee
Measuring Impact and Improving Predictive Risk Programs
Using AI-driven predictive risk models is just the beginning. For these tools to remain effective, healthcare organizations need to measure their performance and adjust to new threats as they arise. This involves tracking the right metrics, ensuring models stay accurate, and establishing feedback systems that adapt to changing risks. These steps align with earlier strategies aimed at staying ahead of potential threats.
Track Success with Key Metrics
Start by identifying key performance indicators (KPIs) that match your organization's strategic goals [15][17]. These KPIs should directly reflect how well you're managing risks. For instance, in cybersecurity, you might monitor metrics like incident reduction rates, mean time to detect (MTTD), and mean time to respond (MTTR). Financial considerations are equally important - track savings from avoided breaches, lower insurance premiums, and reduced downtime.
AI-enhanced KPIs go beyond traditional metrics. They can be descriptive, predictive, and prescriptive, offering insights that connect real-time operational data with strategic planning [16]. For medical AI applications, performance evaluation should cover five critical areas: discrimination (how well the model differentiates outcomes), calibration (accuracy of probability estimates), overall performance, classification accuracy, and clinical utility (its actual impact on patient care) [18]. This approach ensures you're not just measuring technical success but also assessing the real-world benefits. In short, effective metrics provide both a snapshot of past performance and a roadmap for future improvements.
Maintain Model Accuracy and Governance
AI models aren't static - they need ongoing attention to stay effective. Over time, issues like model degradation, data drift, and inaccuracies can reduce their reliability [1][4][2]. Regular monitoring and retraining are essential to keep models performing well. As threats evolve and data patterns shift, continuous validation helps ensure these tools remain capable of identifying and addressing new risks.
Another critical aspect is addressing algorithmic biases. These biases can undermine trust and reliability if left unchecked [1][4][2]. An AI governance committee should oversee this process, assigning clear responsibilities for clinical and operational oversight [13]. This includes monitoring predictions for bias and ensuring compliance with HIPAA and other regulations. Human oversight is equally important - risk teams should review model outputs to confirm that the automated recommendations align with organizational policies and uphold patient safety standards.
Refine Models with Feedback Loops
Predictive risk models should be designed to adapt and improve over time. By incorporating real-time monitoring, AI and machine learning systems can identify patterns and detect abnormalities, such as unusual login activity or unauthorized access to electronic health records (EHRs). This proactive approach helps spot emerging threats before they escalate [3].
Real-time dashboards can be a valuable tool for tracking model performance and identifying risk trends. Documenting the outcomes of flagged threats - whether they were true positives, false positives, or misses - provides essential data for retraining models and refining risk controls [1]. A systems-based analysis can also uncover vulnerabilities across your digital infrastructure [1]. As cybercriminals increasingly use AI to enhance their attacks, organizations must continuously improve their defenses to stay ahead [3][9]. By integrating feedback loops into your risk management framework, you create a cycle of ongoing improvement that strengthens your ability to manage threats effectively.
Conclusion: Managing Risk with AI
Healthcare organizations can no longer afford to handle cybersecurity risks on a reactive basis. With ransomware attacks doubling since 2022 and breaches costing as much as $10.9 million in 2023, the stakes have never been higher [9].
AI-driven models are transforming risk management by shifting the focus from reacting to threats to anticipating them [1][2]. By analyzing historical and real-time data, these models can pinpoint high-risk areas, helping to prevent data breaches, maintain compliance, and safeguard patient safety. As cyberattacks become increasingly advanced, AI is emerging as a critical tool for protecting sensitive patient information and ensuring operational stability [3]. This proactive mindset paves the way for effective implementation strategies.
One example of this shift is Censinet RiskOps™, which simplifies predictive risk management. The platform automates third-party assessments, compiles vendor evidence, and directs critical findings to the right teams for review. By combining human oversight with automation, healthcare organizations can manage cyber risks effectively without compromising on safety or control. Its AI-powered risk dashboard consolidates real-time data, enabling a cohesive approach to governance and accountability across the organization.
While these advancements are promising, they also highlight new challenges. AI is revolutionizing clinical workflows and diagnostics, but its integration introduces cybersecurity risks, such as algorithmic transparency issues and vulnerabilities in AI-controlled medical devices [1][9]. Organizations that adopt AI for predictive risk management today will be better prepared to safeguard patient care and ensure operational resilience in the future. The message is clear: adopting AI-driven risk management is no longer optional - it’s essential for securing the future of healthcare.
FAQs
How does AI enhance cybersecurity in healthcare operations?
AI is transforming cybersecurity in healthcare by providing real-time threat detection, predictive analytics, and automated responses. It keeps a constant watch over systems, devices, and user activities, identifying vulnerabilities and addressing potential risks before they escalate into major breaches.
With its ability to process massive amounts of data quickly and with precision, AI helps healthcare organizations stay one step ahead of threats like ransomware and data breaches. This proactive stance not only protects sensitive patient information but also fortifies the overall security of healthcare operations.
How does AI help healthcare organizations address supply chain disruptions?
AI empowers healthcare organizations to stay ahead of supply chain challenges by analyzing massive datasets, including inventory levels, patient needs, geopolitical trends, and weather patterns. By spotting risks early, AI can create risk assessments, model different scenarios, and suggest strategies to minimize potential disruptions.
On top of that, AI automates alerts and adjustments, enabling quick responses to issues like shortages or interruptions caused by events such as pandemics or natural disasters. This ensures healthcare providers can maintain smooth operations and continue delivering care without interruptions.
What steps can healthcare organizations take to effectively use AI for predictive risk management?
Healthcare organizations can harness AI for predictive risk management by blending cutting-edge technology with well-structured frameworks and human oversight. A crucial first step is implementing real-time monitoring to identify and address potential threats as they arise. AI can process vast datasets, predict vulnerabilities, and streamline tasks like threat detection, incident response, and evaluating risks from third-party vendors.
To ensure trust and regulatory compliance, it’s important to use explainable AI (XAI) and adhere to standards such as HIPAA. Regular testing and validation of AI models help reduce biases, while consistent staff training ensures teams can effectively leverage these tools. Additionally, keeping a close watch on IoMT (Internet of Medical Things) devices for any suspicious activity is key to bolstering cybersecurity and maintaining operational stability.


