AI Monitoring in Healthcare Supply Chains
Post Summary
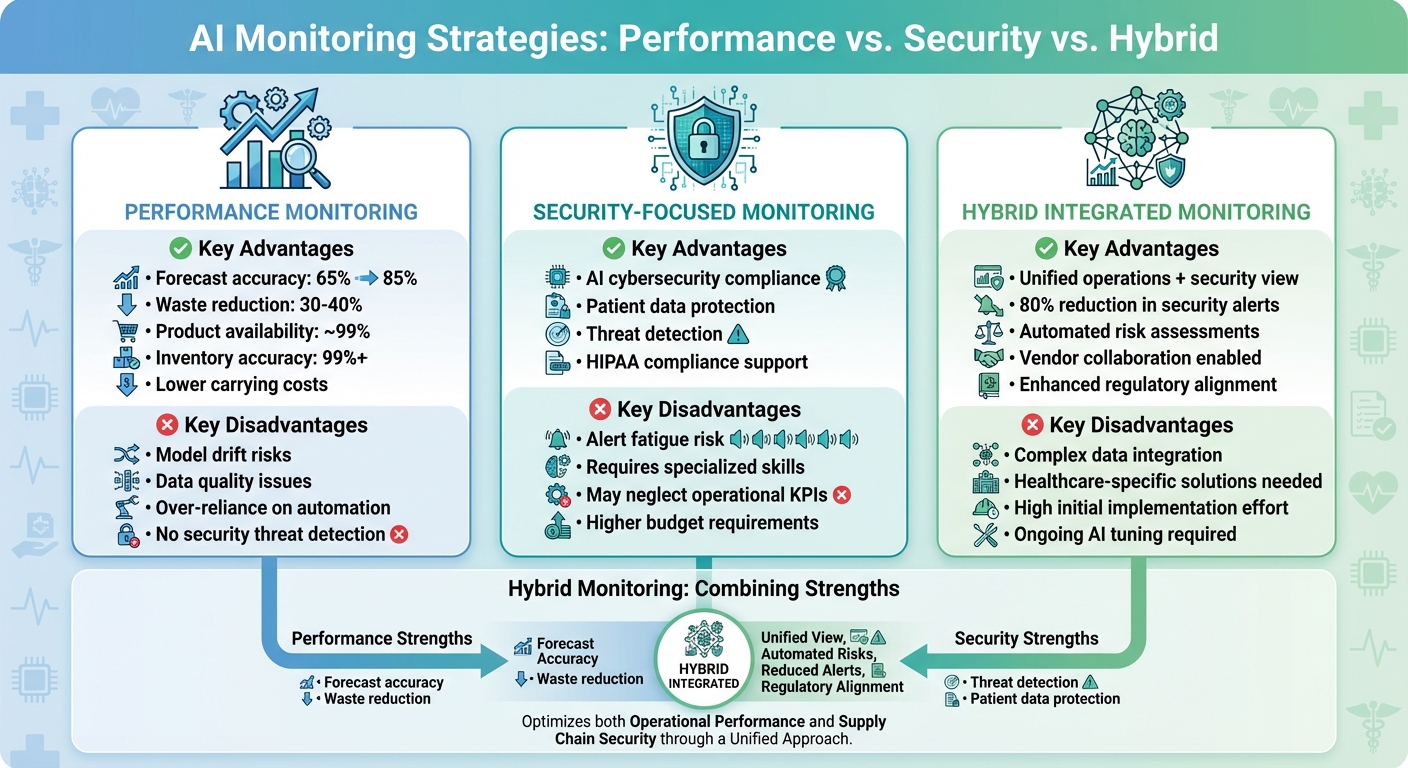
AI is transforming healthcare supply chains by improving efficiency and security. Hospitals face challenges like outdated tracking methods, regulatory demands, and supply chain disruptions that can impact patient safety. AI-powered monitoring addresses these issues through three key strategies:
- Performance Monitoring: Tracks inventory, predicts demand, and reduces waste. AI improves forecasting accuracy to 85% and cuts supply waste by 30–40%.
- Security Monitoring: Protects patient data and supply chain systems by detecting cyber threats and monitoring vendor activity. AI consolidates alerts, reducing noise by 80%.
- Hybrid Monitoring: Combines performance and security insights into a unified system, enabling better decision-making and compliance with regulations like HIPAA and FDA guidelines.
While these strategies improve supply chain management, implementation requires integrating fragmented systems, maintaining data quality, and aligning with healthcare regulations. Starting with high-priority areas, like temperature-sensitive drugs and critical devices, can help healthcare organizations realize the benefits of AI monitoring while addressing both operational and security challenges.
1. Performance Monitoring
Performance monitoring keeps a constant check on the operational flow of healthcare supply chains. It evaluates how effectively AI models handle demand forecasting, inventory management, delivery route optimization, and cold-chain maintenance. By tracking metrics like forecast accuracy, stockout rates, inventory turnover, expiration-related waste, and on-time deliveries, this process ensures that potential problems are identified early. The goal? To minimize waste and guarantee that essential supplies reach patients without delays.
Impact on Operational Efficiency
AI-powered demand forecasting has proven to outperform traditional methods [2]. The results? Leaner inventories and fewer last-minute, costly emergency orders. Some healthcare systems have reported a 30–40% cut in supply waste while maintaining product availability rates close to 99% [2]. Additionally, computer vision systems nearly eliminate errors in inventory checks, saving staff from tedious manual counts [3][5]. For cold-chain items like vaccines and biologics, IoT sensors combined with AI provide real-time monitoring of critical factors such as temperature, humidity, and transit time. These systems send alerts if storage conditions deviate from FDA-approved ranges [6]. Beyond tracking past performance, they also predict risks like temperature fluctuations or delivery delays, enabling proactive solutions.
Implementation Complexity
Rolling out effective performance monitoring comes with its own set of hurdles. Many healthcare systems rely on fragmented legacy platforms - separate ERPs, inventory systems, and distributor portals - which require seamless integration and standardized data [3][9]. Poor data quality, such as inconsistent product codes or incomplete supplier details, can undermine the accuracy of AI models and the usefulness of performance metrics [2][3]. Customization is another challenge. For example, supply chain leaders need network-wide insights, while materials managers benefit more from location-specific alerts. Without carefully calibrated thresholds and tailored dashboards, teams can experience alert fatigue, where notifications are ignored entirely [3][9]. Just as important as the technology is fostering a culture where staff actively use dashboards, investigate anomalies, and refine workflows. These operational challenges highlight the importance of systems that not only deliver actionable insights but also comply with strict regulatory standards.
Alignment with U.S. Healthcare Governance
In the U.S., performance monitoring must align with stringent healthcare regulations. When AI systems handle data like procedure schedules or diagnosis codes, they must meet HIPAA and HITECH standards for encryption, access control, and audit logging [10]. Similarly, tracking pharmaceutical distribution must comply with FDA good distribution practices and the Drug Supply Chain Security Act (DSCSA), which requires traceability for prescription drugs. To stay ahead of evolving governance, organizations need to document the purpose of their AI models, data sources, and performance metrics. This is vital for internal governance reviews and external audits by entities like CMS, the Joint Commission, or state health departments [8][10]. Recent guidance from the Health Sector Coordinating Council emphasizes the importance of cataloging AI tools, monitoring third-party AI systems, and defining clear accountability for both performance and security. In this way, performance monitoring not only supports daily operations but also provides the necessary audit trail to ensure compliance and foster ongoing improvements.
2. Security-Focused Monitoring
Security-focused monitoring takes a different approach from performance monitoring by concentrating on threat detection and access control within healthcare supply chains. While performance monitoring ensures smooth operations - like forecasting demand or managing inventory - security monitoring acts as a safeguard, protecting against unauthorized access, data breaches, suspicious vendor activity, and vulnerabilities in third-party connections. The stakes couldn’t be higher: a single breach in a logistics platform or vendor system could expose sensitive patient health information (PHI), disrupt critical care, and lead to steep regulatory penalties.
Impact on Security
AI-powered security monitoring excels at spotting unusual behavior that traditional tools might miss. These systems are designed to detect advanced threats like lateral movement, privilege escalation, and command-and-control activities across data centers, cloud environments, and third-party integrations [7][10]. One standout capability is monitoring medical IoT devices - such as infusion pumps, imaging systems, and patient monitors - without requiring agent-based software. This is crucial because many clinical devices aren’t compatible with traditional endpoint security tools [7].
Some AI-based solutions have even reported an 80% reduction in critical alerts by consolidating noisy, low-value detections into fewer, more actionable alerts based on attacker behavior. This not only enhances the efficiency of security operations centers (SOC) but also allows teams to focus on genuine threats [7]. However, achieving these security advancements isn’t without its challenges, particularly when it comes to integration.
Implementation Complexity
For security monitoring to be effective, it needs to pull data from a variety of sources: network telemetry, supply chain systems, vendor risk assessments, and threat intelligence feeds [3][4][7][10]. The challenge lies in harmonizing this data and fine-tuning AI models to reduce false positives while aligning with the organization’s specific risk tolerance [7][10]. Tools like Censinet RiskOps™ are designed to tackle these complexities by offering streamlined third-party risk assessments, collaborative risk management, and secure data sharing across healthcare delivery organizations (HDOs) and their vendors.
Alignment with U.S. Healthcare Governance
Security-focused monitoring must also meet the stringent requirements of regulations like HIPAA and HITECH. For example, it needs to align with the HIPAA Security Rule, which mandates safeguards for access control, audit trails, data integrity, and secure data transmission [10]. AI systems that monitor vendor access to PHI or flag unusual activity in supply chain systems not only enhance security but also generate detailed audit logs. These logs are invaluable for responding to Office for Civil Rights (OCR) investigations, documenting incidents, and conducting risk analyses required under federal healthcare laws [10].
Looking ahead, the Healthcare & Public Health Sector Coordinating Council (HSCC) is preparing AI cybersecurity guidelines for 2026. These guidelines will outline best practices for managing third-party AI tools and monitoring AI-driven supply chains [8]. To stay ahead, healthcare organizations must establish strong governance frameworks that bring together security, supply chain, and compliance teams. By regularly reviewing AI-generated insights, prioritizing fixes, and aligning monitoring controls with regulatory standards, organizations can not only detect threats but also demonstrate compliance with both federal and state regulations. This dual focus ensures that security monitoring serves as both a protective measure and a compliance tool.
3. Hybrid Integrated Monitoring
Hybrid integrated monitoring is the evolution of healthcare supply chain management, combining AI-driven operational insights with real-time security oversight. Instead of relying on separate tools for tasks like demand forecasting and threat detection, this approach unifies supply chain optimization with cybersecurity monitoring. It’s a dual-purpose system that tracks inventory levels, vendor behavior, device vulnerabilities, and access patterns simultaneously. The result? A clearer picture of both operational performance and security risks, building on the strengths of earlier monitoring methods.
Impact on Security
By merging security and operational data streams, hybrid systems can detect anomalies that might signal a compromised vendor account or an emerging cyber threat. This comprehensive view enhances cybersecurity across vendors, third parties, patient data, medical records, medical devices, and the entire supply chain. For example, platforms like Censinet RiskOps™ enable healthcare organizations and vendors to securely collaborate in real-time, sharing cybersecurity and risk data. This creates a unified defense network capable of addressing both operational and security challenges at the same time [1].
While strong security measures remain essential, integrating these with operational data ensures a more streamlined and proactive approach to supply chain management.
Impact on Operational Efficiency
Hybrid monitoring also lightens the load for risk management teams. By automating processes like risk assessments and data collection, organizations can reduce manual work and allocate resources more effectively. For instance, replacing spreadsheets with AI-powered assessments allows for deeper evaluations with fewer resources. This approach has led to a 30–40% reduction in inventory waste and maintained product availability at nearly 99% [2]. Meanwhile, intelligent alert correlation has reduced security alerts by 80% [7], freeing up staff to focus on more strategic tasks.
Implementation Complexity
Setting up hybrid monitoring isn’t without its challenges. It requires integrating data from a wide range of sources, such as EHR and ERP systems, warehouse management tools, network telemetry, vendor risk assessments, and threat intelligence feeds. Matt Christensen, Sr. Director GRC at Intermountain Health, highlights the complexity of this process:
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare." [1]
While healthcare-specific solutions simplify some of this integration, organizations still need to align diverse data formats and fine-tune AI models to meet their unique risk profiles. Starting small - focusing on high-impact areas like temperature-sensitive drugs, critical care supplies, implants, and networked medical devices - can help demonstrate value before expanding the system across the entire supply chain [2] [6] [10].
Alignment with U.S. Healthcare Governance
Hybrid monitoring also plays a crucial role in maintaining regulatory compliance. By continuously tracking vendor access to protected health information (PHI), monitoring vulnerabilities in medical devices, and generating detailed audit logs, these systems help organizations meet HIPAA Security Rule requirements for access control, audit trails, and data integrity [10]. Brian Sterud, CIO at Faith Regional Health, underscores the importance of benchmarking:
"Benchmarking against industry standards helps us advocate for the right resources and ensures we are leading where it matters." [1]
Looking ahead, the Healthcare & Public Health Sector Coordinating Council is preparing AI cybersecurity guidance for 2026, which will address third-party AI tools and supply chain monitoring [8]. Organizations that adopt hybrid systems now will be better equipped to meet these evolving standards. The key lies in establishing governance frameworks that regularly review AI-generated insights, prioritize remediation efforts, and ensure monitoring practices align with both federal and state regulations.
sbb-itb-535baee
Advantages and Disadvantages
Comparison of AI Monitoring Strategies in Healthcare Supply Chains
Each monitoring strategy comes with its own set of pros and cons. Let’s start with performance monitoring, which focuses on improving operational efficiency. This method can boost demand forecasting accuracy from 65% to about 85%, reduce waste by 30–40%, and maintain nearly 99% product availability [2]. On top of that, it ensures inventory accuracy of over 99%, cutting down on manual counts and lowering carrying costs. However, it’s not without its challenges. Issues like model drift, poor data quality, and over-reliance on automation can creep in if there’s no continuous validation process [2][11]. And while it’s great for operations, it doesn’t do much to detect security threats.
Switching gears to security-focused monitoring, this approach zeroes in on protecting systems from cyber risks. It aligns with emerging AI cybersecurity standards, helping organizations track third-party AI tools and address vulnerabilities in their supply chains [8]. It’s especially critical for safeguarding patient data and ensuring HIPAA compliance across vendor networks. That said, it’s not perfect. Poorly tuned systems can lead to alert fatigue, and focusing solely on security metrics can cause teams to overlook operational KPIs, like fill rates and lead times [7][4]. Smaller organizations might also struggle to keep up due to the specialized skills and budgets required.
Then there’s hybrid integrated monitoring, which combines the strengths of both operational and security-focused approaches. This method offers a unified view of operations and security, reduces manual work through automation, and can cut security alerts by up to 80% through intelligent correlation [7]. A great example is Censinet RiskOps™, which facilitates real-time sharing of cybersecurity and risk data between healthcare organizations and vendors, creating a collaborative defense network [1]. However, implementing this strategy isn’t a walk in the park. It requires integrating data from systems like EHR, ERP, warehouse management tools, and threat intelligence feeds - an effort that’s both complex and tailored to healthcare’s unique needs [1]. It also demands significant initial effort and ongoing AI model adjustments.
Here’s a quick breakdown of the key advantages and disadvantages of each approach:
| Strategy | Key Advantages | Main Disadvantages |
|---|---|---|
| Performance Monitoring | • Boosts demand forecasting accuracy (65% to ~85%) [2] • Reduces waste by 30–40% while maintaining ~99% product availability [2] • Ensures 99%+ inventory accuracy, reducing manual counts [3] • Lowers carrying costs and emergency orders |
• Prone to model drift and data quality issues without continuous validation [2][11] • Over-reliance on automation may reduce oversight [11][4] • Limited in detecting security threats |
| Security-Focused Monitoring | • Follows AI cybersecurity guidance [8] • Protects patient data and manages vendor access • Detects compromised accounts and threats • Supports HIPAA compliance |
• Can cause alert fatigue if not properly tuned [7] • Requires specialized skills and budgets • May neglect operational KPIs like fill rates and lead times [4] • Might overlook non-security performance issues |
| Hybrid Integrated Monitoring | • Delivers a unified view of operations and security • Reduces security alerts by up to 80% [7] • Automates risk assessments, cutting down manual effort [1] • Enables collaboration through vendor networks [1] • Improves regulatory alignment |
• Demands complex data integration across multiple systems [1] • Requires healthcare-specific solutions • Involves considerable initial implementation effort • Needs ongoing AI model tuning |
Choosing the right monitoring strategy depends on your organization’s specific risks, resources, and compliance needs. A smart starting point is to focus on high-priority areas - like temperature-sensitive drugs, critical care supplies, implants, and connected medical devices. This allows teams to prove the value of their approach before scaling it across the entire supply chain [2][6][10].
Conclusion
Hybrid integrated monitoring stands out as the best approach for managing U.S. healthcare supply chains. While performance-focused monitoring can achieve impressive results - such as improving forecast accuracy to about 85% and reducing waste by 30–40% [2] - it falls short in addressing critical security vulnerabilities. On the other hand, security-focused monitoring tackles cyber threats but fails to address the operational metrics that ensure smooth supply flow and cost management. A hybrid strategy combines the strengths of both, offering a unified view that safeguards patient data, ensures regulatory compliance, and enhances supply chain efficiency.
To fully leverage the advantages of hybrid monitoring, healthcare organizations need solutions tailored to their unique challenges. This starts with taking stock of all AI systems used in areas like demand planning, inventory management, logistics, and vendor portals, and then connecting these systems to clinical and business-critical outcomes [2][3]. With this groundwork in place, organizations can establish governance structures that bring together supply chain leaders, IT security teams, compliance officers, and clinical stakeholders. This collaboration helps define clear risk tolerances and set performance benchmarks.
Examples from the field highlight the effectiveness of this integrated approach. Terry Grogan, CISO at Tower Health, shared how Censinet RiskOps improved their risk assessment processes while allowing full-time employees to focus on other priorities [1]. This type of efficiency - achieving more with fewer resources while strengthening security - is a direct result of hybrid integrated monitoring, which leverages intelligent automation and collaborative risk management.
To measure success, organizations should monitor key metrics such as operational efficiency (forecast accuracy, inventory turnover, waste reduction, emergency orders), security performance (threat detection, vendor compliance, incident response), and clinical outcomes (procedure delays, clinician satisfaction, supply-related quality issues). Comparing these metrics over 12–24 months against pre-implementation baselines provides a clear picture of the operational returns and risk reduction achieved [2][3][4][9].
FAQs
How does AI enhance demand forecasting in healthcare supply chains?
AI plays a key role in improving demand forecasting within healthcare supply chains. By analyzing real-time data, it identifies patterns, predicts future needs, and streamlines inventory management. This reduces the chances of running out of essential supplies, avoids overstocking, and ensures critical items are readily available when required.
With its ability to process massive amounts of data both quickly and accurately, AI enables healthcare organizations to adapt to shifting demands, enhance operational efficiency, and maintain a dependable supply chain.
What challenges come with using AI to monitor healthcare supply chains?
Implementing AI monitoring in healthcare supply chains comes with its fair share of hurdles. One major challenge lies in integrating AI systems with existing workflows, especially when older, legacy infrastructure is involved. This process often demands significant effort to ensure seamless compatibility.
Another critical aspect is ensuring data accuracy while maintaining stringent security standards. With sensitive patient information in the mix, careful planning is essential to safeguard data and meet privacy expectations.
Healthcare regulations, like HIPAA, introduce additional complexities. Strict compliance is non-negotiable, which can make implementation even more intricate. On top of that, achieving real-time monitoring capabilities isn't just a technical feat - it requires advanced systems and resources to function effectively.
There’s also the human element to consider. Resistance to change among staff can slow down adoption. This makes training programs and clear communication vital to help teams understand and embrace the benefits of these new AI systems.
How does hybrid integrated monitoring improve efficiency and security in healthcare supply chains?
Hybrid integrated monitoring enhances operational efficiency by enabling real-time identification of supply chain risks. This reduces reliance on manual oversight and simplifies the process of assessing potential threats. The result? Faster responses to issues, keeping organizations adaptable and ahead of challenges.
From a security standpoint, this approach offers constant monitoring, early threat detection, and robust risk management. By maintaining the integrity of the supply chain, it plays a vital role in protecting patient safety and ensuring the uninterrupted delivery of essential healthcare services.


